Affiliation:
1Department of Pulmonology and Respiratory, Faculty of Medicine, Hasanuddin University, Makassar 90245, Indonesia
Email: noormeywardhani@gmail.com
Affiliation:
1Department of Pulmonology and Respiratory, Faculty of Medicine, Hasanuddin University, Makassar 90245, Indonesia
2Wahidin Sudirohusodo General Hospital, Makassar 90245, Indonesia
ORCID: https://orcid.org/0000-0003-4125-005X
Affiliation:
1Department of Pulmonology and Respiratory, Faculty of Medicine, Hasanuddin University, Makassar 90245, Indonesia
2Wahidin Sudirohusodo General Hospital, Makassar 90245, Indonesia
Affiliation:
1Department of Pulmonology and Respiratory, Faculty of Medicine, Hasanuddin University, Makassar 90245, Indonesia
2Wahidin Sudirohusodo General Hospital, Makassar 90245, Indonesia
ORCID: https://orcid.org/0000-0002-2424-0178
Affiliation:
1Department of Pulmonology and Respiratory, Faculty of Medicine, Hasanuddin University, Makassar 90245, Indonesia
2Wahidin Sudirohusodo General Hospital, Makassar 90245, Indonesia
ORCID: https://orcid.org/0000-0003-1778-2507
Affiliation:
1Department of Pulmonology and Respiratory, Faculty of Medicine, Hasanuddin University, Makassar 90245, Indonesia
Explor Med. 2025;6:1001327 DOI: https://doi.org/10.37349/emed.2025.1001327
Received: July 16, 2024 Accepted: April 02, 2025 Published: May 28, 2025
Academic Editor: Evgeny Imyanitov, N.N. Petrov Research Institute of Oncology, Russia
The article belongs to the special issue Molecular Diagnostics in Oncology
Aim: This study was conducted to analyse the ability of Vascular Endothelial Growth Factor (VEGF) in serum and bronchial wash as a diagnostic biomarker of Non-small Cell Lung Carcinoma (NSCLC).
Methods: This study used an analytic observational study with a cross-sectional design in lung cancer patients. For each study subject, serum and bronchial wash samples were collected, and VEGF levels were tested using the Enzyme-Linked Immunosorbent Assay (ELISA) method. The receiver operating characteristic (ROC) curve analysis was performed to assess the ability of VEGF as a diagnostic biomarker by determining the area under the curve (AUC). Then the best cut-off value will be determined using the Youden Index formula to evaluate the sensitivity and specificity of VEGF to diagnose NSCLC.
Results: The research subjects consisted of 110 participants, consisting of 75 NSCLC patients and 35 controls. This study found that bronchial wash and serum levels of VEGF in patients with NSCLC were higher than those in the control group (p = 0.010 and p < 0.001). Statistical analysis showed a positive correlation between serum VEGF and bronchial wash VEGF in NSCLC (r = 0.235; p = 0.021). The results of the ROC curve analysis showed a fairly good diagnostic ability for VEGF with an AUC value of 0.653 for bronchial wash VEGF and 0.709 for serum VEGF.
Conclusions: The results of this study found that VEGF has a crucial role in NSCLC patients. Increased expression of VEGF in NSCLC patients, both in serum and bronchial wash, has the potential to be used as a diagnostic biomarker for NSCLC patients.
Lung cancer encompasses malignancies originating from the lungs (primary) and malignancies from outside the lungs that metastasize to the lungs (metastases). Globally, lung cancer is estimated at 2.2 million new cases and 1.8 million deaths in 2020 [1, 2]. Based on the classification of the World Health Organisation (WHO), lung cancer is divided into two histological types, namely small cell lung cancer (SCLC) and non-SCLC (NSCLC), which incidence rate is around 80–85% of all lung cancer and has a worse outcome. Early diagnosis and prompt treatment will have an impact on the prognosis and outcomes of lung cancer patients. Patients with advanced lung cancer have a poor prognosis with an estimated 5-year relative survival of only 5.2%. Therefore, early detection of lung cancer will be very important to reduce the death rate due to lung cancer, especially in NSCLC [3–5].
