Affiliation:
1School of Public Health, College of Medicine and Health Science, Hawassa University, Hawassa, Ethiopia
Email: yadessategene@yahoo.com
ORCID: https://orcid.org/0000-0003-1409-8697
Affiliation:
1School of Public Health, College of Medicine and Health Science, Hawassa University, Hawassa, Ethiopia
Affiliation:
2Department of Family Medicine, School CAPHRI, Maastricht University, 6200 MD Maastricht, Netherlands
Affiliation:
2Department of Family Medicine, School CAPHRI, Maastricht University, 6200 MD Maastricht, Netherlands
Affiliation:
3Hawassa University Comprehensive and Specialized Hospital, Hawassa University, Hawassa, Ethiopia
Affiliation:
1School of Public Health, College of Medicine and Health Science, Hawassa University, Hawassa, Ethiopia
ORCID: https://orcid.org/0000-0003-3049-7073
Affiliation:
4School of Medicine, College of Medicine and Health Science, Hawassa University, Hawassa, Ethiopia
ORCID: https://orcid.org/0000-0003-1511-1531
Affiliation:
2Department of Family Medicine, School CAPHRI, Maastricht University, 6200 MD Maastricht, Netherlands
5General Practice Research Unit, Department of Community Medicine, UiT the Arctic University of Norway, N-9037 Tromsø, Norway
ORCID: https://orcid.org/0000-0002-6279-8068
Explor Med. 2025;6:1001317 DOI: https://doi.org/10.37349/emed.2025.1001317
Received: January 13, 2025 Accepted: April 21, 2025 Published: May 08, 2025
Academic Editor: Hongzhou Lu, Shenzhen Third People’s Hospital, National Clinical Research Center for Infectious Diseases, China
The article belongs to the special issue Global Perspectives on the Clinical Diagnosis, Treatment, and Functional Cure of HIV Infection in the Post-ART Era
Aim: This study aimed to assess the prevalence of hypertension and diabetes and the factors associated with these conditions in adult patients living with human immunodeficiency virus (HIV). It also aimed to assess their self-management skills for these chronic conditions, as effective self-management is critical to improving health outcomes and enhancing quality of life for individuals managing multiple health challenges.
Methods: A cross-sectional, facility-based study was conducted in May and June 2022. We randomly selected 520 adult people living with HIV attending antiretroviral therapy clinics in three hospitals in Southern Ethiopia. Nine trained nurses collected data using a pre-tested structured questionnaire, and SPSS version 20 was employed for analysis. A logistic regression model was utilized to identify factors associated with chronic comorbidities in HIV.
Results: The mean age of participants was 38.7 ± 9.01 years, with diabetes and hypertension prevalence at 1.5% [95% CI: (0.70, 3.00)] and 9% [95% CI: (7.10, 12.30)], respectively. Chronic comorbidities such as hypertension and diabetes were significantly associated with age 35–54 years [adjusted odds ratio (AOR) = 3.54, 95% CI: (1.46, 8.74)], 55 years and older [AOR = 7.66, 95% CI: (2.29, 25.50)], and overweight or obesity [AOR = 2.82, 95% CI: (1.00, 7.93)]. The overall HIV self-management score was 42 ± 3.92 out of 60, with the lowest mean score (1.69 ± 0.92) in the social support domain.
Conclusions: The prevalence of diabetes and hypertension was relatively low in our study. In Ethiopia, self-management skills appear low, and the limited understanding of self-management concepts raises questions about the validity of the self-management scale, potentially leading to inaccurate skill assessments.
According to recent statistics, 38 million people worldwide were infected with the human immunodeficiency virus (HIV) in 2019, with 20.7 million from East and Southern Africa [1, 2]. Ethiopia is among the most seriously affected countries in sub-Saharan Africa, with a prevalence of 0.9% and 27,104 new cases in 2017 [3]. Increased coverage of antiretroviral therapy (ART) has brought a substantial improvement in survival among people living with HIV (PLWH) [4]. HIV disease requires lifelong therapy, and it has become a risk factor for additional chronic diseases, such as cardiovascular diseases and diabetes [5, 6]. Over 50% of PLWH with multiple chronic conditions are expected to have multiple limitations in their everyday lives and are more likely to indicate a decline in self-reported health [7, 8].
