









Aim:
To assess healthcare professionals’ awareness, attitudes, and utilization of community-based digital health platforms for preventive care in underserved districts of Khyber Pakhtunkhwa, Pakistan, and to identify key barriers associated with routine use.
Methods:
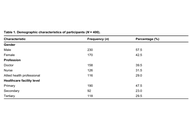
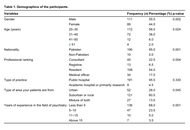
A cross-sectional survey was conducted between December 2024 and February 2025 among 400 healthcare professionals (doctors, nurses, and allied health practitioners) working in primary, secondary, and tertiary facilities in Swabi and Mardan. Participants were recruited using purposive, stratified (quota-based) sampling. The questionnaire captured knowledge/awareness, attitudes, self-reported utilization, and perceived barriers (infrastructure, training, and privacy). Descriptive statistics were produced, and multivariable regression was used to examine factors associated with utilization.
Results:
Among the 400 respondents, 332 (83.0%) reported awareness of digital health platforms and 312 (78.0%) reported positive attitudes toward their use. Overall, 297 (74.3%) reported using digital health platforms in practice. The most frequently reported barriers were lack of infrastructure (n = 309, 77.3%), limited training (n = 297, 74.3%), and data privacy concerns (n = 295, 73.8%). In the adjusted logistic regression model, greater knowledge of digital health platforms was associated with higher odds of routine use (aOR = 10.56, 95% CI: 2.36–47.35; p = 0.002), whereas attitude and infrastructure barriers were not significant (p > 0.05).
Conclusions:
Healthcare professionals in Swabi and Mardan reported high awareness and favorable attitudes toward community-based digital health platforms, but infrastructure gaps, limited training, and data privacy concerns were common barriers. Greater platform knowledge predicted routine use. Strengthening facility readiness, workflow-based training, and practical safeguards to address data privacy concerns may enable safer, more equitable scale-up; findings are context-specific due to non-probability sampling.
Aim:
To assess healthcare professionals’ awareness, attitudes, and utilization of community-based digital health platforms for preventive care in underserved districts of Khyber Pakhtunkhwa, Pakistan, and to identify key barriers associated with routine use.
Methods:
A cross-sectional survey was conducted between December 2024 and February 2025 among 400 healthcare professionals (doctors, nurses, and allied health practitioners) working in primary, secondary, and tertiary facilities in Swabi and Mardan. Participants were recruited using purposive, stratified (quota-based) sampling. The questionnaire captured knowledge/awareness, attitudes, self-reported utilization, and perceived barriers (infrastructure, training, and privacy). Descriptive statistics were produced, and multivariable regression was used to examine factors associated with utilization.
Results:
Among the 400 respondents, 332 (83.0%) reported awareness of digital health platforms and 312 (78.0%) reported positive attitudes toward their use. Overall, 297 (74.3%) reported using digital health platforms in practice. The most frequently reported barriers were lack of infrastructure (n = 309, 77.3%), limited training (n = 297, 74.3%), and data privacy concerns (n = 295, 73.8%). In the adjusted logistic regression model, greater knowledge of digital health platforms was associated with higher odds of routine use (aOR = 10.56, 95% CI: 2.36–47.35; p = 0.002), whereas attitude and infrastructure barriers were not significant (p > 0.05).
Conclusions:
Healthcare professionals in Swabi and Mardan reported high awareness and favorable attitudes toward community-based digital health platforms, but infrastructure gaps, limited training, and data privacy concerns were common barriers. Greater platform knowledge predicted routine use. Strengthening facility readiness, workflow-based training, and practical safeguards to address data privacy concerns may enable safer, more equitable scale-up; findings are context-specific due to non-probability sampling.
DOI: https://doi.org/10.37349/edht.2026.101187
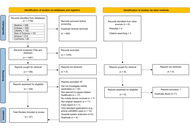
Background:
Sepsis is a major cause of disease worldwide. Mobile applications (apps) have been developed to assist clinical practice. Current evidence evaluating such apps is diverse. This scoping review aimed to map currently available literature investigating the usage of mobile apps for sepsis-related healthcare. This will highlight evidence gaps, and areas for future innovation and app development.
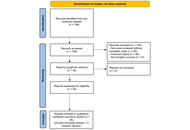
Methods:
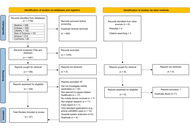
Databases MEDLINE, Embase, CINAHL, Cochrane, Scopus, and Web of Science were searched in June 2023 (updated in July 2024). Studies containing original research investigating mobile apps for sepsis-related healthcare were included and analysed in three categories identified from the primary purpose of the app: (1) education and awareness, (2) clinical assistance, and (3) biomarker or pathogen detection.
Results:
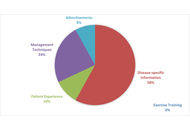
A total of 1,755 studies were identified and 27 included following screening, of which 19 (70%) were published in 2020 or later. Most of the 27 studies investigated apps for clinical assistance (70%, n = 19). These apps were diverse, acting as digital solutions for data collection (n = 2), triage (n = 6), clinical guideline access (n = 5), alert delivery (n = 1), and outcome prediction (n = 5). There were five apps (19%) used to assist biomarker or pathogen detection. Of these, most (80%, n = 4) mobile apps were used to detect and quantify colorimetric signals in combination with assays, and all five apps had attachments necessary for laboratory processes. Lastly, three apps (11%) were designed to enhance education and awareness, two targeting medical education and one targeting public awareness.
Discussion:
Mobile applications offer innovative and exciting digital solutions for biomarker detection, education, and clinical support in sepsis-related healthcare. Current literature is highly heterogenous and rapidly developing.
Background:
Sepsis is a major cause of disease worldwide. Mobile applications (apps) have been developed to assist clinical practice. Current evidence evaluating such apps is diverse. This scoping review aimed to map currently available literature investigating the usage of mobile apps for sepsis-related healthcare. This will highlight evidence gaps, and areas for future innovation and app development.
Methods:
Databases MEDLINE, Embase, CINAHL, Cochrane, Scopus, and Web of Science were searched in June 2023 (updated in July 2024). Studies containing original research investigating mobile apps for sepsis-related healthcare were included and analysed in three categories identified from the primary purpose of the app: (1) education and awareness, (2) clinical assistance, and (3) biomarker or pathogen detection.
Results:
A total of 1,755 studies were identified and 27 included following screening, of which 19 (70%) were published in 2020 or later. Most of the 27 studies investigated apps for clinical assistance (70%, n = 19). These apps were diverse, acting as digital solutions for data collection (n = 2), triage (n = 6), clinical guideline access (n = 5), alert delivery (n = 1), and outcome prediction (n = 5). There were five apps (19%) used to assist biomarker or pathogen detection. Of these, most (80%, n = 4) mobile apps were used to detect and quantify colorimetric signals in combination with assays, and all five apps had attachments necessary for laboratory processes. Lastly, three apps (11%) were designed to enhance education and awareness, two targeting medical education and one targeting public awareness.
Discussion:
Mobile applications offer innovative and exciting digital solutions for biomarker detection, education, and clinical support in sepsis-related healthcare. Current literature is highly heterogenous and rapidly developing.
DOI: https://doi.org/10.37349/edht.2026.101186

Multicenter imaging studies are increasingly critical in epidemiology, yet variability across scanners, acquisition protocols, and reconstruction algorithms introduces systematic biases that threaten reproducibility and comparability of quantitative biomarkers. This paper reviews the major sources of heterogeneity in MRI, CT, and PET-CT data, highlighting their impact on epidemiologic inference, including misclassification, reduced statistical power, and compromised generalizability. We outline harmonization strategies spanning pre-acquisition standardization, phantom-based calibration, post-acquisition intensity normalization, and advanced statistical and machine learning methods such as ComBat and domain adaptation. Illustrative examples from MRI flow quantification and radiomic feature extraction demonstrate how harmonization can mitigate site effects and enable robust large-scale analyses.