Recent scientific evidence on the biomolecular pathways of lung cancer has revealed several important mediators of tumour function, one of which is angiogenesis, which is thought to play a role in tumour growth and spread. The main mediator that drives this process is Vascular Endothelial Growth Factor (VEGF). In lung cancer, activation of the VEGF pathway plays an important role in building a blood vessel supply in the tumour [6]. The role of VEGF in lung cancer growth causes an increase in VEGF levels in the blood and tissue around the lungs, which has the potential to be a biomarker in diagnosing lung cancer. Overexpression of VEGF and/or high serum levels of VEGF have been reported in both SCLC and NSCLC patients [6, 7].
Matsuyama et al. [8] in their research reported that serum VEGF levels increased significantly according to the stage and progression of lung cancer. In addition, Cao et al. [9] assessed VEGF in bronchial wash fluid for differential diagnosis of primary lung cancer and found that VEGF in bronchial wash fluid was significantly higher than VEGF in plasma. Based on these studies, it was hypothesised that serum VEGF and bronchial wash could be diagnostic markers of NSCLC. This study aims to analyse the levels of serum VEGF and bronchial wash in NSCLC patients and examine their ability as diagnostic markers of NSCLC. This study also attempts to calculate the cut-off value of serum VEGF and bronchial wash levels as diagnostic markers of NSCLC.
This research is an analytical observational study with a cross-sectional design on cancer patients who were hospitalised at Wahidin Sudirohusodo General Hospital and underwent bronchoscopy in August until December 2023. The participants in this study were taken consecutively during the research period. The inclusion criteria for the research participants were adult patients aged ≥ 18 years, patients who underwent bronchoscopy procedures, and patients who were willing to take part in the research by signing an informed consent. Patients who have received previous lung cancer therapy or have a history of other cancers will be excluded from this study.
We divided the participants into two groups, the NSCLC group and the control group, to then compare the serum VEGF and bronchial wash levels. The diagnosis of NSCLC in patients was confirmed by cytology/histology examination by the Pathology Department of Wahidin Sudirohusodo General Hospital, as well as to determine the stage using classification based on the Union for International Cancer Control (UICC)/The American Joint Committee on Cancer (AJCC) [10]. The control patients in this study were patients with other lung diseases (non-lung cancer), such as those with infectious complications, bronchiectasis, and others that have complaints similar to NSCLC (coughing, coughing up blood, and shortness of breath).
We examined VEGF levels using two samples: serum and bronchial wash fluid. Serum was taken from the blood from the median cubital vein and then allowed to clot for 5 minutes at room temperature and centrifuged for 5 minutes at 3,000 rotations per minute (rpm); then the serum was separated from other blood components. Bronchial wash fluid samples were taken from bronchoscopy and then centrifuged for 10 minutes at a speed of 2,000 rpm. The collected samples are stored in the Sample Bank at Hasanuddin University Medical Research (HUM-RC) at a temperature of –80˚C [11]. All samples were collected before the patients received any previous therapy or intervention to avoid biasing the results.
Examination of VEGF levels from blood and bronchial wash fluid was carried out using the Enzyme-Linked Immunosorbent Assay (ELISA) method using a spectrophotometer with a wavelength of 450 nm to calculate VEGF-A levels in pg/mL (Human ELISA kit, No. LS-F10515) [11]. The VEGF examination process is also carried out at Hasanuddin University Medical Research (HUM-RC).
The data that has been collected is then tabulated into Microsoft Excel. Data analysis used Statistical Package for the Social Sciences (SPSS) software. The data normality test is carried out for all numerical data to determine the type of data analysis that will be used. The t-independent test is used to compare numerical data between two groups if the data is normally distributed; otherwise, the Mann-Whitney test will be carried out. If there are more than two groups that want to be compared, the ANOVA test will be used if the data is normally distributed; if not, the Kruskal-Wallis test will be used. Chi-square analysis was used to assess the relationship between variables and categorical data. The correlation test uses Pearson correlation if the data is normally distributed; otherwise, the Spearman test will be used. In addition, receiver operating characteristic (ROC) curve analysis was performed to assess the ability of VEGF as a diagnostic biomarker by assessing the area under the curve (AUC). Then the best cut-off value will be determined using the Youden Index formula. The results of data analysis are then presented in tabular and graph form and combined with making several models of the existing variables accompanied by explanations.
