40 results in Exploration of Asthma & Allergy
Latest
Sort by :
- Latest
- Most Viewed
- Most Downloaded
- Most Cited
Open Access
Systematic Review
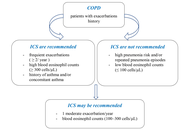
Ensuring patient safety: a closer look at glucocorticoid therapy in COPD and asthma
Alexandru Corlateanu, Cristina Toma
Published: December 22, 2025 Explor Asthma Allergy. 2025;3:1009104
This article belongs to the special issue The Era of Biologics in Allergy
Open Access
Review
Beyond the airways: asthma as a systemic disorder
Silvina Monica Alvarez ... Nidia Noemi Gomez
Published: December 11, 2025 Explor Asthma Allergy. 2025;3:1009103
This article belongs to the special issue Asthma and its Relationship with Psychological and Psychopathological Factors

Open Access
Commentary
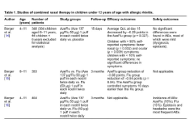
Combined intranasal treatment for allergic rhinitis: an option for children under 12 years of age
Alberto Vidal, Pedro Cortez
Published: December 01, 2025 Explor Asthma Allergy. 2025;3:1009102
This article belongs to the special issue Asthma, Allergies, and Respiratory Infections in Pediatric Age
Open Access
Original Article
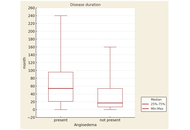
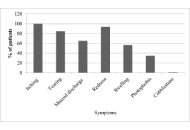
Clinical and autoimmune characteristics associated with angioedema in patients with chronic spontaneous urticaria
Vesna Trajkova ... Kristina Trpcheva Stojkov
Published: December 01, 2025 Explor Asthma Allergy. 2025;3:1009101
This article belongs to the special issue Bridging Experimental and Translational Allergology
Open Access
Case Report
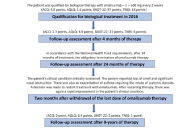
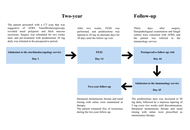
Multidimensional super-response to omalizumab in a patient with N-ERD: 9-year follow-up of a case report
Edyta Jura-Szołtys ... Radosław Gawlik
Published: November 21, 2025 Explor Asthma Allergy. 2025;3:1009100
This article belongs to the special issue Update on Chronic Rhinosinusitis
Open Access
Case Report
A rare complication in Schnitzler syndrome: recall urticaria in a patient treated with anakinra—a case report
Christian Paolo Ratti ... Silvia Mariel Ferrucci
Published: November 13, 2025 Explor Asthma Allergy. 2025;3:100999
This article belongs to the special issue The Era of Biologics in Allergy

Open Access
Review
Update on the management of eosinophilic esophagitis in adult patients
Adrianna Wierzbicka, Andrew Ukleja
Published: November 12, 2025 Explor Asthma Allergy. 2025;3:100998
This article belongs to the special issue Beyond Eosinophilic Gastrointestinal Diseases: Pathogenetic Mechanisms and Therapeutic Strategies
Open Access
Original Article
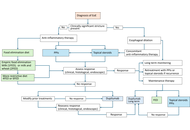
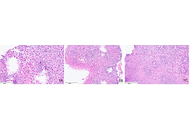
The expanding spectrum of eosinophilic gastrointestinal disorders: summarizing diagnostic challenges, updated consensus diagnostic criteria, molecular drivers and site-specific histopathological changes
Nayantrishna Nath ... Prasenjit Das
Published: November 06, 2025 Explor Asthma Allergy. 2025;3:100997
This article belongs to the special issue Beyond Eosinophilic Gastrointestinal Diseases: Pathogenetic Mechanisms and Therapeutic Strategies
Open Access
Original Article
Floral biology variations in Olea europaea over 6 years in Southern Italy: implications for allergy
Alessandro Cinquantasei ... Marcello Albanesi
Published: October 29, 2025 Explor Asthma Allergy. 2025;3:100996
This article belongs to the special issue Climate Change, Allergy, and Immunotherapy