Multicenter imaging studies are increasingly critical in epidemiology, yet variability across scanners, acquisition protocols, and reconstruction algorithms introduces systematic biases that threaten reproducibility and comparability of quantitative biomarkers. This paper reviews the major sources of heterogeneity in MRI, CT, and PET-CT data, highlighting their impact on epidemiologic inference, including misclassification, reduced statistical power, and compromised generalizability. We outline harmonization strategies spanning pre-acquisition standardization, phantom-based calibration, post-acquisition intensity normalization, and advanced statistical and machine learning methods such as ComBat and domain adaptation. Illustrative examples from MRI flow quantification and radiomic feature extraction demonstrate how harmonization can mitigate site effects and enable robust large-scale analyses.
DOI: https://doi.org/10.37349/edht.2026.101185
Aim:
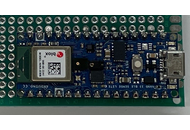
Neonatal jaundice or neonatal hyperbilirubinemia is a common medical condition impacting newborns and pathological jaundice if left untreated, leads to neurological encephalopathy and/or death. The majority of pathological jaundice cases occur in low and middle- income countries (LMIC). Phototherapy has been determined to be the safest and most effective treatment for jaundice. Although inexpensive light-emitting diodes are available on the market, commercial phototherapy devices are expensive (~US$2,000), which creates a barrier to access for these devices in LMIC. Efforts to construct cost-effective phototherapy units have been implemented in the past, but need a method to validate the intensity and wavelength of light received by the infant at a distance away from the source.
Methods:
To enable low-cost phototherapy units to be used clinically, this study provides an open-source, low-cost, distributed manufacturing approach to create a light sensor to calibrate phototherapy units. This instrument is a necessary component of any open-source phototherapy treatment used in a clinical setting. This novel instrument was validated by comparing its irradiance and wavelength reading to the commercially calibrated Ocean Insight UV-VIS spectrometer under varying lighting conditions, including that of the existing Datex-Ohmeda Giraffe Spot PT Lite phototherapy equipment accessible through Victoria Children’s Hospital Neonatal Care Ward in London, Ontario, and Kiambu County Hospital in Kenya.
Results:
The results of this study have demonstrated that for under US$150, a phototherapy calibration device can be constructed capable of measuring up to 200 uW/cm2/nm with an accuracy of 98.6% and detect the peak wavelength within ±12.5 nm.
Conclusions:
It can be concluded that 3D printed open-source irradiance meters are a viable option for calibrating phototherapy units in LMIC to treat hyperbilirubinemia.
Aim:
Neonatal jaundice or neonatal hyperbilirubinemia is a common medical condition impacting newborns and pathological jaundice if left untreated, leads to neurological encephalopathy and/or death. The majority of pathological jaundice cases occur in low and middle- income countries (LMIC). Phototherapy has been determined to be the safest and most effective treatment for jaundice. Although inexpensive light-emitting diodes are available on the market, commercial phototherapy devices are expensive (~US$2,000), which creates a barrier to access for these devices in LMIC. Efforts to construct cost-effective phototherapy units have been implemented in the past, but need a method to validate the intensity and wavelength of light received by the infant at a distance away from the source.
Methods:
To enable low-cost phototherapy units to be used clinically, this study provides an open-source, low-cost, distributed manufacturing approach to create a light sensor to calibrate phototherapy units. This instrument is a necessary component of any open-source phototherapy treatment used in a clinical setting. This novel instrument was validated by comparing its irradiance and wavelength reading to the commercially calibrated Ocean Insight UV-VIS spectrometer under varying lighting conditions, including that of the existing Datex-Ohmeda Giraffe Spot PT Lite phototherapy equipment accessible through Victoria Children’s Hospital Neonatal Care Ward in London, Ontario, and Kiambu County Hospital in Kenya.
Results:
The results of this study have demonstrated that for under US$150, a phototherapy calibration device can be constructed capable of measuring up to 200 uW/cm2/nm with an accuracy of 98.6% and detect the peak wavelength within ±12.5 nm.
Conclusions:
It can be concluded that 3D printed open-source irradiance meters are a viable option for calibrating phototherapy units in LMIC to treat hyperbilirubinemia.
DOI: https://doi.org/10.37349/edht.2026.101184

Aim:
This study aims to evaluate the outreach achieved by psychiatry-related posts using the hashtag #YouthMentalHealth, highlighting how social media platforms can shape public discourse on adolescent mental health.
Methods:
We utilized the Fedica research analytics tool to characterize posts containing #YouthMentalHealth from January 10, 2018, to January 10, 2023. This analysis examined the #YouthMentalHealth activity timeline, identifying the number of posts containing the hashtag and the geographical distribution to assess the effectiveness of hashtag campaigns.
Results:
The #YouthMentalHealth movement resulted in 58,000 posts shared by around 25,000 X users, generating 292.7 million impressions (views). The top three countries from which most posts containing #YouthMentalHealth were shared included the United States (35.14%), Canada (29.15%), and the United Kingdom (14.37%). The three largest contributor groups were management companies (20.6%), educational advocacy organizations (17.5%), and social advocacy groups (14%).
Conclusions:
This first-of-its-kind study explores the impact and utilization of #YouthMentalHealth globally, reporting trends and patterns from digital media platforms. By mapping the hashtag’s global footprint, the study offers novel insights into how digital advocacy can amplify youth mental health awareness and connect multidisciplinary stakeholders. These findings contribute to emerging frameworks in digital psychiatry by underscoring the role of social media as a complementary tool for mental health promotion and community engagement, while illuminating diverse strategies to aid the psychiatric community in effectively addressing the mental health needs of adolescents.
Aim:
This study aims to evaluate the outreach achieved by psychiatry-related posts using the hashtag #YouthMentalHealth, highlighting how social media platforms can shape public discourse on adolescent mental health.
Methods:
We utilized the Fedica research analytics tool to characterize posts containing #YouthMentalHealth from January 10, 2018, to January 10, 2023. This analysis examined the #YouthMentalHealth activity timeline, identifying the number of posts containing the hashtag and the geographical distribution to assess the effectiveness of hashtag campaigns.
Results:
The #YouthMentalHealth movement resulted in 58,000 posts shared by around 25,000 X users, generating 292.7 million impressions (views). The top three countries from which most posts containing #YouthMentalHealth were shared included the United States (35.14%), Canada (29.15%), and the United Kingdom (14.37%). The three largest contributor groups were management companies (20.6%), educational advocacy organizations (17.5%), and social advocacy groups (14%).
Conclusions:
This first-of-its-kind study explores the impact and utilization of #YouthMentalHealth globally, reporting trends and patterns from digital media platforms. By mapping the hashtag’s global footprint, the study offers novel insights into how digital advocacy can amplify youth mental health awareness and connect multidisciplinary stakeholders. These findings contribute to emerging frameworks in digital psychiatry by underscoring the role of social media as a complementary tool for mental health promotion and community engagement, while illuminating diverse strategies to aid the psychiatric community in effectively addressing the mental health needs of adolescents.
DOI: https://doi.org/10.37349/edht.2026.101183
Background:
To synthesize evidence on how medical thermography, integrated with artificial intelligence (AI), blockchain, 5G (5th Generation mobile networks), and Internet of Things (IoT), enhances diagnostics, fraud prevention, and personalized health insurance in emerging markets, addressing cost escalation and access gaps.
Methods:
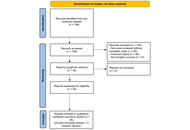
This systematic review followed AMSTAR 2 and PRISMA guidelines, synthesizing 25 sources (22 peer-reviewed articles, 3 industry reports) from a pre-analyzed dataset. Inclusion focused on relevance to thermography, insurance, or synergistic technologies; exclusions included non-peer-reviewed or irrelevant items. Data extraction via Microsoft Excel (version 2409) covered diagnostics, applications, synergies, and contexts. Quality appraisal used the Mixed Methods Appraisal Tool (MMAT) to assess methodological rigor. Narrative synthesis addressed heterogeneity, without meta-analysis due to design diversity and resource limits.