This study received ethical clearance from Hasanuddin University Faculty of Medicine Ethics Commission (No.692/UN.4.6.4.5.31/PP36/2023).
A total of 110 patients who met the inclusion criteria participated as subjects in this study, consisting of 75 NSCLC patients and 35 control patients. The average age of the research subjects was 52.85 years. In this study, there was a significant difference between the ages of NSCLC patients and control patients. The mean age in NSCLC patients was significantly higher compared to control patients. A significant relationship was also found between the patient’s smoking status and the degree of smoking based on the Brinkman with the incidence of NSCLC; as many as 60% of NSCLC patients were smokers, with 40% of them being severe smokers, whereas in the control group only 31.4% were smokers (Table 1).
Characteristics of Subjects
| Characteristics | Mean ± SD/Frequency (%) | p-value | ||
|---|---|---|---|---|
| NSCLC | Control | Total | ||
| Age (years) | 58.49 ± 11.23 | 40.77 ± 15.57 | 52.85 ± 15.16 | < 0.001* |
| 18–50 years old | 9 (12%) | 20 (57.1%) | 29 (26.4%) | < 0.001# |
| > 50 years old | 66 (88%) | 15 (42.9%) | 81 (73.6%) | |
| Gender | ||||
| Male | 50 (66.7%) | 21 (60%) | 71 (64.5%) | 0.496# |
| Female | 25 (33.3%) | 14 (40%) | 39 (35.5%) | |
| Smoking status | ||||
| Active smoker | 45 (60%) | 11 (31.4%) | 56 (50.9%) | 0.001# |
| Passive smoker | 17 (22.7%) | 3 (8.6%) | 20 (18.2%) | |
| Non smoker | 13 (17.3%) | 21 (60%) | 34 (30.9%) | |
| Brinkman indexa | ||||
| Mild smoker | 12 (26.6%) | 8 (72.8%) | 20 (18.2%) | 0.015# |
| Moderate smoker | 15 (33.4%) | 2 (18.2%) | 17 (15.4%) | |
| Severe smoker | 18 (40%) | 1 (9%) | 19 (17.2%) | |
| Comorbidityb | ||||
| Tuberculosis | 24 (32%) | 18 (51.4%) | 42 (38.2%) | - |
| Malignancy | 2 (2.7%) | 1 (2.6%) | 3 (2.7%) | |
| Diabetes mellitus | 10 (13.3%) | 7 (20%) | 17 (15.4%) | |
| Hypertension | 19 (25.3%) | 5 (14.3%) | 24 (21.8%) | |
a Subject of an active smoker; b subjects with the mentioned disease; * t-independent test; # chi-square test; SD: standard deviation; NSCLC: Non-small Cell Lung Carcinoma; -: not calculable
Participants in this study consisted of a total of 71 male patients (64.5%) and 39 female patients (35.5%); the male gender dominated both the NSCLC group (66.7%) and the control group (60%), and there is no significant difference between the genders of the two groups. Based on the comorbidities of the participants, the majority had tuberculosis in 42 subjects (38.2%), diabetes mellitus in 17 subjects (15.4%), hypertension in 24 subjects (21.8%), and a family history of malignancy in 3 subjects (2.7%) (Table 1).
Comparison of VEGF levels between the NSCLC patients group and the control group showed that both bronchial wash fluid and serum VEGF levels in NSCLC subjects were higher than in control subjects. Bronchial wash fluid VEGF levels in NSCLC patients were (675.45 ± 738.1 pg/mL), while control subjects were only (316.03 ± 188.4 pg/mL). Serum VEGF levels in NSCLC subjects were found to be (834.51 ± 653.1 pg/mL), whereas in control subjects they were (416.19 ± 272.7 pg/mL). Comparison of bronchial wash VEGF values showed that bronchial wash VEGF levels in NSCLC patients were significantly higher (p = 0.010). Likewise, serum VEGF levels in NSCLC patients were significantly higher compared to control subjects (p < 0.001) (Table 2).