An increasing burden of chronic comorbidity among PLWH is becoming one of the greatest challenges that health care systems are facing globally [9, 10]. An increase in complexity and fragmentation of chronic care (poorly coordinated care) is reported by both patients and healthcare providers [11]. Patients with multiple chronic diseases experience unfavorable health outcomes and give rise to challenges in patient care and medical costs [12]. According to the evidence, those with multiple chronic conditions use more health-care resources than those with fewer conditions, and their costs are up to seven times higher than those with only one chronic condition [13]. When chronic diseases began to emerge, patients, health professionals, and health services had to play new roles [14]. When health care systems shift from acute to chronic care, a self-management model is needed in which the patient has an active and informed role in healthcare decision-making [15]. Since patients spend most of their time away from medical facilities, they have to manage care activities on a daily basis [16].
Self-management is a process through which individuals actively cope with their chronic diseases in the context of their daily lives [17]. Self-management is regarded as a best practice for improving clinical care and outcomes. It can also reduce the burden of chronic disease on healthcare system resources and capacity by helping patients to be more active and engaged in their self-care [18]. Chronic care programs that promote self-management are effective for various chronic diseases, including HIV. These programs typically involve personalized care plans, regular viral load monitoring, and mental health resources, empowering individuals to actively manage their treatment and enhance their quality of life [19, 20]. The response of health systems to facilitate proper self-management is highly inadequate in low-income countries [21]. Although also in high-income countries, optimal self-management support for chronically ill patients remains relatively underdeveloped and far from accomplished [22].
In lower and middle-income countries (LMICs) like Ethiopia, where health systems are already overburdened by the rapid expansion of non-communicable diseases and the high burden of communicable diseases, the impact of comorbidity is expected to be severe [23]. However, no evidence exists on the best techniques for managing chronic comorbidities in LMICs [24]. Health systems in LMICs are generally constructed on traditional one-size-fits-all chronic care models rather than developing a model of care for every possible combination of chronic disorders [23, 24]. As a result of their uncoordinated responses to each of their health issues, people who have chronic comorbidity are more likely to face rising and overwhelming complexity (complicated and challenging situations) [25, 26]. Therefore, more and more attention is being paid to the issue of comorbidity in HIV disease and the fact that it could overpower health-care systems, especially in resource-limited regions that lack the infrastructure to organize chronic care [27].
Previous research on chronic comorbidities among PLWH in Ethiopia has been limited by small sample sizes [28–30]. Additionally, self-management, a multifaceted concept, has not been extensively studied in this population [31], leaving the extent of self-management among PLWH in Ethiopia largely unknown. When we gain more insight into chronic comorbidity and self-management, it will help to bridge the gap between the needs of the patients and the care that is provided [32]. The aim of this study is to assess the prevalence of chronic comorbidities and the self-management skills of adults living with HIV in Ethiopia. It seeks to answer key questions about the extent of chronic comorbidities, variation in self-management skills, and factors influencing both comorbidity and self-management. The study aims to highlight the challenges this population faces in managing their chronic health conditions by addressing these issues.
A cross-sectional study was conducted at three selected hospitals from May to June 2022. Hawassa University Comprehensive and Specialized Hospital (HUCSH) is a tertiary-level hospital that delivers specialized and referral services for general hospitals. Adare and Yirgalem Hospitals are general hospitals that deliver secondary-level healthcare. HUCSH and Adare General Hospitals are found in Hawassa Town, the capital of Sidama Regional State of Ethiopia, and are located 275 km south of Addis Ababa, the capital of Ethiopia. The other, Yirgalem General Hospital, is located 47 km southeast of the regional capital, Hawassa. At the beginning of this study (May 7, 2022), HUCSH, Adare, and Yirgalem General Hospital gave ART service for 2,553, 1,821, and 1,476 adult PLWH, respectively.