Results:
Thermography achieves 83–98% sensitivities for breast cancer (asymmetries > 3.0°C), diabetic foot ulcers (DFUs; 96.71% with AI), and rheumatoid arthritis (RA; inflammation > 0.5°C), reducing triage times by 25% and costs by 30% in mobile settings. Blockchain’s six-layer architecture, with Practical Byzantine Fault Tolerance and InterPlanetary File System, secures data at US$0.028 per transaction, potentially reducing fraud through enhanced verification. In emerging markets like India and Brazil, portable thermography with 5G supports screening, aligned with standards like T/ZADT 005-2002.
Discussion:
These integrations enable early detection (saving US$8,000–12,000 per DFU), fraud mitigation, and equitable access, though protocol variances and biases require attention. Recommendations include standardization, pilots in rural areas, and bias-mitigating AI frameworks to optimize health insurance outcomes.
Background:
To synthesize evidence on how medical thermography, integrated with artificial intelligence (AI), blockchain, 5G (5th Generation mobile networks), and Internet of Things (IoT), enhances diagnostics, fraud prevention, and personalized health insurance in emerging markets, addressing cost escalation and access gaps.
Methods:
This systematic review followed AMSTAR 2 and PRISMA guidelines, synthesizing 25 sources (22 peer-reviewed articles, 3 industry reports) from a pre-analyzed dataset. Inclusion focused on relevance to thermography, insurance, or synergistic technologies; exclusions included non-peer-reviewed or irrelevant items. Data extraction via Microsoft Excel (version 2409) covered diagnostics, applications, synergies, and contexts. Quality appraisal used the Mixed Methods Appraisal Tool (MMAT) to assess methodological rigor. Narrative synthesis addressed heterogeneity, without meta-analysis due to design diversity and resource limits.
Results:
Thermography achieves 83–98% sensitivities for breast cancer (asymmetries > 3.0°C), diabetic foot ulcers (DFUs; 96.71% with AI), and rheumatoid arthritis (RA; inflammation > 0.5°C), reducing triage times by 25% and costs by 30% in mobile settings. Blockchain’s six-layer architecture, with Practical Byzantine Fault Tolerance and InterPlanetary File System, secures data at US$0.028 per transaction, potentially reducing fraud through enhanced verification. In emerging markets like India and Brazil, portable thermography with 5G supports screening, aligned with standards like T/ZADT 005-2002.
Discussion:
These integrations enable early detection (saving US$8,000–12,000 per DFU), fraud mitigation, and equitable access, though protocol variances and biases require attention. Recommendations include standardization, pilots in rural areas, and bias-mitigating AI frameworks to optimize health insurance outcomes.
DOI: https://doi.org/10.37349/edht.2026.101182

Digital twin technology is emerging as a transformative paradigm in healthcare, shifting practice from provider-centered models toward more personalized forms of medicine. As dynamic virtual representations of the human body, digital twins integrate biometric data, lifestyle patterns, and clinical records to simulate, monitor, and predict health trajectories in real time. Their growing use raises not only technical possibilities but also important questions about how patients relate to these data-driven counterparts, particularly when twins inform everyday health decisions in chronic care, such as diabetes or oncology. This perspective examines these relational dynamics and their ethical, cultural, and experiential implications for autonomy, decision-making, and the lived experience of being represented in data. To guide this analysis, we introduce a scale framework with three intersecting lenses: time, distinguishing asynchronous from synchronous updating; twining, ranging from close mirroring to more augmentative forms of representation; and control, spanning human-led to twin-driven decision authority. Using this framework, we position four common types of digital twins: mirror, shadow, intelligent, and simulacra as an evolution from basic representation to transformative modeling. We argue that future healthcare and public health policy must go beyond technical innovation to address patients’ lived experiences, ensuring that digital twins enhance rather than diminish autonomy, trust, and equity. This perspective thus calls for a patient-centered approach in designing and implementing digital twin technologies.
Digital twin technology is emerging as a transformative paradigm in healthcare, shifting practice from provider-centered models toward more personalized forms of medicine. As dynamic virtual representations of the human body, digital twins integrate biometric data, lifestyle patterns, and clinical records to simulate, monitor, and predict health trajectories in real time. Their growing use raises not only technical possibilities but also important questions about how patients relate to these data-driven counterparts, particularly when twins inform everyday health decisions in chronic care, such as diabetes or oncology. This perspective examines these relational dynamics and their ethical, cultural, and experiential implications for autonomy, decision-making, and the lived experience of being represented in data. To guide this analysis, we introduce a scale framework with three intersecting lenses: time, distinguishing asynchronous from synchronous updating; twining, ranging from close mirroring to more augmentative forms of representation; and control, spanning human-led to twin-driven decision authority. Using this framework, we position four common types of digital twins: mirror, shadow, intelligent, and simulacra as an evolution from basic representation to transformative modeling. We argue that future healthcare and public health policy must go beyond technical innovation to address patients’ lived experiences, ensuring that digital twins enhance rather than diminish autonomy, trust, and equity. This perspective thus calls for a patient-centered approach in designing and implementing digital twin technologies.
DOI: https://doi.org/10.37349/edht.2026.101181

Aim:
Diagnosing and treating major depressive disorder (MDD) remains a pressing global health challenge. Generative-AI tools, by lowering technical barriers and offering rapid visual feedback, may open new avenues for art-based assessment and intervention.
Methods:
In this exploratory qualitative pilot, we conducted reflexive thematic analysis of semi-structured interviews with N = 10 young adults at elevated risk for depression who generated self-representative images in Midjourney during a 45-minute session. Participants were selected from a larger cohort described elsewhere; no quantitative analyses were conducted in the present paper.
Results:
Qualitative findings suggested therapeutic-like mechanisms that mirror—and in some cases amplify—those reported for traditional art therapy, including the experience of flow and spontaneity, a heightened sense of creative agency, and the safe externalization of difficult or extreme emotions. Some participants described abrupt “sentiment switches,” where joyful imagery was immediately followed by scenes of sudden, intrusive self-criticism. Importantly, the generative process also surfaced idiosyncratic “resource images” (e.g., nature motifs, hobbies, values, loved ones) that participants experienced as calming or empowering, hinting at personalised anchors for future interventions.
Conclusions:
In line with prior quantitative work showing that more negative prompt sentiment statistically relates to higher BDI scores, the present qualitative narratives offer an interpretive account of how such negativity may emerge during AI-assisted self-representation. However, the current study does not integrate datasets or perform mixed-methods triangulation and uses those prior findings solely for contextualization. We conclude that, with appropriate ethical safeguards, generative-AI image making may serve as a flexible, low-cost adjunct to existing diagnostic and art-therapeutic practices, offering clients and clinicians a shared visual language for exploring the multi-layered experience of depression.
Aim:
Diagnosing and treating major depressive disorder (MDD) remains a pressing global health challenge. Generative-AI tools, by lowering technical barriers and offering rapid visual feedback, may open new avenues for art-based assessment and intervention.
Methods:
In this exploratory qualitative pilot, we conducted reflexive thematic analysis of semi-structured interviews with N = 10 young adults at elevated risk for depression who generated self-representative images in Midjourney during a 45-minute session. Participants were selected from a larger cohort described elsewhere; no quantitative analyses were conducted in the present paper.
Results:
Qualitative findings suggested therapeutic-like mechanisms that mirror—and in some cases amplify—those reported for traditional art therapy, including the experience of flow and spontaneity, a heightened sense of creative agency, and the safe externalization of difficult or extreme emotions. Some participants described abrupt “sentiment switches,” where joyful imagery was immediately followed by scenes of sudden, intrusive self-criticism. Importantly, the generative process also surfaced idiosyncratic “resource images” (e.g., nature motifs, hobbies, values, loved ones) that participants experienced as calming or empowering, hinting at personalised anchors for future interventions.
Conclusions:
In line with prior quantitative work showing that more negative prompt sentiment statistically relates to higher BDI scores, the present qualitative narratives offer an interpretive account of how such negativity may emerge during AI-assisted self-representation. However, the current study does not integrate datasets or perform mixed-methods triangulation and uses those prior findings solely for contextualization. We conclude that, with appropriate ethical safeguards, generative-AI image making may serve as a flexible, low-cost adjunct to existing diagnostic and art-therapeutic practices, offering clients and clinicians a shared visual language for exploring the multi-layered experience of depression.