Comparison of VEGF levels between the NSCLC and control groups
| Group | Bronchial Wash VEGF | Serum VEGF | ||
|---|---|---|---|---|
| Mean ± SD (pg/mL) | p-value | Mean ± SD (pg/mL) | p-value | |
| NSCLC | 675.45 ± 738.1 | 0.010 | 834.51 ± 653.1 | < 0.001** |
| Control | 316.03 ± 188.4 | 416.19 ± 272.7 | ||
VEGF: Vascular Endothelial Growth Factor; NSCLC: Non-small Cell Lung Carcinoma; SD: standard deviation; ** Mann-Whitney test
The correlation test between bronchial wash VEGF values and serum VEGF is shown in Table 3. The results indicate that there is a significant positive correlation (r = 0.235; p = 0.021) between bronchial wash VEGF levels and serum VEGF levels. This shows that the higher the serum VEGF level, the higher the bronchial wash VEGF level in NSCLC patients (Table 3).
Correlation between bronchial wash fluid VEGF and serum VEGF in NSCLC patients
| Variable | Mean ± SD | Spearman Correlations | |
|---|---|---|---|
| r | p-value | ||
| Bronchial wash VEGF | 675.45 ± 738.1 | 0.235 | 0.021 |
| Serum VEGF | 834.51 ± 653.1 | ||
VEGF: Vascular Endothelial Growth Factor; NSCLC: Non-small Cell Lung Carcinoma; SD: standard deviation
The results of the ROC curve analysis showed that the AUC value for the bronchial wash VEGF variable was 0.653, and serum VEGF was 0.709. This shows that both have good abilities in diagnosing NSCLC, but serum VEGF is better compared to bronchial wash VEGF (Figure 1).
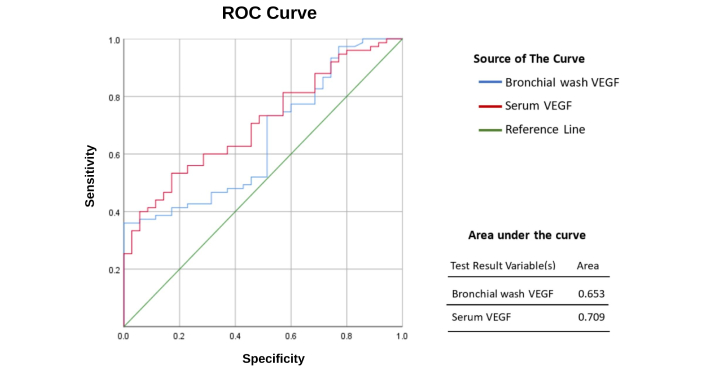
ROC curve analysis of serum and bronchial wash VEGF to diagnose NSCLC. ROC: receiver operating characteristic; VEGF: Vascular Endothelial Growth Factor; NSCLC: Non-small Cell Lung Carcinoma
Determining the best cut-off value is assessed using the Youden Index. The results showed that the best cut-off value for bronchial wash VEGF was 667.17 pg/mL with a sensitivity value of 36% and specificity of 100%, while the best cut-off value for serum VEGF was 640.42 pg/mL with a sensitivity value of 53.3% and specificity of 82.9%.
This study is the first study in Indonesia to assess the effect of VEGF as a biomarker in NSCLC patients. What is more interesting is that this study not only uses serum VEGF but also assesses the potential of VEGF in bronchial wash as a biomarker in NSCLC patients. We think this study is important to reveal the role of VEGF in NSCLC more comprehensively. The results of this study certainly provide a real view of the potential of VEGF as a biomarker in NSCLC patients.