All adult PLWH aged ≥ 18 years attending the ART clinic in this period were eligible for this study. The formula for single population proportion was applied to compute the optimal sample size for estimating the number of PLWH needed for this study. The prevalence of hypertension among PLWH (12.7%) was taken from the study conducted in Eastern Ethiopia [28]. The calculation was performed with a 95% confidence level (Z = 1.96) and a 3% margin of error (d) as inputs. For the sake of accommodating the possibility of non-response, a 10% contingency was added. Accordingly, the calculated sample size was 520 participants. A proportionate sample was determined, and thus, 227 participants were targeted from HUCSH, 162 participants from Adare General Hospital, and 131 from Yirgalem General Hospital. Individual study participants who fit the criteria and volunteered to participate were selected at random when they arrived at the ART clinic.
Nine trained nurses used interview-administered questionnaires to collect data during routine consultations, and relevant medical data were retrieved from medical files. The study participants’ socioeconomic and ART-related variables were collected using a structured questionnaire. To collect data on dietary diversity and household food insecurity, the Household Dietary Diversity Score (HDDS) of the food and nutrition technical assistance indicator guide [33] and the Household Food Insecurity Access Scale (HFIAS) [34] were used, respectively. The weight was measured using a calibrated digital Seca® scale and recorded to the nearest 0.1 kg. Height was measured using a stadiometer by positioning the patient at the Frankfurt plane to the nearest 0.1 cm. Normal weight and underweight were defined as body mass index (BMI) 18.5–24.9 kg/m2 and < 18.5 kg/m2, respectively, whereas overweight and obesity were defined as BMI ≥ 25 kg/m2 and > 30 kg/m2, respectively [35].
Random blood glucose levels were measured using the Fia Biomed Blood Glucose Meter (Glucometer) via finger puncture. According to the American Diabetes Association, diabetes is defined by fasting plasma glucose levels ≥ 126 mg/dL, 2-hour plasma glucose ≥ 200 mg/dL during an oral glucose tolerance test, hemoglobin A1C ≥ 6.5%, or a random plasma glucose ≥ 200 mg/dL in patients with classic hyperglycemia symptoms [36]. If random blood glucose indicated diabetes (≥ 200 mg/dL) or impaired glucose regulation (140–199 mg/dL), fasting blood glucose levels were measured for confirmation. Blood pressure was assessed using a standard mercury sphygmomanometer on the left arm, with three readings taken at 5-minute intervals. The average of the last two readings was used, and hypertension was diagnosed based on WHO criteria: systolic BP ≥ 140 mmHg or diastolic BP ≥ 90 mmHg [37].
To assess self-management in PLWH, the HIV Self-management Scale was used [38]. To ensure consistency, the questionnaire was translated from English to Amharic and then retranslated to the original version. The HIV Self-Management Scale consists of 20 items relating to three domains. The domains consist of 12 items with daily self-management health practices (e.g., “Staying physically active is an important part of my HIV self-management strategy”); 3 items with social support for HIV self-management (e.g., “Attending support groups is an important part of my HIV self-management strategy”); and 5 items on the chronic nature of HIV self-management (e.g., “I have accepted that HIV is a life-long condition that can be managed”). Each item is scored on a 0–3 scale: 0 = not applicable, 1 = none of the time, 2 = some of the time, and 3 = all of the time. Each domain is scored separately and divided by the number of items in that domain, and the total score of the scale was calculated by summing items in all domains; the possible score thus ranged from 0 to 60.
Data were entered, cleaned, coded, and analyzed using SPSS for Windows version 20.0 to calculate proportions, frequencies, and means. Binary logistic regression was used to evaluate the relationship between independent variables and outcome variables at a significance level of p < 0.25, and significant variables were selected for multivariable analysis. The Hosmer and Lemeshow test was used to assess model fit, and an adjusted odds ratio (AOR) with a 95% confidence interval (CI) was calculated to determine the strength of the associations, with statistical significance set at p ≤ 0.05.
A total of 520 patients were included in the study, with a response rate of 100% of those invited. The mean age of study participants was 38.7 ± 9.01 years. Study participants were predominantly female (63%), single (45%), and had a tertiary level of education (27%). More than half of the participants in the study were orthodox Christians (51%), had a family size of 3–6 (60%), and half of them (50%) had a monthly household income of < 1,500 Ethiopian Birr. The majority of them (94%) live in urban areas and are privately employed (30%) (Table 1).