DOI: https://doi.org/10.37349/edht.2026.101180
This article belongs to the special issue Digital Health Innovations in the Battle Against Psychological Problems: Progress, Hurdles, and Prospects
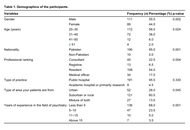
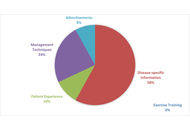
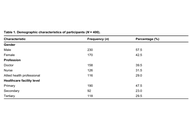
Aim:
A comprehensive understanding of current digital literacy and perspectives of the psychiatric workforce is important to introduce appropriate digital psychiatry interventions and implement contextually relevant measures in Pakistan. This study aims to address a gap in the existing literature by assessing psychiatrists’ knowledge, attitudes, perceived barriers, and willingness to integrate digital psychiatry into their clinical practice.
Methods:
A cross-sectional online survey was conducted from January 2023 to June 2023 across psychiatric departments of 18 public hospitals in Pakistan. The study included psychiatry residents, fellows, and consultants. A 48-item questionnaire, internally and externally validated, assessed knowledge, perceptions, and willingness to adopt digital psychiatry tools—telepsychiatry, artificial intelligence, mental health applications, and virtual reality. Data were analyzed using Statistical Package for the Social Sciences (version 26) for descriptive statistics, correlation, and regression analyses, while thematic analysis of open-ended responses was performed using Quirkos.
Results:
A total of 200 participants (56.0% aged 20–30 years, n = 112; 55.5% male, n = 111) were part of this study. 68.5% (n = 137) understood the applications of telepsychiatry, while 72.5% (n = 145) agreed that it is time-efficient and cost-effective. Only 39.5% (n = 79) of participants had received relevant artificial intelligence training to incorporate it in their psychiatric clinical practice. 62.0% (n = 124) of respondents reported unfamiliarity with the use of mental health applications. Regarding virtual reality, 32.5% (n = 65) were familiar with the technology, but only 42.5% (n = 85) were aware of its applications in psychiatric care. Thematic reflexive analysis revealed major challenges, including a ‘lack of infrastructure/resources’ (44.5%, n = 89) and a ‘lack of education/awareness’ (21.5%, n = 43).
Conclusions:
This study represents the first cross-sectional examination of digital psychiatric literacy in Pakistan’s healthcare system, which revealed significant gaps in digital health competencies among psychiatrists. Given the vast potential of emerging technologies in addressing mental health challenges, there is an urgent need for mental health professionals in Pakistan to integrate digitization in psychiatric practice.
Aim:
A comprehensive understanding of current digital literacy and perspectives of the psychiatric workforce is important to introduce appropriate digital psychiatry interventions and implement contextually relevant measures in Pakistan. This study aims to address a gap in the existing literature by assessing psychiatrists’ knowledge, attitudes, perceived barriers, and willingness to integrate digital psychiatry into their clinical practice.
Methods:
A cross-sectional online survey was conducted from January 2023 to June 2023 across psychiatric departments of 18 public hospitals in Pakistan. The study included psychiatry residents, fellows, and consultants. A 48-item questionnaire, internally and externally validated, assessed knowledge, perceptions, and willingness to adopt digital psychiatry tools—telepsychiatry, artificial intelligence, mental health applications, and virtual reality. Data were analyzed using Statistical Package for the Social Sciences (version 26) for descriptive statistics, correlation, and regression analyses, while thematic analysis of open-ended responses was performed using Quirkos.
Results:
A total of 200 participants (56.0% aged 20–30 years, n = 112; 55.5% male, n = 111) were part of this study. 68.5% (n = 137) understood the applications of telepsychiatry, while 72.5% (n = 145) agreed that it is time-efficient and cost-effective. Only 39.5% (n = 79) of participants had received relevant artificial intelligence training to incorporate it in their psychiatric clinical practice. 62.0% (n = 124) of respondents reported unfamiliarity with the use of mental health applications. Regarding virtual reality, 32.5% (n = 65) were familiar with the technology, but only 42.5% (n = 85) were aware of its applications in psychiatric care. Thematic reflexive analysis revealed major challenges, including a ‘lack of infrastructure/resources’ (44.5%, n = 89) and a ‘lack of education/awareness’ (21.5%, n = 43).
Conclusions:
This study represents the first cross-sectional examination of digital psychiatric literacy in Pakistan’s healthcare system, which revealed significant gaps in digital health competencies among psychiatrists. Given the vast potential of emerging technologies in addressing mental health challenges, there is an urgent need for mental health professionals in Pakistan to integrate digitization in psychiatric practice.
DOI: https://doi.org/10.37349/edht.2026.101179
This article belongs to the special issue Telepsychiatry in Low-and Middle-income Countries: an Update

Artificial intelligence (AI) is transforming healthcare by equipping clinicians and patients with tools that support more efficient, patient-centered care. In pediatrics, however, the implementation of AI demands a higher threshold for responsibility, transparency, and family-centered engagement. This perspective explores the opportunities and challenges of AI in pediatric healthcare, highlighting the unique ethical and developmental considerations that distinguish children’s care from adult medicine. Drawing on Kaiser Permanente’s seven principles for responsible AI, the article emphasizes the importance of augmentation over automation, the need for pediatric-specific validation, and the necessity of trustworthiness and fairness in clinical deployment. It outlines how AI can support primary care providers through enhanced decision support, early screening for developmental and behavioral disorders, including the potential for AI to create personalized developmental trajectories, moving beyond static population norms to provide earlier, more precise insights into a child’s neurodevelopmental progress, improved electronic health record usability, and risk prediction models. However, without careful governance, AI poses risks of bias, inequity, and erosion of clinician judgment. Policy recommendations include redesigning family consent models, ensuring robust clinician training, and mandating pediatric-specific testing of AI systems with diverse, representative datasets. Ultimately, AI should function as a supportive tool that strengthens, not replaces, human empathy, clinical expertise, and family-centered values. Responsible innovation is essential to ensure that children benefit equitably from AI while maintaining trust, safety, and compassion in pediatric healthcare.
Artificial intelligence (AI) is transforming healthcare by equipping clinicians and patients with tools that support more efficient, patient-centered care. In pediatrics, however, the implementation of AI demands a higher threshold for responsibility, transparency, and family-centered engagement. This perspective explores the opportunities and challenges of AI in pediatric healthcare, highlighting the unique ethical and developmental considerations that distinguish children’s care from adult medicine. Drawing on Kaiser Permanente’s seven principles for responsible AI, the article emphasizes the importance of augmentation over automation, the need for pediatric-specific validation, and the necessity of trustworthiness and fairness in clinical deployment. It outlines how AI can support primary care providers through enhanced decision support, early screening for developmental and behavioral disorders, including the potential for AI to create personalized developmental trajectories, moving beyond static population norms to provide earlier, more precise insights into a child’s neurodevelopmental progress, improved electronic health record usability, and risk prediction models. However, without careful governance, AI poses risks of bias, inequity, and erosion of clinician judgment. Policy recommendations include redesigning family consent models, ensuring robust clinician training, and mandating pediatric-specific testing of AI systems with diverse, representative datasets. Ultimately, AI should function as a supportive tool that strengthens, not replaces, human empathy, clinical expertise, and family-centered values. Responsible innovation is essential to ensure that children benefit equitably from AI while maintaining trust, safety, and compassion in pediatric healthcare.