The results of this study found that the mean age of the NSCLC group is 58.49, dominated by age > 50 years (88%). This is different from the control group, with a mean age of 40.77 years, with the predominance being in the age range 18–50 years. The age difference between the NSCLC and control groups was found to be statistically significant. Age is a risk factor for lung cancer and NSCLC [12]. The study by Putra et al. [13] states that the majority of NSCLC sufferers are in the age group 41–60 years. This is in line with several previous studies which stated that the incidence of lung cancer above 45 years of age increases significantly [14]. Older age is associated with the risk of lung cancer, which is caused by continuous shortening of telomeres during repeated cell replication cycles, so that the older a person is, the greater the chance of DNA damage [15].
In the results of this study, it was found that 45 NSCLC patients had a history of being active smokers (60%). This is in line with the findings of Jose et al. [16] in 761 NSCLC patients, where 55.3% of patients were found to have a history of smoking or were still smoking at the time the research was conducted. In several previous studies, it was also found that most NSCLC patients had a history of smoking. Furrukh et al. [17] reported that 47 cases (91%) of lung cancer had a history of smoking, and the risk of lung cancer increased with the duration and intensity of smoking. Cigarette smoke contains more than 60 chemicals that have been identified as carcinogens. The most potent carcinogens are polycyclic aromatic hydrocarbons, such as benzo[a]pyrene and nitrosamines specific to tobacco which are derived from nicotine (Nicotine-derived Nitrosamine Ketone; NNK). Carcinogens produced during smoking or produced in its intermediate metabolites can activate cell proliferation and survival signals, resulting in preneoplastic changes in bronchial epithelial cells and inducing lung cancer [18].
The bronchial wash VEGF levels in NSCLC patients were significantly higher compared to the control group, as well as the serum VEGF levels in NSCLC patients, which were higher and statistically significant compared to control patients. This is in line with the findings of Xu et al. [19] that serum VEGF levels in NSCLC patients were higher than in controls with a significant difference. Likewise, Cao et al. [9] found that VEGF levels in bronchial lavage were significantly higher in patients with malignant lung masses compared to patients with benign masses. Similar findings were also found by Lai et al. [20], who found that the serum VEGF levels of NSCLC patients are significantly higher than the serum VEGF levels of controls. The results of this study show that there is an increase in VEGF levels in both serum and bronchial wash in NSCLC patients.
VEGF has an important role in various pathophysiological processes in NSCLC. One of the major roles of VEGF in the pathophysiology of NSCLC is related to the dependence of tumour growth on angiogenesis. In this context, VEGF specifically promotes endothelial cell proliferation and induces angiogenesis, and its biological effects include increasing vascular permeability, promoting endothelial cell mitosis, and affecting the extracellular matrix. VEGF can also induce the expression of plasminogen activator and its inhibitors, as well as tissue factor and matrix collagenase, which are conducive to blood vessel growth [20]. Abnormal tumour cell proliferation causes a hypoxic environment that is conducive to VEGF production. Furthermore, VEGF specifically acts on vascular endothelial cells to promote cell proliferation, migration, and angiogenesis. Therefore, VEGF plays an important role in the growth of blood vessels involved in tumour growth [21]. In addition, the study of Cao et al. [9] found that VEGF was present in much higher levels in bronchial lavage, indicating that in this context, VEGF is produced locally in the airway.
Another result of this study shows that there is a significant positive correlation between bronchial wash VEGF and serum VEGF levels. This shows that the higher the serum VEGF level, the higher the bronchial wash VEGF level in NSCLC patients. This is in line with the findings of Cao et al. [9], who found that VEGF levels in bronchoalveolar lavage and serum in NSCLC patients had a positive correlation. However, it was further found that VEGF levels from bronchial lavage were significantly greater than VEGF levels.