Socio-demographic characteristics of adult PLWH in selected Hospitals of Southern Ethiopia, 2022
| Variable | Frequency (n = 520) | Percent (%) |
|---|---|---|
| Sex | ||
| Male | 191 | 37 |
| Female | 329 | 63 |
| Age | ||
| ≤ 20 | 9 | 2 |
| 21–30 | 94 | 18 |
| 31–40 | 236 | 45 |
| 41–50 | 128 | 25 |
| 51–60 | 53 | 10 |
| Marital status | ||
| Single | 233 | 45 |
| Married | 89 | 17 |
| Divorced | 98 | 19 |
| Widowed | 100 | 19 |
| Education level | ||
| No formal education | 55 | 11 |
| Primary education | 131 | 25 |
| Secondary education | 194 | 37 |
| Tertiary education | 140 | 27 |
| Religion | ||
| Orthodox | 263 | 51 |
| Muslim | 80 | 15 |
| Protestant | 171 | 33 |
| Others | 6 | 1 |
| Place of residence | ||
| Urban | 487 | 94 |
| Rural | 33 | 6 |
| Occupation | ||
| Government employee | 111 | 21 |
| Private employee | 156 | 30 |
| Daily-laborer | 58 | 11 |
| House wife | 13 | 3 |
| Merchant | 78 | 15 |
| Others | 104 | 20 |
| Family members | ||
| < 3 | 153 | 29 |
| 3–6 | 310 | 60 |
| ≥ 7 | 57 | 11 |
| Income level (Ethiopian Birr) | ||
| < 1,500 | 262 | 50 |
| ≥ 1,500 | 258 | 50 |
Private employee: a person who works for a private employer or in a private organization and receives regular remuneration in salary. 1 USD = 44.15 Ethiopian Birr, 2021. PLWH: people living with human immunodeficiency virus
Of the 520 study participants, 99% were already on ART, with only 1% new to treatment. Over half had a normal BMI (59%) and a CD4 count of ≥ 500 (58.4%), but 53% did not exercise regularly. Additionally, 55% had poor dietary diversity, 77.5% experienced food insecurity, and 71% had been on ART for over 24 months. Most participants (92%) were in WHO clinical stage one and did not smoke (99%) or drink (88%) (Table 2).
Health-related characteristics of adult PLWH in selected Hospitals of Southern Ethiopia, 2022
| Variable | Frequency (n = 520) | Percent (%) |
|---|---|---|
| WHO clinical stage | ||
| Stage I | 478 | 92 |
| Stage II | 19 | 4 |
| Stage III | 18 | 3 |
| Stage IV | 5 | 1 |
| ART regimen started | ||
| AZT-3TC-EFV | 87 | 16.7 |
| AZT-3TC-NVP | 93 | 18 |
| TDF-3TC-EFV | 268 | 51.5 |
| Others | 72 | 13.8 |
| Duration of ART in months | ||
| < 24 | 149 | 29 |
| ≥ 24 | 371 | 71 |
| CD4 count (n = 450 patients) | ||
| < 200 | 45 | 10 |
| 200–349 | 65 | 14.5 |
| 350–499 | 77 | 17.1 |
| ≥ 500 | 263 | 58.4 |
| Regular physical exercise | ||
| Yes | 242 | 47 |
| No | 278 | 53 |
| History of alcohol consumption | ||
| Yes | 64 | 12 |
| No | 456 | 88 |
| History of cigarette smoking | ||
| Yes | 7 | 1 |
| No | 513 | 99 |
| BMI | ||
| Underweight (< 18.5) | 77 | 15 |
| Normal weight (18.5–24.9) | 307 | 59 |
| Overweight (25–30) | 100 | 19 |
| Obesity (> 30) | 36 | 7 |
| Dietary diversity score | ||
| Low | 285 | 55 |
| High | 235 | 45 |
| Household food security | ||
| Secured | 117 | 22.5 |
| Insecure | 403 | 77.5 |
PLWH: people living with human immunodeficiency virus; ART: antiretroviral therapy; BMI: body mass index; AZT-3TC-EFV: Zidovudine-Lamivudine-Efavirenz; AZT-3TC-NVP: Zidovudine-Lamivudine-Nevirapine; TDF-3TC-EFV: Tenofovir Disoproxil Fumarate-Lamivudine-Efavirenz
The prevalence of diabetes and hypertension was 1.5% [95% CI: (0.70, 3.00)] and 9% [95% CI: (7.10, 12.30)], respectively. The very few cases of diabetes seemed to be distributed rather equally across different subgroups. Hypertension seemed to concentrate among the older and more educated patients (Table 3).
