Affiliation:
1Division of Pediatric Cardiology, Department of Pediatrics, University of Tennessee Health Science Center, Le Bonheur Children’s Hospital, Memphis, TN 38103, USA
Email: eharve12@uthsc.edu
ORCID: https://orcid.org/0009-0005-7234-1925
Affiliation:
2Division of Pediatric Nephrology, Department of Pediatrics, University of Tennessee Health Science Center, Le Bonheur Children’s Hospital, Memphis, TN 38103, USA
Affiliation:
1Division of Pediatric Cardiology, Department of Pediatrics, University of Tennessee Health Science Center, Le Bonheur Children’s Hospital, Memphis, TN 38103, USA
ORCID: https://orcid.org/0000-0002-4448-9325
Affiliation:
3Department of Anesthesiology, University of Missouri Kansas City, St. Luke’s Hospital of Kansas City, Kansas City, MO 64111, USA
Affiliation:
4Department of Pediatric Surgery, McGovern Medical School at the University of Texas Health Science Center at Houston, Houston, TX 77030, USA
Affiliation:
1Division of Pediatric Cardiology, Department of Pediatrics, University of Tennessee Health Science Center, Le Bonheur Children’s Hospital, Memphis, TN 38103, USA
ORCID: https://orcid.org/0000-0002-0464-7747
Affiliation:
1Division of Pediatric Cardiology, Department of Pediatrics, University of Tennessee Health Science Center, Le Bonheur Children’s Hospital, Memphis, TN 38103, USA
ORCID: https://orcid.org/0000-0003-3748-0215
Explor Cardiol. 2024;2:40–48 DOI: https://doi.org/10.37349/ec.2024.00020
Received: December 30, 2023 Accepted: February 20, 2024 Published: April 06, 2024
Academic Editor: Maria Grazia Andreassi, CNR Institute of Clinical Physiology, Italy
The article belongs to the special issue Environmental Cardiology
Aim: Cardio-ankle vascular index (CAVI) is a marker of arterial stiffness independent of blood pressure (BP) at the time of measurement. This work sought to evaluate the association of CAVI with left ventricular hypertrophy (LVH), a marker of long-standing hypertension (HTN) in the pediatric population.
Methods: CAVI values from 236 children being evaluated for HTN were compared with their BP grade (normal, elevated, stage I HTN, and stage II HTN) in accordance with clinical guidelines. CAVI values were correlated to the presence of LVH and lipid profiles. One hundred seven of the studied patients had transthoracic echocardiograms available for comparison, and 126 had available lipid results. CAVI means between the groups were compared using analysis of variance.
Results: There was no significant difference in CAVI values between the BP groups [median/interquartile range: normal BP (4.95/4.4–5.7), elevated BP (5.1/4.5–5.6), stage I/II HTN (5.0/4.3–5.5)]. Mean CAVI value was higher in the group that had LVH (5.53, standard deviation = 1.4 vs. 5.1, standard deviation = 1; P = 0.13) but was not statistically significant. However, higher mean CAVI value in children ≥ 15 years was significantly associated with the presence of LVH (5.9, standard deviation = 1.8 vs. 5.2 standard deviation = 0.8; P = 0.018).
Conclusions: In post-pubertal children, CAVI may be a good predictor of LVH from long-standing HTN. This tool could prove useful in screening for the presence of atherosclerotic changes and provide opportunity for intervention/improved long-term outcomes.
Hypertension (HTN) in the pediatric population has long been recognized as a diagnostic challenge to clinicians [1–3]. Further, despite recent successful efforts to simplify/optimize screening and management guidelines [4, 5], consistent and effective management of HTN in this age group remains challenging. While this is due in part to the complex diagnostic standard for pediatric HTN [average systolic and/or diastolic blood pressure (BP) that is ≥ 95th percentile for gender, age, and height on three or more separate occasions [4]], another shortcoming on the part of medical providers is failure to educate on the implications of the diagnosis once it has been made [5, 6]. This becomes understandable when one considers that despite the known association between pediatric HTN and end organ damage [left ventricular hypertrophy (LVH), chronic kidney injury, etc.] [7, 8], there still exists a gap in published data identifying a specific threshold of pediatric BP in childhood that predicts adverse cardiovascular outcomes in adulthood [3]. In short, it is difficult to motivate a patient or family experiencing no symptoms to modify his or her lifestyle in a meaningful way without a definitive endpoint that merits avoidance.