DOI: https://doi.org/10.37349/edht.2026.101178
This article belongs to the special issue Expert Opinions on Digital Health Innovations
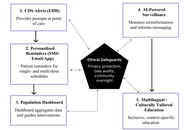
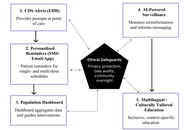
Vaccines have eliminated once-deadly diseases, yet rising vaccine hesitancy threatens these gains. Human papillomavirus (HPV) illustrates this crisis: Although it is one of the few vaccines that directly prevents cancer, uptake remains low in the United States and globally, particularly in regions with high cervical cancer incidence. This persistent gap undermines both individual and public health. This paper examines how digital health technologies, aligned with policy frameworks and community engagement, can address HPV vaccine hesitancy. We propose the Digital Vaccine Advocacy Toolkit, a structured, HPV-focused framework that integrates electronic health record (EHR)-based clinical decision support, personalized reminders, population dashboards, AI-driven misinformation surveillance, and culturally tailored education. As a conceptual model, it draws on secondary evidence and policy recommendations rather than original empirical data, emphasizing interoperability, privacy safeguards, equity-driven design, and stakeholder engagement to support feasibility across diverse health systems. The Toolkit is organized into illustrative workflows that demonstrate how technical features could be combined with policy mechanisms and financing models to strengthen HPV vaccination. By situating HPV within the World Health Organization’s 90-70-90 elimination targets and the recent adoption of single-dose schedules, the framework highlights both translational relevance and global applicability, though its recommendations require pilot testing and empirical validation. Overall, the Digital Vaccine Advocacy Toolkit offers a practical roadmap for improving HPV vaccine uptake through the integration of technology, policy, and ethics, and provides a transferable model for advancing digital health strategies to increase vaccine confidence and equity in immunization programs worldwide.
Vaccines have eliminated once-deadly diseases, yet rising vaccine hesitancy threatens these gains. Human papillomavirus (HPV) illustrates this crisis: Although it is one of the few vaccines that directly prevents cancer, uptake remains low in the United States and globally, particularly in regions with high cervical cancer incidence. This persistent gap undermines both individual and public health. This paper examines how digital health technologies, aligned with policy frameworks and community engagement, can address HPV vaccine hesitancy. We propose the Digital Vaccine Advocacy Toolkit, a structured, HPV-focused framework that integrates electronic health record (EHR)-based clinical decision support, personalized reminders, population dashboards, AI-driven misinformation surveillance, and culturally tailored education. As a conceptual model, it draws on secondary evidence and policy recommendations rather than original empirical data, emphasizing interoperability, privacy safeguards, equity-driven design, and stakeholder engagement to support feasibility across diverse health systems. The Toolkit is organized into illustrative workflows that demonstrate how technical features could be combined with policy mechanisms and financing models to strengthen HPV vaccination. By situating HPV within the World Health Organization’s 90-70-90 elimination targets and the recent adoption of single-dose schedules, the framework highlights both translational relevance and global applicability, though its recommendations require pilot testing and empirical validation. Overall, the Digital Vaccine Advocacy Toolkit offers a practical roadmap for improving HPV vaccine uptake through the integration of technology, policy, and ethics, and provides a transferable model for advancing digital health strategies to increase vaccine confidence and equity in immunization programs worldwide.
DOI: https://doi.org/10.37349/edht.2026.101177
Aim:
The aim of this study is to compare the accuracy, reliability, and educational quality of YouTube videos on osteochondritis dissecans based on their YouTube Health verification status.
Methods:
The term “osteochondritis dissecans” was searched on June 3, 2024. The first 50 videos found on YouTube after searching “osteochondritis dissecans” were evaluated. The Journal of the American Medical Association (JAMA) benchmark criteria was used to score video reliability and accuracy (0–4 points), the Global Quality Score (GQS) was used to score nonspecific educational content (0–5 points), and the osteochondritis dissecans specific score (OCDSS) was used to score specific educational content (0–11 points). Three independent reviewers scored all videos, and interrater reliability was assessed with intraclass correlation coefficients (ICC). Group differences were analyzed with one-way analysis of variance (ANOVA) and independent sample t-tests, and multivariable linear regression was used to identify independent predictors of JAMA, GQS, and OCDSS scores.
Results:
A total of 50 videos were analyzed with a cumulative 326,851 views. The mean JAMA score was 2.28 ± 0.64, the mean GQS score was 2.60 ± 1.36, and the mean OCDSS was 5.02 ± 3.16. The mean JAMA score for YouTube Health verified videos was 2.44 ± 0.34, GQS was 2.72 ± 1.22, and OCDSS was 5.72 ± 2.69. The mean JAMA score for videos not verified by YouTube Health was 2.29 ± 0.65, GQS score was 2.61 ± 1.44, and OCDSS was 4.95 ± 3.37. These differences were not statistically significant: JAMA p = 0.380, GQS p = 0.837, OCDSS p = 0.546.
Conclusions:
There were no significant differences in reliability, educational content, and comprehensiveness between videos that were verified by YouTube Health and videos that were not verified.
Aim:
The aim of this study is to compare the accuracy, reliability, and educational quality of YouTube videos on osteochondritis dissecans based on their YouTube Health verification status.
Methods:
The term “osteochondritis dissecans” was searched on June 3, 2024. The first 50 videos found on YouTube after searching “osteochondritis dissecans” were evaluated. The Journal of the American Medical Association (JAMA) benchmark criteria was used to score video reliability and accuracy (0–4 points), the Global Quality Score (GQS) was used to score nonspecific educational content (0–5 points), and the osteochondritis dissecans specific score (OCDSS) was used to score specific educational content (0–11 points). Three independent reviewers scored all videos, and interrater reliability was assessed with intraclass correlation coefficients (ICC). Group differences were analyzed with one-way analysis of variance (ANOVA) and independent sample t-tests, and multivariable linear regression was used to identify independent predictors of JAMA, GQS, and OCDSS scores.
Results:
A total of 50 videos were analyzed with a cumulative 326,851 views. The mean JAMA score was 2.28 ± 0.64, the mean GQS score was 2.60 ± 1.36, and the mean OCDSS was 5.02 ± 3.16. The mean JAMA score for YouTube Health verified videos was 2.44 ± 0.34, GQS was 2.72 ± 1.22, and OCDSS was 5.72 ± 2.69. The mean JAMA score for videos not verified by YouTube Health was 2.29 ± 0.65, GQS score was 2.61 ± 1.44, and OCDSS was 4.95 ± 3.37. These differences were not statistically significant: JAMA p = 0.380, GQS p = 0.837, OCDSS p = 0.546.
Conclusions:
There were no significant differences in reliability, educational content, and comprehensiveness between videos that were verified by YouTube Health and videos that were not verified.
DOI: https://doi.org/10.37349/edht.2026.101176

Aim:
Patients diagnosed with irregular astigmatism often require specific methods of vision correction. Among these, the use of a rigid gas permeable (RGP) lens is considered one of the most effective treatment approaches. This study aims to propose a new automated method for accurate RGP lens base-curve detection.
Methods:
A multi-modal feature fusion approach was developed based on Pentacam images, incorporating image processing and machine learning techniques. Four types of features were extracted from the images and integrated through a serial feature fusion mechanism. The fused features were then evaluated using a multi-layered perceptron (MLP) network. Specifically, the features included: (1) middle-layer outputs of a convolutional autoencoder (CAE) applied to RGB map combinations; (2) ratios of colored areas in the front cornea map; (3) a feature vector from cornea front parameters; and (4) the radius of the reference sphere/ellipse in the front elevation map.
Results:
Evaluations were performed on a manually labeled dataset. The proposed method achieved a mean squared error (MSE) of 0.005 and a coefficient of determination of 0.79, demonstrating improved accuracy compared to existing techniques.
Conclusions:
The proposed multi-modal feature fusion technique provides a reliable and accurate solution for RGP lens base-curve detection. This approach reduces manual intervention in lens fitting and represents a significant step toward automated base-curve determination.
Aim:
Patients diagnosed with irregular astigmatism often require specific methods of vision correction. Among these, the use of a rigid gas permeable (RGP) lens is considered one of the most effective treatment approaches. This study aims to propose a new automated method for accurate RGP lens base-curve detection.