Chronic comorbidity among adult PLWH in selected Hospitals of Southern Ethiopia, 2022
| Variable | Chronic comorbidity | |
|---|---|---|
| Hypertension (n = 49) | Diabetes (n = 8) | |
| Sex | ||
| Male | 24 (49) | 3 (37.5) |
| Female | 25 (51) | 5 (62.5) |
| Age | ||
| 21–30 | 5 (10) | 0 (0) |
| 31–40 | 11 (23) | 1 (12.5) |
| 41–50 | 24 (49) | 3 (37.5) |
| 51–60 | 9 (18) | 4 (50) |
| Education level | ||
| No formal education | 5 (10) | 1 (12.5) |
| Primary education | 10 (20) | 2 (25) |
| Secondary education | 20 (41) | 3 (37.5) |
| Tertiary education | 14 (29) | 2 (25) |
| Occupation | ||
| Government employee | 14 (29) | 0 (0) |
| Private employee | 10 (20) | 5 (62.5) |
| Daily-laborer | 6 (12) | 1 (12.5) |
| Merchant | 9 (19) | 2 (25) |
| Others | 10 (20) | 0 (0) |
| Marital status | ||
| Single | 22 (44.9) | 3 (37.5) |
| Married | 9 (18.4) | 0 (0) |
| Divorced | 8 (16.3) | 2 (25) |
| Widowed | 10 (20.4) | 3 (37.5) |
| Regular physical exercise | ||
| Yes | 22 (45) | 4 (50) |
| No | 27 (55) | 4 (50) |
| Duration of ART | ||
| < 24 months | 17 (35) | 2 (25) |
| ≥ 24 months | 32 (65) | 6 (75) |
| Income level (Ethiopian Birr) | ||
| < 1,500 | 20 (41) | 4 (50) |
| ≥ 1,500 | 29 (59) | 4 (50) |
| Place of residence | ||
| Urban | 49 (100) | 8 (100) |
| Rural | 0 (0) | 0 (0) |
| Religion | ||
| Orthodox | 26 (53) | 6 (75) |
| Muslim | 13 (27) | 0 (0) |
| Protestant | 9 (18) | 2 (25) |
| Others | 1 (2) | 0 (0) |
| WHO clinical stage | ||
| Stage I | 48 (98) | 8 (100) |
| Stage II | 1 (2) | 0 (0) |
| Stage III | 0 (0) | 0 (0) |
| Stage IV | 0 (0) | 0 (0) |
| CD4 count | ||
| < 200 | 3 (6.1) | 0 (0) |
| 200–349 | 9 (18.4) | 2 (25) |
| 350–499 | 7 (14.3) | 3 (37.5) |
| ≥ 500 | 30 (61.2) | 3 (37.5) |
| History of alcohol consumption | ||
| Yes | 8 (16) | 3 (37.5) |
| No | 41 (84) | 5 (62.5) |
| BMI | ||
| Underweight (< 18.5) | 4 (8) | 0 (0) |
| Normal weight (18.5–24.9) | 22 (45) | 4 (50) |
| Overweight (25–30) | 23 (47) | 4 (50) |
| Dietary diversity score | ||
| Low | 23 (47) | 4 (50) |
| High | 26 (53) | 4(50) |
| Household food insecurity | ||
| Secured | 17 (35) | 2 (25) |
| Insecure | 32 (65) | 6 (75) |
Private employee: a person who works for a private employer or in a private organization and receives regular remuneration in salary. 1 USD = 44.15 Ethiopian Birr, 2021. PLWH: people living with human immunodeficiency virus; ART: antiretroviral therapy; BMI: body mass index
In the bivariate analysis, age, income level, BMI, household food security, dietary diversity score, and self-management were factors associated with chronic comorbidity. During multivariable logistic regression analysis, being older and having a BMI of 25 kg/m2 or higher were significantly associated. The odds of having chronic comorbidity among PLWH were four times and eight times higher in age groups between 35 and 54 years [AOR = 3.54, 95% CI: (1.46, 8.74)] and ≥ 55 years [AOR = 7.66, 95% CI: (2.29, 25.50)], respectively, compared to younger adults. Compared to those who had BMI < 18.5 kg/m2 (underweight) and between 18.5 kg/m2 and 24.9 kg/m2 (normal), the odds of having chronic comorbidity were 3 times higher [AOR = 2.82, 95% CI: (1.00, 7.93)] than those having BMI greater than or equal to 25 kg/m2 (Table 4).