Arterial stiffness—or a loss of vascular elasticity—has been shown in the adult population to be an independent predictor of morbidity and mortality in adult hypertensive patients [9]. As it has been shown the atherosclerotic process begins in childhood, interest has grown in assessing the early stages of arterial stiffness in the pediatric population [10, 11]. Studies have reported positive correlation with increased measures of arterial stiffness in pediatric patients exhibiting atherosclerotic risk factors such as obesity and HTN [12, 13]. While certain laboratory markers have been shown to correlate with the atherosclerotic process [14–17], greater clinical interest exists in the utilization of physical measures of arterial stiffness in the care of at-risk patients. Cardio-ankle vascular index (CAVI) is a measure of arterial stiffness that has been shown to be a promising tool aiding in prediction of cardiovascular disease risk [18–20]. It also has the added benefit of being unaffected by changes in BP during time of measurement [21]. This is of particular importance in measurement of pediatric BP which may be affected to a greater extent by white coat HTN [22]. Reference values for CAVI in the pediatric population have been proposed [23] and adolescent patients with essential HTN have been found to exhibit increased CAVI values [24].
This study sought to assess the utility of CAVI as a predictor of end-organ damage in the form of LVH in pediatric patients with HTN. CAVI values in the patient population were also compared against absolute BP measurements to confirm independence from influence. Lastly, CAVI values in these patients were compared against lipid profiles as certain derangements in these lab values have been shown to predict arterial stiffness [25]. The hypothesis was that CAVI values would be higher in those with LVH and dyslipidemia but not correlate specifically with instantaneous BP measurement.
This was a single center, retrospective review of patients evaluated in outpatient Nephrology and Cardiology clinics at our institution referred for evaluation of HTN who had undergone CAVI measurement as part of their comprehensive assessment from 2013–2016. CAVI values were measured at initial visit. Prior to data collection, approval was obtained from the University of Tennessee Health Science Center institutional review board. All patients meeting the pediatric age criterion (age 21 or less) evaluated in these clinics within this time frame and having at least CAVI and BP measurements for assessment were included in our analysis. Patients with any complex congenital heart disease having undergone surgical intervention of the native aorta or those exhibiting hypertensive emergency at time of assessment were excluded.
To calculate CAVI, heart sounds, electrocardiography, and brachial/ankle pulsations are simultaneously measured (Figure 1). Pulse wave velocity is calculated from distance and time of a single aortic pulse propagation from the aortic valve origin to the ankle. Measured variables are then input to a modified Bramwell-Hill equation to yield unitless CAVI values [21, 26]. The VaSera (VS-1500) device (Fukuda Denshi Company, Tokyo, Japan) was used in this study to determine left and right arm CAVI values from included patients and the averaged value was used for analysis.
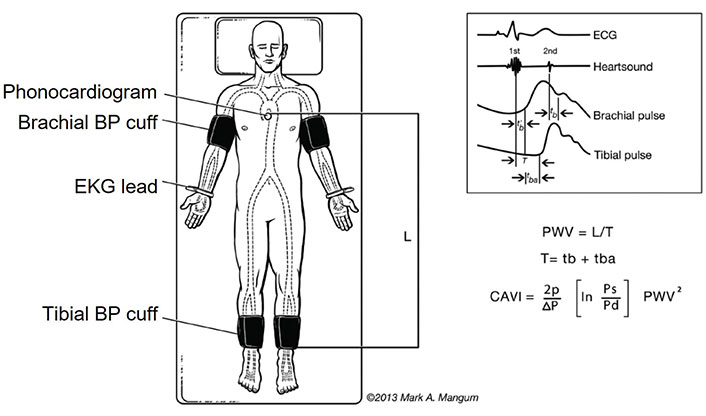
CAVI measurement technique. PWV: pulse wave velocity; L: distance from aortic valve to ankle; T: time from pulse wave propagation from aortic valve to ankle; p: blood viscosity; Ps: systolic BP; Pd: diastolic BP; ΔP: Ps – Pd; ECG: electrocardiogram; tb: time from aortic valve closure to the notch of brachial pulse wave; tba: time from the rise of brachial pulse wave to the rise of ankle pulse wave; t’b: time from aortic valve opening to the rise of brachial pulse wave. © 2013 Mark A. Mangum, reprinted with permission [26]