Methods:
A multi-modal feature fusion approach was developed based on Pentacam images, incorporating image processing and machine learning techniques. Four types of features were extracted from the images and integrated through a serial feature fusion mechanism. The fused features were then evaluated using a multi-layered perceptron (MLP) network. Specifically, the features included: (1) middle-layer outputs of a convolutional autoencoder (CAE) applied to RGB map combinations; (2) ratios of colored areas in the front cornea map; (3) a feature vector from cornea front parameters; and (4) the radius of the reference sphere/ellipse in the front elevation map.
Results:
Evaluations were performed on a manually labeled dataset. The proposed method achieved a mean squared error (MSE) of 0.005 and a coefficient of determination of 0.79, demonstrating improved accuracy compared to existing techniques.
Conclusions:
The proposed multi-modal feature fusion technique provides a reliable and accurate solution for RGP lens base-curve detection. This approach reduces manual intervention in lens fitting and represents a significant step toward automated base-curve determination.
DOI: https://doi.org/10.37349/edht.2025.101175
This article belongs to the special issue Deep Learning Methods and Applications for Biomedical Imaging
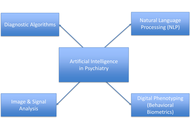
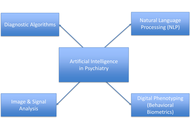
The integration of artificial intelligence (AI) into psychiatric care is rapidly revolutionizing diagnosis, risk stratification, therapy customization, and the delivery of mental health services. This narrative review synthesized recent research on ethical issues, methodological challenges, and practical applications of AI in psychiatry. A comprehensive literature search was conducted with no limitation to publication year using PubMed, Scopus, Web of Science, and Google Scholar to identify peer-reviewed articles and grey literature related to the integration of AI in psychiatry. AI enhances early identification, predicts relapses and treatment resistance, and facilitates precision pharmacopsychiatry by leveraging data from machine learning, natural language processing, digital phenotyping, and multimodal data integration. This review highlights the advancements in the integration of AI in psychiatric care, such as chatbot-mediated psychotherapy, reinforcement learning for clinical decision-making, and AI-driven triage systems in resource-constrained environments. However, there are still serious concerns about data privacy, algorithmic bias, informed consent, and the interpretability of AI systems. Other barriers to fair and safe implementation include discrepancies in training datasets, underrepresentation of marginalized groups, and a lack of clinician preparedness. There is a need for transparent, explainable, and ethically regulated AI systems that enhance, rather than replace, human decision-making. A hybrid human-AI approach to psychiatry is recommended to address these limitations, while interdisciplinary studies, strong validation frameworks, and inclusive policymaking are needed to guarantee that AI-enhanced mental health treatment continues to be effective, fair, and reliable.
The integration of artificial intelligence (AI) into psychiatric care is rapidly revolutionizing diagnosis, risk stratification, therapy customization, and the delivery of mental health services. This narrative review synthesized recent research on ethical issues, methodological challenges, and practical applications of AI in psychiatry. A comprehensive literature search was conducted with no limitation to publication year using PubMed, Scopus, Web of Science, and Google Scholar to identify peer-reviewed articles and grey literature related to the integration of AI in psychiatry. AI enhances early identification, predicts relapses and treatment resistance, and facilitates precision pharmacopsychiatry by leveraging data from machine learning, natural language processing, digital phenotyping, and multimodal data integration. This review highlights the advancements in the integration of AI in psychiatric care, such as chatbot-mediated psychotherapy, reinforcement learning for clinical decision-making, and AI-driven triage systems in resource-constrained environments. However, there are still serious concerns about data privacy, algorithmic bias, informed consent, and the interpretability of AI systems. Other barriers to fair and safe implementation include discrepancies in training datasets, underrepresentation of marginalized groups, and a lack of clinician preparedness. There is a need for transparent, explainable, and ethically regulated AI systems that enhance, rather than replace, human decision-making. A hybrid human-AI approach to psychiatry is recommended to address these limitations, while interdisciplinary studies, strong validation frameworks, and inclusive policymaking are needed to guarantee that AI-enhanced mental health treatment continues to be effective, fair, and reliable.
DOI: https://doi.org/10.37349/edht.2025.101174

Aim:
To assess the burden of digital eye strain (DES) and associated factors among technology students at public universities in southern Ethiopia.
Methods:
A cross-sectional study was conducted from March to April 2024 at three universities—Hawassa, Dilla, and Jinka. Data were collected using pretested self-administered questionnaires, including the Digital Eye Strain Questionnaire and other relevant variables.
Results:
The survey tool was distributed to the total study population of 788 students, of whom 403 completed the survey, representing 93.5% of the calculated sample size of 431. Participants were predominantly male (74.7%) and enrolled at Hawassa University (57.8%). Daily digital device usage of ≥ 2 hours was reported by 259 (64.3%), and 72.7% had owned digital devices for > 2 years. Few participants reported smoking (0.7%), alcohol use (10.9%), or khat chewing (7.7%), and 13.9% had a history of accidents. Overall, 68.5% [95% confidence interval (CI): 64.0%–73.0%] experienced at least one symptom of DES in the past 12 months, with photophobia being the most common. DES was experienced more likely among students from Hawassa University [adjusted odds ratio (AOR) = 2.43; 95% CI: 1.11–5.30; p = 0.026], females (AOR = 2.32; 95% CI: 1.25–4.31; p = 0.008), current alcohol consumers (AOR = 3.12; 95% CI: 1.20–8.08; p = 0.019), and those with a history of accidents (AOR = 2.68; 95% CI: 1.17–6.13; p = 0.020).
Conclusions:
Over two-thirds of final-year technology students in southern Ethiopian universities reported at least one symptom of DES, with higher risk observed among females, alcohol users, and those with prior accidents.
Aim:
To assess the burden of digital eye strain (DES) and associated factors among technology students at public universities in southern Ethiopia.
Methods:
A cross-sectional study was conducted from March to April 2024 at three universities—Hawassa, Dilla, and Jinka. Data were collected using pretested self-administered questionnaires, including the Digital Eye Strain Questionnaire and other relevant variables.
Results:
The survey tool was distributed to the total study population of 788 students, of whom 403 completed the survey, representing 93.5% of the calculated sample size of 431. Participants were predominantly male (74.7%) and enrolled at Hawassa University (57.8%). Daily digital device usage of ≥ 2 hours was reported by 259 (64.3%), and 72.7% had owned digital devices for > 2 years. Few participants reported smoking (0.7%), alcohol use (10.9%), or khat chewing (7.7%), and 13.9% had a history of accidents. Overall, 68.5% [95% confidence interval (CI): 64.0%–73.0%] experienced at least one symptom of DES in the past 12 months, with photophobia being the most common. DES was experienced more likely among students from Hawassa University [adjusted odds ratio (AOR) = 2.43; 95% CI: 1.11–5.30; p = 0.026], females (AOR = 2.32; 95% CI: 1.25–4.31; p = 0.008), current alcohol consumers (AOR = 3.12; 95% CI: 1.20–8.08; p = 0.019), and those with a history of accidents (AOR = 2.68; 95% CI: 1.17–6.13; p = 0.020).
Conclusions:
Over two-thirds of final-year technology students in southern Ethiopian universities reported at least one symptom of DES, with higher risk observed among females, alcohol users, and those with prior accidents.
DOI: https://doi.org/10.37349/edht.2025.101173

Aim:
Generative text-to-image technologies offer new opportunities for individuals to visually articulate internal experiences. While traditional artistic self-portraiture has been extensively associated with self-insight, its AI-assisted equivalent remains underexplored. This study investigates the experiential and assessment potential of AI-generated self-representations and assesses their applicability within contemporary digital mental health frameworks.
Methods:
Five participants (aged 18–58) engaged in a 45-minute image generation session using Midjourney, producing approximately 500 images. This was followed by semi-structured interviews analyzed via interpretative phenomenological analysis (IPA). This study is idiographic and exploratory, drawing on the principles of IPA. Our aim is an in-depth explication of lived experience and shared experiential layers across cases. The findings should therefore be read as hypothesis-generating and as groundwork for future, larger-scale and mixed-methods evaluations and potential telepsychology integrations.