Factors associated with chronic comorbidity among adult ART patients of the public hospital in South Ethiopia, 2022
| Factor variable | Chronic comorbidity | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|
| Yes (n) | No (n) | |||
| Age | ||||
| 18–34® | 6 | 155 | 1 | 1 |
| 35–54 | 42 | 283 | 3.83 (1.59, 9.22) | 3.54 (1.46, 8.74)* |
| ≥ 55 | 7 | 27 | 6.69 (2.09, 21.46) | 7.66 (2.29, 25.50)* |
| Income level | ||||
| Low® | 22 | 240 | 1 | 1 |
| High | 33 | 225 | 1.60 (0.91, 2.83) | 1.11 (0.59, 2.06) |
| BMI | ||||
| Underweight (< 18.5)® | 5 | 73 | 1 | 1 |
| Normal weight (18.5–24.9) | 25 | 279 | 1.31 (0.48, 3.54) | 1.02 (0.36, 2.84) |
| Overweight (≥ 25) | 25 | 113 | 3.23 (1.18, 8.82) | 2.82 (1.00, 7.93)* |
| Household food security | ||||
| Food secured® | 19 | 98 | 1 | 1 |
| Food insecure | 36 | 367 | 1.98 (1.09, 3.59) | 1.94 (0.99, 3.78) |
| Dietary diversity score | ||||
| Low® | 26 | 259 | 1 | 1 |
| High | 29 | 206 | 1.40 (0.80, 2.46) | 1.27 (0.68, 2.38) |
| Self-management | ||||
| Low® | 37 | 368 | 1 | 1 |
| High | 18 | 97 | 1.85(1.01, 3.38) | 1.39 (0.69, 2.80) |
* Statistically significant variables in multiple logistic regressions at p-value ≤ 0.05; ® reference category. ART: antiretroviral therapy; COR: crude odds ratio; CI: confidence interval; AOR: adjusted odds ratio; BMI: body mass index
On a scale from 0 to 60, the total self-management score was 42 ± 3.92, which was the sum of the three domains, namely the daily self-management health practices (Domain 1), social support (Domain 2), and the chronic nature of HIV (Domain 3). Self-management scores were different for the separate domains of the questionnaire, and each domain was scored separately by taking the mean of all the items in that domain. Accordingly, the mean score for daily self-management health practices was 2.09 ± 0.57, the social support score was 1.69 ± 0.92, and the chronic nature of HIV score was 2.68 ± 0.43 (Figure 1). The low score in the social support domain group was mainly due to the two questions about social support groups, which are not very customary in Ethiopia.
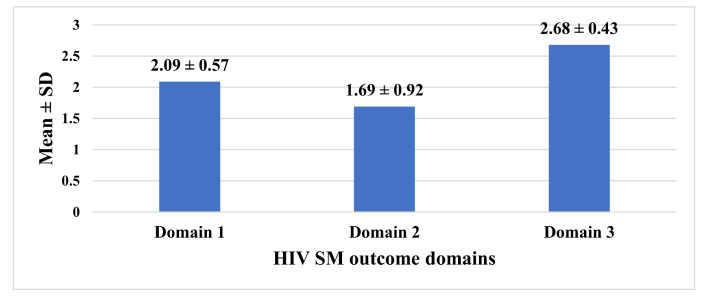
The mean result of each domain of self-management among adult PLWH in selected Hospitals of Southern Ethiopia, 2022 (n = 520). HIV: human immunodeficiency virus; SD: standard deviation; SM: self-management
The study was conducted with the aim of determining chronic comorbidity and self-management skills among adult PLWH. In the present study, the prevalence of hypertension and diabetes mellitus (chronic comorbidities) among adult PLWH was rather low. Chronic comorbidity has been associated with age, being overweight, or obesity. The total score for self-management was low, with the mean score for the social support domain being the lowest.