Open Access
Original Article
Unveiling allergic conjunctivitis: the role of skin prick tests and key risk factors
Seyed Hesamedin Nabavizadeh ... Najmeh Sepahi
Published: October 20, 2025 Explor Asthma Allergy. 2025;3:100995
Open Access
Case Report
Pediatric allergic fungal rhinosinusitis: case report and literature review
Daniela de Abreu e Silva Martinez ... Priscila Novaes Ferraiolo
Published: October 14, 2025 Explor Asthma Allergy. 2025;3:100994
Open Access
Editorial
Underuse of allergen immunotherapy: a call to action
Mario Di Gioacchino ... Giorgio Walter Canonica
Published: October 10, 2025 Explor Asthma Allergy. 2025;3:100993

Open Access
Review
Artificial intelligence in clinical allergy practice: current status, challenges, and future directions
Melvin Lee Qiyu ... Qasim Malik
Published: September 25, 2025 Explor Asthma Allergy. 2025;3:100992
This article belongs to the special issue Allergy and Asthma in the Digital Age

Open Access
Review
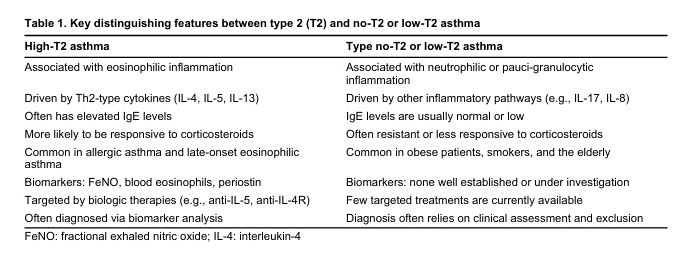
Evidence-based answers to clinical controversies in the management of severe asthma
David El-Qutob, Martin Maillo
Published: August 21, 2025 Explor Asthma Allergy. 2025;3:100991
Open Access
Original Article
A real-world clustering analysis reveals heterogeneous response patterns to biologic therapy in severe asthma
Shuichiro Matsumoto ... Hisatoshi Sugiura
Published: August 18, 2025 Explor Asthma Allergy. 2025;3:100990
This article belongs to the special issue The Era of Biologics in Allergy
Open Access
Case Report
Delayed hypersensitivity and cytokine release syndrome to paclitaxel and nab-paclitaxel: a case report
Shaonie Ton-Leclerc ... Ghislaine Isabwe
Published: August 05, 2025 Explor Asthma Allergy. 2025;3:100989
Open Access
Review
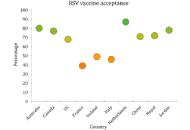
Maternal RSV vaccination to protect infants: current evidence and future directions
Malik Sallam ... Mohammed Sallam
Published: July 30, 2025 Explor Asthma Allergy. 2025;3:100988
This article belongs to the special issue Asthma, Allergies, and Respiratory Infections in Pediatric Age
Open Access
Mini Review
Climate change and allergy: a call for action in Europe
Lisa Vitry
Published: July 23, 2025 Explor Asthma Allergy. 2025;3:100987
This article belongs to the special issue Climate Change, Allergy, and Immunotherapy
Open Access
Perspective
Pollen allergy and climate change: perceptions by physicians and patients
Nhan Pham-Thi, Pascal Demoly
Published: July 07, 2025 Explor Asthma Allergy. 2025;3:100986
This article belongs to the special issue Climate Change, Allergy, and Immunotherapy
Open Access
Review
Role of air pollution in rhinitis
Dichapong Kanjanawasee ... Pongsakorn Tantilipikorn
Published: July 03, 2025 Explor Asthma Allergy. 2025;3:100985
This article belongs to the special issue Precision Medicine in Allergy and Rhinology

Journal Information
 Previous
Previous