Results:
Three group experiential themes: (1) images as functional tools (e.g., as sources of comfort or aspirational vision boards); (2) self-reflective space (facilitating spontaneous self-disclosure and novel insight); and (3) modalities of self-definition (symbolic representation and narrative arc). Participants described the process as highly engaging and reported enhanced self-efficacy.
Conclusions:
AI-assisted image generation presents a flexible and user-centered modality for psychological reflection, with potential to augment art- and narrative-based therapeutic interventions. Ethical measures (e.g., anonymized data handling, withdrawal options) proved viable. Further research should explore larger, diverse samples and examine integration within telepsychology platforms to assess clinical utility.
Aim:
Generative text-to-image technologies offer new opportunities for individuals to visually articulate internal experiences. While traditional artistic self-portraiture has been extensively associated with self-insight, its AI-assisted equivalent remains underexplored. This study investigates the experiential and assessment potential of AI-generated self-representations and assesses their applicability within contemporary digital mental health frameworks.
Methods:
Five participants (aged 18–58) engaged in a 45-minute image generation session using Midjourney, producing approximately 500 images. This was followed by semi-structured interviews analyzed via interpretative phenomenological analysis (IPA). This study is idiographic and exploratory, drawing on the principles of IPA. Our aim is an in-depth explication of lived experience and shared experiential layers across cases. The findings should therefore be read as hypothesis-generating and as groundwork for future, larger-scale and mixed-methods evaluations and potential telepsychology integrations.
Results:
Three group experiential themes: (1) images as functional tools (e.g., as sources of comfort or aspirational vision boards); (2) self-reflective space (facilitating spontaneous self-disclosure and novel insight); and (3) modalities of self-definition (symbolic representation and narrative arc). Participants described the process as highly engaging and reported enhanced self-efficacy.
Conclusions:
AI-assisted image generation presents a flexible and user-centered modality for psychological reflection, with potential to augment art- and narrative-based therapeutic interventions. Ethical measures (e.g., anonymized data handling, withdrawal options) proved viable. Further research should explore larger, diverse samples and examine integration within telepsychology platforms to assess clinical utility.
DOI: https://doi.org/10.37349/edht.2025.101172
This article belongs to the special issue Digital Health Innovations in the Battle Against Psychological Problems: Progress, Hurdles, and Prospects

We describe the rationale for and design of a non-inferiority trial to evaluate the relative effectiveness of electronic alcohol screening with in-person vs. electronic brief intervention (BI) approaches implemented in Alexandra Township, South Africa, and Zacatecas-Guadalupe, Mexico. The purpose of screening and brief intervention is to identify individuals whose responses to the Alcohol Use Disorders Identification Test (AUDIT) indicate risky drinking patterns and offer them information and advice to help them reduce their drinking. We seek to determine whether a BI comprising information and advice delivered electronically, along with the opportunity to schedule an appointment with a health care professional at a later time, is not significantly worse than a more labor-intensive traditional BI provided through a face-to-face interaction with a health professional immediately following screening. Selected patients visiting participating health clinics in Alexandra and Zacatecas-Guadalupe will be asked to complete the AUDIT screening using an online app accessed via a handheld device. Those whose scores indicate risky alcohol consumption will be invited to participate in the study. Participants at the clinics will be allocated in alternate weeks to either a customary in-person BI or an electronic BI. Based on power analyses taking attrition and nesting within clinics into account, the target sample sizes are 680 in Alexandra and 560 in Zacatecas-Guadalupe. Measures of 30-day alcohol consumption and AUDIT scores will be obtained at baseline, 3 months, and 6 months. The primary outcome will be the past 30-day quantity-frequency of alcohol consumption. Outcomes will be compared for the two study conditions using mixed effects multilevel regression analyses to account for nesting of observations within participants and participants within clinics. Potential socio-demographic covariates include gender, age, marital status, the highest completed level of education, family’s primary native language (a proxy for ethnicity/culture), presence of household members younger than 16, and subjective economic status (Trial ID: NCT07150156. Clinical trial platform: ClinicalTrials.gov Protocol Registration and Results System. Web address: https://clinicaltrials.gov).
We describe the rationale for and design of a non-inferiority trial to evaluate the relative effectiveness of electronic alcohol screening with in-person vs. electronic brief intervention (BI) approaches implemented in Alexandra Township, South Africa, and Zacatecas-Guadalupe, Mexico. The purpose of screening and brief intervention is to identify individuals whose responses to the Alcohol Use Disorders Identification Test (AUDIT) indicate risky drinking patterns and offer them information and advice to help them reduce their drinking. We seek to determine whether a BI comprising information and advice delivered electronically, along with the opportunity to schedule an appointment with a health care professional at a later time, is not significantly worse than a more labor-intensive traditional BI provided through a face-to-face interaction with a health professional immediately following screening. Selected patients visiting participating health clinics in Alexandra and Zacatecas-Guadalupe will be asked to complete the AUDIT screening using an online app accessed via a handheld device. Those whose scores indicate risky alcohol consumption will be invited to participate in the study. Participants at the clinics will be allocated in alternate weeks to either a customary in-person BI or an electronic BI. Based on power analyses taking attrition and nesting within clinics into account, the target sample sizes are 680 in Alexandra and 560 in Zacatecas-Guadalupe. Measures of 30-day alcohol consumption and AUDIT scores will be obtained at baseline, 3 months, and 6 months. The primary outcome will be the past 30-day quantity-frequency of alcohol consumption. Outcomes will be compared for the two study conditions using mixed effects multilevel regression analyses to account for nesting of observations within participants and participants within clinics. Potential socio-demographic covariates include gender, age, marital status, the highest completed level of education, family’s primary native language (a proxy for ethnicity/culture), presence of household members younger than 16, and subjective economic status (Trial ID: NCT07150156. Clinical trial platform: ClinicalTrials.gov Protocol Registration and Results System. Web address: https://clinicaltrials.gov).
DOI: https://doi.org/10.37349/edht.2025.101171
This article belongs to the special issue Telepsychiatry in Low-and Middle-income Countries: an Update
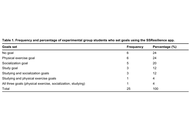
Aim:
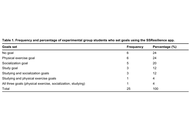
Designed to support the mental well-being of university students, the gamified Student Stress Resilience (SSResilience) app guides users in setting and working toward goals related to studying, socializing, and exercising. The app monitors progress through a combination of data from a user’s phone (via Internet of Things sensors) and information they enter themselves. This efficacy study documented students’ goal-setting efforts (RQ1) and examined the app’s effect on students’ anxiety, resilience, and psychological well-being (RQ2).
Methods:
A quasi-experimental pretest-posttest control group design was used. Experimental group students (n1 = 25) used the app for two weeks. Control group students (n2 = 50) used different means to set the same goals. All students were pre-tested and post-tested on anxiety, well-being, and resilience using standardized questionnaires.
Results:
Nineteen out of 25 experimental group students used the app to set one or more goals (19/25), and 18 of them found it helpful (18/25). The experimental group experienced a significant (t(22) = 2.72, P = 0.013) decrease in anxiety from Mpre = 8.96 (SD = 5.30) to Mpost = 5.76 (SD = 4.59), an increase in well-being from Mpre = 54.6 (SD = 25.88) to Mpost = 65.12 (SD = 23.90), but no change in resilience. Control group students’ (n = 43) measurements remained unchanged.
Conclusions:
Preliminary findings indicate a potential value of the SSResilience app for significantly reducing students’ anxiety and increasing their well-being. Integrating Internet of Things technology (built-in phone sensors) into gamified apps for health holds significant promise by offering valuable data to users, app developers, and researchers. Future research will use wearables to measure stress and physical activity more accurately than self-reports.
Aim:
Designed to support the mental well-being of university students, the gamified Student Stress Resilience (SSResilience) app guides users in setting and working toward goals related to studying, socializing, and exercising. The app monitors progress through a combination of data from a user’s phone (via Internet of Things sensors) and information they enter themselves. This efficacy study documented students’ goal-setting efforts (RQ1) and examined the app’s effect on students’ anxiety, resilience, and psychological well-being (RQ2).