The current study’s estimated prevalence of hypertension was 9%, which is lower than studies conducted among HIV-positive individuals in other parts of Ethiopia, such as Jimma (34%) and Harar (12.7%) [28, 29]. It is also lower than the findings from Uganda (27.9%) [39]. The high percentage of young people (65% ≤ 40 years old) among our study participants could be one factor for the comparatively low hypertension prevalence. Aside from age, the length of therapy, the type of ART used, and the participants’ lifestyle could contribute to the discrepancy. To address this, more research using a longitudinal study design is needed.
In comparison to studies on adult PLWH in other parts of Ethiopia (Harar and Jimma), which showed a diabetes prevalence of 7.1% and 6.4%, respectively [28, 29], we also found a lower prevalence of diabetes (1.5%). However, other studies conducted in South Africa (1.3%) and Kenya (1.5%) [40, 41] showed comparable prevalences. Many cases of comorbidity with diabetes mellitus have been reported, particularly in places where the prevalence of HIV is high [42]. The observed disparity between the different studies could be due to differences in the participant characteristics that influence these disease conditions. These include variations in lifestyle, ART regimens, treatment duration, and age distribution of the HIV-infected individuals. To better understand the reason for this discrepancy, we recommend a follow-up study using a longitudinal study design.
In our study, chronic comorbidity was more prevalent among older PLWH, which is in line with study conducted in Northern Ethiopia [43]. The widespread availability of ART has significantly reduced AIDS-related mortality, thereby turning HIV into a chronic illness that lasts the rest of a patient’s life [44]. As a result, HIV patients who have access to ART are far more likely to live longer. However, aging poses a number of issues for HIV patients’ health, as age is associated with a number of comorbidities [45]. Furthermore, PLWH are obligated to use ART for the remainder of their lives, increasing the risk of chronic comorbidity [46]. Despite the fact that age is a non-modifiable risk factor, ART patients should receive regular follow-up and early intervention as part of their routine care, with special attention given to this group. Screening older PLWH for chronic comorbidity should be a priority for healthcare providers working in ART clinics.
Overweight people experienced greater chronic comorbidity than normal weight and underweight people, which is consistent with studies conducted in Nigeria [35]. It was also supported by a systematic review and meta-analysis of prospective cohort studies on obesity and comorbidity, which found a substantial association between the occurrence of chronic comorbidity and overweight and obesity [47]. According to the Veterans Aging Cohort Study [48], PLWH had a higher incidence of diabetes mellitus due to excess weight. Another study found that the actual number of overweight people among PLHIV is on the rise [44]. Because of urbanization in resource-limited countries, there is a shift toward consuming energy-dense foods, which may contribute to obesity [49]. Weight control programs in ART clinics, such as physical exercise and nutritional counseling, should be reinforced.
The total score of HIV self-management in the current study was lower than that of Webel et al. [50] in the United States. Attending support groups as an important part of their HIV self-management strategy and the helpfulness of educating others about HIV to stay in control of HIV are two elements where participants scored lower in self-management practice than others. Despite the fact that sub-Saharan African countries have the greatest HIV prevalence, self-management in this region is relatively new and poorly researched [31]. Furthermore, unlike in developed countries, chronic disease self-management programs, which are helpful in improving the self-management ability of PLWH, are not well-functioning [21, 51]. This difference highlights the need to seek an urgent implementation program on HIV self-management to improve the self-management ability of PLWH in Ethiopia.
Our study found that the second domain of the self-management scale, which assesses social support for people living with HIV (PLWH), had the lowest mean score (1.69 ± 0.92), consistent with findings from a study in the Liangshan area of China [52]. This domain includes critical elements such as social influence, emotional support, and cooperation with healthcare professionals, suggesting that a low score reflects inadequate support from both personal networks and healthcare providers. As a result, this lack of support can have a significant impact on the ability of PLWH to effectively manage their health and adhere to treatment regimens, which ultimately affects their overall well-being [38]. According to studies conducted in South Africa and Uganda [53, 54], more social contact improves the quality of life for people on ART. Informational, emotional, companionship, and instrumental assistance (including the provision of specific services to lessen client needs) are all ways that social support can help people cope with stress [55–57]. The current study area, Ethiopia, is known for strong social relationships, which makes this study finding paradoxical. The high presence of stigma and discrimination among PLWH in the study area [58] could be a plausible reason for this finding. More focus should be placed on mainstreaming actions aimed at preventing stigma and discrimination, and further research should be done on a new scale in each domain.
