Affiliation:
1Department of Pharmacy, Debre Markos University, Debre Markos, Ethiopia
ORCID: https://orcid.org/0000-0003-0810-1191
Affiliation:
2Deprtment of Pharmacy, Komar University of Science and Technology, Sulaymaniyah, Iraq
3School of Pharmacy, Wolaita Sodo University, Woliata Sodo, Ethiopia
Email: alemayehutoma@gmail.com
ORCID: https://orcid.org/0000-0003-1511-1531
Affiliation:
3School of Pharmacy, Wolaita Sodo University, Woliata Sodo, Ethiopia
ORCID: https://orcid.org/0000-0003-1956-6744
Explor Med. 2025;6:1001328 DOI: https://doi.org/10.37349/emed.2025.1001328
Received: January 15, 2025 Accepted: May 08, 2025 Published: June 08, 2025
Academic Editor: Lindsay A. Farrer, Boston University School of Medicine, USA
Aim: This study aimed to identify the predictors of treatment outcomes among children under five years of age hospitalized with severe acute malnutrition.
Methods: A hospital-based prospective cohort study was conducted among children under five years diagnosed with severe acute malnutrition. A total of 143 children were recruited using a consecutive sampling method. Univariable and multivariable logistic regression analyses were utilized to identify predictors of treatment outcomes. Survival analyses, including life-table analysis, Kaplan-Meier survival curves, the log-rank test, and the Cox proportional hazards model, were employed to estimate survival probabilities, recovery rates over time, and predictors of time to recovery.
Results: Of the 143 enrolled children, 55.2% were male, and 58% were between 6 and 24 months of age. During a total of 1,802 child days of follow-up, the treatment outcomes were as follows: 60.8% of children recovered, 32.9% transferred out for other medical reasons, 4.2% defaulted, and 2.1% died. Key predictors of poor treatment outcomes included hypothermia [adjusted odds ratio (AOR) = 0.17; 95% confidence interval (CI): 0.03–0.94; p = 0.042], diarrhea (AOR = 0.28; CI: 0.12–0.66; p = 0.004), edema (AOR = 0.21; CI: 0.07–0.64; p = 0.006), and feeding with ready-to-use therapeutic food (RUTF) [recovery (AOR = 2.01, 95% CI: 0.92–4.96; p = 0.098)]. The median recovery time was 14 days (95% CI: 12.9–15.1).
Conclusions: The study highlighted suboptimal recovery rates and average daily weight gain among children treated for severe acute malnutrition. Diarrhea, hypothermia, and edema on admission were associated with lower nutritional recovery rates. These findings underscore the need for targeted interventions to address these factors and improve treatment outcomes in children with severe acute malnutrition.
Severe acute malnutrition (SAM) is evidenced by visible severe wasting, eventual nutritional origin edema of feet, mid upper arm circumference (MUAC) < 11.5 cm, and, most importantly, very low weight for height (WFH) [1]. Height to weight limit should be less than –3 Z scores of the median growth standards of the WHO in order to define SAM. SAM is still a major public health concern in many African and Asian countries for its effects on overall health and development priorities [2, 3]. Most SAM children are in South Asia and Sub-Saharan African countries. Insufficient use of carbohydrates, protein, vitamins, and minerals is one and the major causes of malnutrition [4].
Childhood malnutrition is defined as a set of nutritional disorders encompassing stunting, underweight, wasting, moderate acute malnutrition (MAM), SAM, and micronutrient shortages [5]. Under-nutrition is often an outcome of low dietary consumption of various minerals and nutrients or the presence of morbidity [4]. SAM affects almost twenty million children of pre-school age, majorly in Sub-Saharan Africa and South East Asia regions. Worldwide, malnutrition is a key factor in about one third of almost eight million of the reported under five mortalities [1].
Ethiopia is documented for its history of inconsistent food access and nutritional matters, harming considerable division of the population [5]. Even during the time of relatively less-drought times, children and women’s malnutrition remain high, posing a greater risk to their survival [6].
The Ethiopian Demographic and Health Survey (EDHS) of 2019 indicated the prevalence of wasting, underweight, and stunting were 7%, 21%, and 37%, respectively [7]. According to this report, a higher percentage of males (31%) than females (27%) were underweight. Similarly, the proportion of underweight children in rural areas (30%) was higher than that of urban children (17%) [5, 8]. The under five mortality rate and nutritional recovery rate in children with SAM in Ethiopia still show a big deviation from international standard limits [9].