Per routine clinic intake vitals protocol, auscultatory BP was measured in right upper extremity with appropriate-sized cuff with patient sitting upright. Patients were categorically grouped by BP grade (normal BP, elevated BP, stage I HTN, and stage II HTN) in accordance with most recent 2017 American Academy of Pediatrics clinical guidelines [4]. Patients were assessed across all ages initially and then separately into pre- and post-pubertal age groups. Fifteen years was used as the threshold between pre- and post-pubertal age groups as this would reasonably separate the cohorts in lieu of recorded Tanner staging (a limitation of the retrospective nature of the study). For each included patient, the electronic medical record was reviewed for the presence of a transthoracic echocardiogram (TTE) and/or lab evaluation including lipid profile performed as part of their comprehensive HTN evaluation having been performed within one year of the CAVI measurement (on occasion, TTE and lab evaluation was not feasible on same day as initial evaluation/CAVI measurement). LVH was measured from the TTE by M-mode according to American Society of Echocardiography guidelines and defined as a left ventricular mass index of > 48 g/m2.7 [27, 28]. Low density lipoprotein (LDL) levels were grouped as: normal < 100 mg/dL, borderline 100–130 mg/dL, and elevated > 130 mg/dL. Total cholesterol (TC) was considered elevated if > 200 mg/dL and triglyceride (TG)/high density lipoprotein (HDL) ratio was considered elevated if > 2.5.
Mean and median CAVI values were calculated for all groups and means between the groups were compared using analysis of variance.
There were 236 patients (ages 4–21) who met inclusion criteria for analysis within the studied time frame of 2013–2016 (Table 1). Of the studied patients, 142 were male (60%) and 112 (47%) were < 15 years of age at the time of CAVI/BP measurement. One hundred seven (45%) of the studied patients had a TTE for review and 126 (53%) patients had undergone laboratory evaluation including lipid panel.
Patient demographics
| Demographics | N | Percentage | |
|---|---|---|---|
| Age | < 15 years | 112 | 47% |
| ≥ 15 years | 124 | 53% | |
| Gender | Male | 142 | 60% |
| Female | 94 | 40% | |
| BMI percentile | < 85th | 96 | 41% |
| 85th–95th | 29 | 12% | |
| > 95th | 111 | 47% | |
Of the 236 patients evaluated, 70% had an abnormal BP at initial consultation visit (27% with an elevated BP and 43% with stage I/II HTN). There was no significant difference in CAVI values between the BP groups (mean: normal BP—4.94, elevated BP—5.12, stage I/II HTN—5.05; P = 0.70) even when considering the patient cohort > 15 years of age (Table 2).
Comparison of CAVI with BP group
| BP group | N | Mean CAVI | Median (IQR) | P-value | |
|---|---|---|---|---|---|
| BP group (all ages) | Normal | 70 | 4.94 | 5.0 (4.4–5.7) | 0.7 |
| Elevated | 64 | 5.12 | 5.1 (4.5–5.6) | ||
| Stage I/II HTN | 102 | 5.05 | 5.0 (4.3–5.5) | ||
| BP group (> 15 years) | Normal | 22 | 5.40 | 5.33 (4.7–6.2) | 0.9 |
| Elevated | 31 | 5.48 | 5.40 (5.3–6.0) | ||
| Stage I/II HTN | 57 | 5.38 | 5.20 (4.7–5.9) | ||
IQR: interquartile rage
In the cohort of patients (n = 107) that had a TTE performed, 17% (n = 18) were noted to have LVH (Table 3). Across all ages, the mean CAVI values were higher in the group that exhibited LVH (5.5, standard deviation = 1.4 vs. 5.1, standard deviation = 1; P = 0.13), but it was not statistically significant. However, when assessing children 15 years and above, higher mean CAVI value was significantly associated with the presence of LVH (5.9, standard deviation = 1.8 vs. 5.2 standard deviation = 0.8, P = 0.018). Of the 64 children (> 15 years), 7 of the 19 with a CAVI value > 5.9 had LVH in comparison to 6 of the 45 with a CAVI value ≤ 5.9 (odds ratio 3.79 [1.06,13.47], P = 0.019). A CAVI score > 5.9 in predicting LVH was only 53.85% sensitive but had good specificity of 76.47% and a negative predictive value of 86.67%.