Mounting evidence shows that VEGF expression is significantly higher in patients with malignant lung masses, including NSCLC, compared to patients with benign masses, indicating the potential of VEGF as a good marker for the diagnosis of lung cancer [9]. The results of ROC curve analysis in this study show that VEGF levels in bronchial wash and serum have the potential to be used as diagnostic biomarkers for NSCLC. Although both are equally potent, the level of VEGF in serum with a cut-off value of 640.42 pg/mL shows its superiority with a higher AUC value (AUC: 0.709, sensitivity: 53.3%, specificity: 82.9%) compared to bronchial wash fluid VEGF with a cut-off value of 667.17 pg/mL (AUC: 0.653, sensitivity: 36%, specificity: 100%). This result is different from the study of Chakra et al. [22], which reported that serum VEGF was not a significant biomarker of NSCLC, although the cut-off value found was the same at around 600 pg/mL. Although the number of samples used in the study of Chakra et al. [22] was larger, we believe that differences in sociodemographic status may be a factor because the study was conducted in Europe. In addition, biomarker assessment in this study was conducted before patients received any intervention or treatment, so there is no risk of bias in the results due to treatment effects [22]. While a similar study in Asia was conducted by Lai et al. [20] and showed results that were in line with the results in this study. Lai et al. [20] reported the ability of serum VEGF in diagnosing NSCLC with an AUC value of 0.824 with a sensitivity of 75% and specificity of 93.3%. The difference in AUC, sensitivity and specificity values could be due to the smaller number of samples in this study compared to the study of Lai et al. [20]. However, the results of this study still show consistency with the results of previous studies that VEGF in serum or bronchial wash fluid can be used as a diagnostic biomarker in NSCLC patients.
The results of this study found that VEGF has a crucial role in NSCLC patients. Increased expression of VEGF in NSCLC patients, both in serum and bronchial wash, has the potential to be used as a diagnostic biomarker for NSCLC patients. Examination of serum VEGF and bronchial wash can be an option for patients suspected of NSCLC, especially at the age of more than 50 years. The results of VEGF levels in NSCLC patients can also be a consideration for the administration of anti-VEGF therapy which is currently being developed. Apart from the results in this study, we are aware that there are still several limitations to this study, including the small sample size and the existence of variables that were significantly different between the NSCLC and control groups (age and smoking status). Although in several previous studies it was reported that there was no significant correlation between VEGF expression and age [19]. We cannot deny that these two variables remain confounding factors in this study. So we recommend that further research be carried out with a larger sample size, if possible, in a multicenter hospital and adjust the characteristics between the case and control groups.
AUC: area under the curve
ELISA: Enzyme-Linked Immunosorbent Assay
NSCLC: Non-small Cell Lung Carcinoma
ROC: receiver operating characteristic
rpm: rotations per minute
SCLC: small cell lung cancer
VEGF: Vascular Endothelial Growth Factor
We would like to thank all the staff of the Department of Pulmonology and Respiratory, Faculty of Medicine, Hasanuddin University, Wahidin Sudirohusodo General Hospital, and Hasanuddin University Medical Research Unit (HUM-RC) for their cooperation during the course of this research.
NMW: Conceptualization, Investigation, Data curation, Formal analysis, Writing—original draft, Writing—review & editing. AS: Conceptualization, Investigation, Writing—review & editing, Supervision. HAP: Conceptualization, Investigation, Validation, Writing—review & editing, Supervision. HI, NL, and BN: Investigation, Writing—review & editing, Supervision. All authors read and approved the submitted version.
The authors declare that they have no conflicts of interest.
This study received ethical clearance from Hasanuddin University Faculty of Medicine Ethics Commission (No.692/UN.4.6.4.5.31/PP36/2023).
Informed consent to participate in the study was obtained from all participants.
Not applicable.
Datasets are available on request.
Not applicable.
© The Author(s) 2025.
Open Exploration maintains a neutral stance on jurisdictional claims in published institutional affiliations and maps. All opinions expressed in this article are the personal views of the author(s) and do not represent the stance of the editorial team or the publisher.
Copyright: © The Author(s) 2025. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 3352
Download: 24
Times Cited: 0
Tatiana L. Nekhaeva ... Irina A. Baldueva
Viktoria Borobova ... Sergey Kovalenko
Evgeny Imyanitov, Anna Sokolenko