Methods:
A quasi-experimental pretest-posttest control group design was used. Experimental group students (n1 = 25) used the app for two weeks. Control group students (n2 = 50) used different means to set the same goals. All students were pre-tested and post-tested on anxiety, well-being, and resilience using standardized questionnaires.
Results:
Nineteen out of 25 experimental group students used the app to set one or more goals (19/25), and 18 of them found it helpful (18/25). The experimental group experienced a significant (t(22) = 2.72, P = 0.013) decrease in anxiety from Mpre = 8.96 (SD = 5.30) to Mpost = 5.76 (SD = 4.59), an increase in well-being from Mpre = 54.6 (SD = 25.88) to Mpost = 65.12 (SD = 23.90), but no change in resilience. Control group students’ (n = 43) measurements remained unchanged.
Conclusions:
Preliminary findings indicate a potential value of the SSResilience app for significantly reducing students’ anxiety and increasing their well-being. Integrating Internet of Things technology (built-in phone sensors) into gamified apps for health holds significant promise by offering valuable data to users, app developers, and researchers. Future research will use wearables to measure stress and physical activity more accurately than self-reports.
DOI: https://doi.org/10.37349/edht.2025.101170
This article belongs to the special issue Digital Health Innovations in the Battle Against Psychological Problems: Progress, Hurdles, and Prospects

Aim:
Obsessive-compulsive disorder (OCD) is a mental health condition that significantly interferes with the school environment. The concealment of symptoms, lack of identification, and limited knowledge about the disorder often lead to delays in help-seeking, which are associated with greater chronicity, increased interference, and poorer treatment response. Programmes that educate teachers on early detection of OCD could help identify children at risk and promote help-seeking behavior. This study analyzed the feasibility, acceptability, and preliminary efficacy of the health app esTOCma from both quantitative and qualitative perspectives among teachers, as well as explored areas for improvement.
Methods:
A total of 19 teachers (mean age = 47.74 years, SD = 11.2) completed the intervention along with pre- and post-intervention assessments through the app. In addition, they responded to open-ended questions to share their opinions about the app.
Results:
Teachers took an average of 4.89 days (SD = 4.21) to complete the intervention. The app demonstrated excellent usability (M = 85.5, SD = 10.3) and was found useful by the majority of participants (89.5%), who reported satisfaction (84.2%) and stated they had learned considerably (73.7%) through its use. Upon completing the intervention, participants showed greater understanding of OCD and its treatments (MHLQ-R: z = –2.92, p = 0.004), lower levels of stigma (AQ-9: z = –3.67, p < 0.001), and a higher intention to seek professional help in case of experiencing obsessive-compulsive symptoms (GHSQ: z = –2.50, p = 0.012).
Conclusions:
esTOCma appears to be a feasible app in an educational context, showing high acceptability among participating teachers. Moreover, the app increases knowledge and understanding of OCD, promotes the intention to seek professional help, and reduces stigma toward the disorder. Several improvements are suggested to further enhance the app’s potential impact in educational settings.
Aim:
Obsessive-compulsive disorder (OCD) is a mental health condition that significantly interferes with the school environment. The concealment of symptoms, lack of identification, and limited knowledge about the disorder often lead to delays in help-seeking, which are associated with greater chronicity, increased interference, and poorer treatment response. Programmes that educate teachers on early detection of OCD could help identify children at risk and promote help-seeking behavior. This study analyzed the feasibility, acceptability, and preliminary efficacy of the health app esTOCma from both quantitative and qualitative perspectives among teachers, as well as explored areas for improvement.
Methods:
A total of 19 teachers (mean age = 47.74 years, SD = 11.2) completed the intervention along with pre- and post-intervention assessments through the app. In addition, they responded to open-ended questions to share their opinions about the app.
Results:
Teachers took an average of 4.89 days (SD = 4.21) to complete the intervention. The app demonstrated excellent usability (M = 85.5, SD = 10.3) and was found useful by the majority of participants (89.5%), who reported satisfaction (84.2%) and stated they had learned considerably (73.7%) through its use. Upon completing the intervention, participants showed greater understanding of OCD and its treatments (MHLQ-R: z = –2.92, p = 0.004), lower levels of stigma (AQ-9: z = –3.67, p < 0.001), and a higher intention to seek professional help in case of experiencing obsessive-compulsive symptoms (GHSQ: z = –2.50, p = 0.012).
Conclusions:
esTOCma appears to be a feasible app in an educational context, showing high acceptability among participating teachers. Moreover, the app increases knowledge and understanding of OCD, promotes the intention to seek professional help, and reduces stigma toward the disorder. Several improvements are suggested to further enhance the app’s potential impact in educational settings.
DOI: https://doi.org/10.37349/edht.2025.101169
This article belongs to the special issue Digital Health Innovations in the Battle Against Psychological Problems: Progress, Hurdles, and Prospects
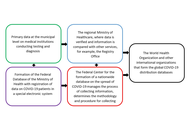
Aim:
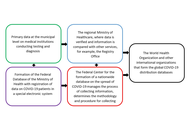
This study analyses the time series of daily increases in the number of diagnosed COVID-19 cases in Russia and countries from different continents. The aim of the study is to identify the specifics of the population response of different countries to the spread of the pandemic and anti-epidemic measures of public authorities to determine the most effective model to describe this process. This is a problematic, synoptic, and pilot study.
Methods:
To evaluate this response strategy, models and methods from reliability theory are used to describe the probability of health protection, the probability density function of an increasing number of cases, the integrated risk of infection, the risk of morbidity, the acceptable risk, and the manageability of the epidemic situation. To approximate infection curves, various daily incidence rate functions are used and compared, and their coefficients are calculated for various pandemic waves.
Results:
The results demonstrate that the Fréchet distribution function is the best model for the epidemic process. Indicators of variability in acceptable risk were identified during the first stage of pandemic development, showing the varying controllability of the situation by health systems. Through meta-analysis, country distributions were shown to appear as a single pattern, abstracted from local conditions. Estimated coefficients of reliability functions allow the construction of cartograms that reflect the peculiarities of state epidemic regulation and the stages of global pandemic deployment.
Conclusions:
The findings confirm the effectiveness of the selected model in terms of reliability theory and identify directions for model improvement, taking into account the dynamic nature of the pandemic and its specific characteristics in different countries. The study is based on the methodological approach of function stratification (geometric fiber bundle). It allows for a deeper understanding of the identified patterns within a broader knowledge system.
Aim:
This study analyses the time series of daily increases in the number of diagnosed COVID-19 cases in Russia and countries from different continents. The aim of the study is to identify the specifics of the population response of different countries to the spread of the pandemic and anti-epidemic measures of public authorities to determine the most effective model to describe this process. This is a problematic, synoptic, and pilot study.
Methods:
To evaluate this response strategy, models and methods from reliability theory are used to describe the probability of health protection, the probability density function of an increasing number of cases, the integrated risk of infection, the risk of morbidity, the acceptable risk, and the manageability of the epidemic situation. To approximate infection curves, various daily incidence rate functions are used and compared, and their coefficients are calculated for various pandemic waves.
Results:
The results demonstrate that the Fréchet distribution function is the best model for the epidemic process. Indicators of variability in acceptable risk were identified during the first stage of pandemic development, showing the varying controllability of the situation by health systems. Through meta-analysis, country distributions were shown to appear as a single pattern, abstracted from local conditions. Estimated coefficients of reliability functions allow the construction of cartograms that reflect the peculiarities of state epidemic regulation and the stages of global pandemic deployment.
Conclusions:
The findings confirm the effectiveness of the selected model in terms of reliability theory and identify directions for model improvement, taking into account the dynamic nature of the pandemic and its specific characteristics in different countries. The study is based on the methodological approach of function stratification (geometric fiber bundle). It allows for a deeper understanding of the identified patterns within a broader knowledge system.
DOI: https://doi.org/10.37349/edht.2025.101168
This article belongs to the special issue Data-informed Decision Making in Healthcare
 Previous
Previous