The minimum international standards set by the SPHERE project to help manage SAM were a cure rate of at least 75%, defaulter rate of less than 15%, and death rate below 10% [10, 11]. However, in hospitals treating SAM in developing countries, the rate of case-fatalities is high (average 20–30%). In Ethiopia, the rate of death in children under five with SAM was 3.5–29%, describing a variation of 26% [11, 12]. Similarly, in different facilities of the country, the range of rates of nutritional recovery was 43.5–87.6%. This indicates that there is a significant deviation from the national treatment outcome goals and more work is to be done on this issue [13, 14]. Our null hypothesis was that recovery and deaths from SAM were in agreement with WHO SAM treatment outcome standards for hospitalized SAM patients.
The study was conducted at Wolaita Sodo University Comprehensive Specialized Hospital (WSUCSH) Medical Center, located 329 km South of Addis Ababa, Wolaita Zone, Wolaita Ethiopia. The former “Otona Hospital” and the current WSUCSH were established in 1920 E.C as small clinics by Sudan Interior Mission (SIM). The hospital delivers different medical services for outpatient, emergency, and inpatients for about 450–500 cases per day. The total service coverage of the hospital is about three million people in catchment areas.
A facility based prospective cohort study was employed to determine predictors of treatment outcomes in under five children with SAM receiving care at WSUCSH Medical Center in the time period of follow-up from mid-May to mid-August 2022.
All under five years of age children patients admitted with the diagnosis of SAM and receiving care (treatment) in the study period were included and followed.
Children whose parents or care takers not willing to participate in the study were excluded from the study.
SAM: WFH < –3 Z score or MUAC < 11.5 cm for 6–59 months of age children.
SAM: weight for length (WFL) < –3 Z score or bilateral pitting edema for less than 6 months of age.
Admission criteria: Infants and children who are less than 59 months of age and have a MUAC < 11.5 cm or a WFH/WFL < –3 Z scores of the WHO growth standards or have bilateral edema.
Cured/recovered: Patient who has reached the discharge criteria.
Death: Patient who has died while he or she was in the program at the facility or in transit to another component of the program.
Defaulter: A child for whom two consecutive weighings (i.e., for 2 days) were absent during inpatient therapeutic feeding program.
Non-responder: Patient who has not reached the discharge criteria after 40 days treatment program.
Censored: If a child’s clinical information is recorded as death, defaulter, transfer out or unknown status, then this was operationally defined as censored.
Discharge criteria: WFH/WFL is ≥ –2 Z score and they have had no edema for at least 2 weeks, or MUAC is ≥ 125 mm and they have had no edema for at least 2 weeks.
Based on the number of patient flow in this hospital’s nutritional rehabilitation unit; we intend to study all of the admitted under five SAM children within the study period. Therefore; the implemented sampling technique was a total enumerative sampling method and so, all eligible children admitted in the study period were studied consecutively. In the study period (from mid-May to mid-August 2022) the total number of admitted eligible SAM children was 143 and all of them were enrolled and followed.
The data collection tool was a structured format adapted from reviewing different literature and previous similar studies done on this study title [15]. The prepared format contains five main different categories which include socio-demographic characteristics, history and examination, vital sign and laboratory tests, nutritional diagnosis and other medical diagnoses, and Final treatment outcome.
Before the actual data collection, a pretest was done to ensure the appropriateness of the data collection instrument and necessary modifications were made. Data was collected by three assigned and pre-trained health care professionals (HCP) i.e., by two nurses working at pediatric ward SAM treatment unit and one pharmacist as a supervisor. Data was collected in three main techniques; through direct patient (parent) interviews including socio-demographic and other patient related factors, by assessing the patient’s medical chart, and by direct measurement of patient conditions. We followed pre-designed conceptual framework to develop tools for data collection (Figure 1). The supervisor and the principal investigator supervised the data collection process daily and assured the precision of data collection.
Before analysis started, the completeness and consistency of the collected data were checked. Then, cleaning, editing, and coding of the data were also performed. Data was entered into SPSS version 25.0 for data analysis. The life-table analysis, Kaplan-Meier survival analysis, and log-rank test were used to estimate proportion surviving within each interval, to determine rate of nutritional recovery over time, and to compare time to recovery respectively. Bivariate and then multivariate logistic regression analyses were also used to identify predictors of treatment outcomes. Statistical significance was determined by setting p-values < 0.05 and 95% confidence intervals (CIs).
Prior to the actual data collection process, hands on training was delivered for both data collectors and the mentors concerning the data gathering tool and data gathering process for one day and before the beginning of data gathering, the consistency in the recording of variables in the follow-up forms was checked by taking few patients and amendments were done on the data collection tool after cheek up. The supervisor and principal investigator were assigned for a strict follow-up and supervision throughout the entire data collection period.