Comparison of CAVI with LVH and lipid profile
| Comparison group | N | Mean CAVI | Median (IQR) | P-value | |
|---|---|---|---|---|---|
| LVH (all ages) | < 48 g/m2.7 | 89 | 5.1 | 5.0 (4.3–5.7) | 0.13 |
| > 48 g/m2.7 | 18 | 5.53 | 5.3 (4.6–6.2) | ||
| LVH (> 15 years) | < 48 g/m2.7 | 51 | 5.21 | 5.2 (4.6–5.9) | 0.018* |
| > 48 g/m2.7 | 13 | 5.95 | 6.1 (4.9–6.4) | ||
| LDL | < 100 g/dL | 74 | 4.93 | 5.4 (5–5.95) | 0.77 |
| 100–130 g/dL | 26 | 5.05 | 5.3 (4.6–6.0) | ||
| > 130 g/dL | 26 | 5.07 | 5.0 (4.6–5.7) | ||
| TC | < 200 g/dL | 95 | 4.96 | 5.0 (4.3–5.5) | 0.63 |
| > 200 g/dL | 31 | 5.06 | 5.1 (4.6–5.6) | ||
| TG/HDL (all ages) | < 2.5 | 77 | 5.04 | 5.0 (4.5–5.6) | 0.39 |
| > 2.5 | 49 | 4.89 | 4.7 (4.2–5.4) | ||
| TG/HDL (> 15 years) | < 2.5 | 41 | 5.42 | 5.4 (4.9–5.9) | 0.72 |
| > 2.5 | 22 | 5.34 | 5.2 (4.7–5.6) | ||
* Statistically significant (P < 0.05)
Among the 126 patients that had a lipid panel performed, 41% (n = 52) had an abnormal LDL level (> 100 mg/dL), 25% (n = 31) an abnormal TC (> 200 mg/dL), and 39% (n = 39) had an abnormal TG/HDL ratio (> 2.5). There was no significant difference between mean CAVI values for the groups of LDL (4.9, standard deviation = 1.0 vs. 5.1, standard deviation = 1.0 vs. 5.1, standard deviation = 1.0; P = 0.77) or when considering TC (5.0, standard deviation = 1.1 vs. 5.1, standard deviation = 0.7; P = 0.63). TG/HDL ratio groups similarly did not exhibit statistically significant different mean CAVI values (5.0, standard deviation = 0.9 vs. 4.9, standard deviation = 1.1; P = 0.39) even when considering children 15 years and above (5.4, standard deviation = 0.9 vs. 5.3, standard deviation = 0.9; P = 0.72).
The ability to characterize vascular stiffness accurately and non-invasively in the pediatric population (especially in patients exhibiting early atherosclerotic risk factors) could prove tremendously useful to clinicians. Not only would this provide opportunity for aggressive early intervention and prevention of adverse long-term outcomes, but it would arm pediatricians (both primary and subspecialists) with objective data to aid in education/counseling on the importance of lifestyle modification in this time period when it would prove most beneficial. Since the introduction of CAVI as a potential measure of vascular stiffness [21], studies have sought to prove/disprove its claim of being truly BP-independent [29, 30]. Our data would suggest that in this patient population, CAVI values are indeed independent of BP at the time of measurement as there was no significant difference in mean CAVI values amongst the normal, elevated, and stage I/II HTN groups. This independence from instantaneous BP measurement makes CAVI particularly appealing in the pediatric population where white coat HTN is prevalent and daytime systolic BP variability has been shown to correlate with LVH [31].
Being assured that CAVI can be interpreted reliably as BP-independent becomes particularly important when considering our results that suggest elevated CAVI does indeed predict the presence of LVH. All of the 18 studied patients whose echocardiograms exhibited LVH had BP at the time of CAVI measurement that fell in the elevated or stage I/II HTN groups. Echocardiographic evidence of the end-organ effect of long-standing HTN serves to confirm that the elevated CAVI values measured in these patients are a true reflection of vascular changes and not the result of instantaneous BP effect. We feel that the strong negative predictive value of a CAVI value < 5.9 in the post-pubertal age may be a useful tool for the clinician when deciding the need for an echocardiogram for LVH in children being evaluated for HTN. Further, though this same result was not proven to be statistically significant in the < 15 years age group, the trend was similar with a higher CAVI value in those with LVH. This may be related to the lesser duration of exposure to HTN in younger children or pubertal changes in older children. This could potentially be due to the relatively small sample size of this study and presents an opportunity for further study of increased utilization of CAVI in this patient population.