As a strength of our study, we would like to mention the fact that our data collectors were nurses and had expertise in HIV management. They could assist the participants in understanding and completing the questionnaires. They observed that the participants were being challenged to understand the different options in each item of the questionnaire. In particular, understanding the items of the self-management scale was reported to be challenging. Specifically, the difference between the ‘not applicable’ and ‘none of the time’ answer options was difficult. This probably led to the misunderstanding of the questions and may have resulted in measurement errors. In addition, the data-collectors reported that quite a few of the items were difficult to apply in an Ethiopian context. For example, attending social support groups is very uncommon in an Ethiopian setting, mostly because of the fear of stigma and discrimination. Therefore, we feel that developing a new questionnaire for self-management in a low-income setting is needed.
One limitation of this study is its exclusive focus on the prevalence of diabetes and hypertension, the two most common chronic comorbidities among PLWH. This narrow focus may overlook other significant chronic conditions that could affect the health and quality of life of this population, leading to an underestimation of the overall burden of chronic comorbidity among PLWH. Furthermore, the study’s design may limit the generalizability of the findings, as the relatively low expected prevalence of additional chronic conditions highlights the need for follow-up studies involving larger populations and extended follow-up periods. Such research is crucial for capturing a broader spectrum of chronic comorbidities, thereby enhancing our understanding of the health challenges faced by PLWH and informing more effective interventions and support strategies.
In conclusion, among adult PLWH, there was a relatively low prevalence of chronic comorbidity. Chronic comorbidity was more common in PLWH who were older and overweight. Despite the fact that the social support domain is the most essential aspect of HIV self-management and the current research area is recognized for strong social bonds, this domain is difficult in an Ethiopian setting. A self-management questionnaire that is tailored to the low-income setting is urgently needed in Ethiopia and other low-income countries to better assess the degree of self-management. In addition, we recommend additional research to explore the role of stigma and discrimination in the observed lack of interest in engaging in social support groups.
AOR: adjusted odds ratio
ART: antiretroviral therapy
BMI: body mass index
CI: confidence interval
HIV: human immunodeficiency virus
HUCSH: Hawassa University Comprehensive and Specialized Hospital
LMICs: lower and middle-income countries
PLWH: people living with human immunodeficiency virus
We thank Hawassa University, College of Medicine and Health Sciences, for providing funds for the study. We would also like to thank the data collectors and the study participants.
YTW: Conceptualization, Data curation, Formal analysis, Investigation, Writing—original draft, Writing—review & editing. SMB, RT, BS, AT, and MS: Conceptualization, Writing—review & editing. MRU and KTB: Writing—review & editing. All authors read and approved the final draft of the manuscript.
The authors declare that they have no conflicts of interest.
To comply with the Helsinki Declaration (2013) and the Population Screening Act, the study received ethical approval from the Hawassa University, College of Medicine and Health Sciences Institutional Review Board (IRB/216/2019) on May 7, 2019. Permission was obtained from the hospital management. Participation was determined by the person without any external influence to participate or not. Before the data collection, informed written consent (signed or verified by fingerprint) was taken from the study subjects. The data was collected and analyzed anonymously.
The informed consent to participate in the study was obtained from all participants.
Not applicable.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
This research work was financed by the research office of Hawassa University, College of Medicine and Health Sciences, Ethiopia. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
© The Author(s) 2025.
Open Exploration maintains a neutral stance on jurisdictional claims in published institutional affiliations and maps. All opinions expressed in this article are the personal views of the author(s) and do not represent the stance of the editorial team or the publisher.
Copyright: © The Author(s) 2025. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 2401
Download: 29
Times Cited: 0
Violetta Vlasova ... Konstantin Shmagel
Zhimin Huang, Xiaohui Wang
Werner Krause
Yun-Meng Yan ... Qi-Wen Yang
Yang Zhou ... Hongzhou Lu