When considering these results, once diagnosed with LVH, there may be a role for CAVI as a tool to serially follow CAVI values in the same patient to assess the response to interventions such as diet, exercise, or medications. This may preclude the need for serial TTE assessments which add a significant cost and time burden to the patient and family. The average time for measuring CAVI is 3–5 min with an expertise requirement similar to what is needed for obtaining routine vital signs. Further, while the diagnostic importance of ambulatory BP monitoring (ABPM) in the pediatric population cannot be denied [32], having an adjuvant in-office testing modality to follow such serial changes after initiation of treatment is appealing. This becomes especially enticing when considering that regular access to ABPM is often limited to both pediatric primary care physicians and pediatric subspecialists [33].
We did not observe higher CAVI values in those of our studied population who exhibited dyslipidemia in the form of an elevated LDL, TC, or TG/HDL ratio. Increased vascular stiffness has been previously reported in pediatric patients exhibiting similar lipid abnormalities [25]. This observation may be due to our use of CAVI as the measure of vascular stiffness whereas this previous work utilized more traditional measures of vascular stiffness, pulse wave velocity and augmentation index. The authors of this study mention that their observed association was particularly prominent in the obese youth population. This stands in contrast to data we have previously reported that describes an inverse relationship between CAVI values and body mass index, thought to reflect vascular adaptations to the state of obesity seen in the early years of life [34]. It is assumed, however, that these protective vascular changes do not persist in the face of long-standing obesity and that—eventually—vascular stiffness (and thus CAVI values) would increase over time as is observed in the adult population [35]. Studies investigating the effect of dyslipidemia on arterial stiffness in the pediatric population are few, however, likely due to the difficult, arduous nature of longitudinal observational studies that would provide the best insights.
This study is inherently limited by its retrospective nature and relatively small sample size. Ideally, this work would be conducted in a controlled, prospective manner to ensure all studied subjects undergo all studied testing modalities (echocardiography, lipid screening, etc.). However, even considering its retrospective nature, we feel the results still provide useful insight to the utility of CAVI in this patient population. As a relatively quick and easy tool with limited expertise requirements, it does pose as a potential “6th vital sign” which can be used at scale for larger prospective, longitudinal studies to investigate changes in vascular stiffness as measured by CAVI over time with increasing age, development of LVH in the setting of long-standing HTN, and evolving lipid profiles. This would provide greatest insight into the applicability of this testing modality as a screening tool in our patient population.
In conclusion, CAVI remains a BP-independent measure of vascular stiffness that shows great potential for use in the pediatric population. In post-pubertal (and likely all aged) children, CAVI may be a good predictor of LVH from long-standing HTN. This tool could prove useful in screening for the presence of atherosclerotic changes early in their course and provide opportunity for intervention and improved long-term outcomes.
BP: blood pressure
CAVI: cardio-ankle vascular index
HDL: high density lipoprotein
HTN: hypertension
LDL: low density lipoprotein
LVH: left ventricular hypertrophy
TC: total cholesterol
TG: triglyceride
TTE: transthoracic echocardiogram
EH: Conceptualization, Investigation, Formal analysis, Writing—original draft, Writing—review & editing. NDS, NZ, BH, and RN: Conceptualization, Investigation. BA: Conceptualization, Supervision, Writing—review & editing. RP: Conceptualization, Investigation, Formal analysis, Supervision, Writing—review & editing.
The authors declare that they have no conflicts of interest.
Approval for this study was obtained from the University of Tennessee Health Science Center institutional review board. This study was in compliance with the Declaration of Helsinki.
Written informed consent to participate was appropriately obtained from all participants or their patients/legal guardians for children under 16.
Not applicable.
The raw data supporting the conclusions of this manuscript will be made available by the authors, without undue reservation, to any qualified researcher.
Not applicable.
© The Author(s) 2024.
Copyright: © The Author(s) 2024. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Francesca Gorini, Alessandro Tonacci
Maria Grazia Andreassi