Before conducting the study, the study protocol was approved by the Research Ethics and Approval Committee of Wolaita Sodo University College of Health Sciences and Medicine with a project No. CHSM/ERC/06/14. Official letters of co-operation were written to WSUCSH to facilitate the study with letter No.4/467/20/1. Both written and verbal consent were obtained from the parents and study subjects confidentiality was assured as the information they gave will not be used for any purpose other than the study of treatment outcome. The privacy of the participants was maintained as data were anonymized or maintained with confidentiality. We confirm that the study complies with the Declaration of Helsinki.
Out of 157 children admitted for SAM treatment to the hospital during the study period (from mid-May to mid-August 2022), 14 were excluded due to their age of greater than 59 months and the rest children met the inclusion criteria and enrolled. Of the total of 143 children, 79 (55.2%) were males, and most 83 (58%) of them were aged between 6 to 24 months; while 15 (10.5%) of children were younger than six months of age. The mean and median age of the whole cohort was 21 (± 16) and 14 months (6–24) respectively. More than two thirds of the children were from rural areas (n = 100, 69.9%). The majority, 118 (82.5%) of the children were on breast feeding during admission while only 67 (46.9%) of the total children was on exclusive breast feed for the first six months of their age. The mean age for those children’s mothers was 35 (± 6) and the average number of children for the families was 3.4 (± 2) concerning the educational status of mothers; 54 (37.8%) of them attended primary education.
The mean weight of the children at admission was 7.46 (± 2.8) kg while at the time of discharge was 7.65 (± 2.5) kg. The majority of above five months of age children (60.8%) had MUAC below 11.5 cm and about 79.7% of the whole cohort had WFH/WFL less than 70% [–3 standard deviation (SD)] at the time of admission (Table 1).
Anthropometric measurements of SAM children; WSUCSH, 2022 (n = 143)
| Variable | Frequency | Percentage | |
|---|---|---|---|
| MUAC on admission where is the place for 11.5 | < 11.5 cm | 87 | 60.8 |
| > 11.5 cm | 56 | 39.2 | |
| WFH (SD) = –3 | < –3 | 114 | 79.7 |
| > –3 | 29 | 20.3 | |
| SAM type | Marasmus | 91 | 63.6 |
| Kwashiorkor | 36 | 25.2 | |
| Marasmic-kwash | 16 | 11.2 | |
MUAC: mid upper arm circumference; SAM: severe acute malnutrition; SD: standard deviation; WFH: weight for height; WSUCSH: Wolaita Sodo University Comprehensive Specialized Hospital
Concerning co-morbidities on admission; almost all (94%) of the admitted children had at least one medical condition or complication with SAM and the most common co-morbidities accompanied with SAM at admission were: anemia (74.1%), diarrhea (47.6%), and edema (39.9%). About 60.1% of the cohort was diagnosed with non-edematous SAM. Tuberculosis co-infection 2.8%, pneumonia 30.1%, malaria 2.1%, and vomiting 28% were the other medical problems identified on admission.
Almost all of the admitted children, 131 (91.6%) had been given F-75 formula milk as a main nutritional support. In addition, 49.0% and 10.5% of the children received ready-to-use therapeutic food (RUTF) and F-100 formula milk during their admission stay respectively. Concerning the routine medication use; except in one case, all 142 children were provided the routine anti-biotics which were mainly ampicillin and gentamycin among others. Also, from 68 SAM children with diarrhea; 30% of them were given rehydration solution for malnutrition (ReSoMal) as a fluid and electrolyte replacement.
After 1,802 child days of follow-up; 87 (60.8%) recovered or cured from malnutrition state, 47 (32.9%) transferred out for other medical reasons or outpatient treatment program, 6 (4.2%) defaulted and 3 (2.1%) cases were died during the data collection period. The overall incidence rate of recovery was 4.8 cases per 100 child days of follow-up. Based on the treatment outcome: 60.8% of the children were recognized as ‘recovered’ while the rest (39.2%) were called ‘censored’ for the purpose logistic regression analysis model. The overall average weight gain for the children who recovered from wasting was 7.6 g/kg/day. The mean (± SD) length of hospitalization for the cohort was determined and it was 12.6 (± 5.8) days and specifically for recovered children was 13.3 (± 6.7) days.
In the first week of admission, only 8 (9%) of the children recovered while 49 (56.3%) recovered within the second week of admission. The total percentage of recovery within 3 weeks of admission was estimated to be 95.4%. The overall mean recovery time was also estimated and it was 15 days (95% CI, 14.3–17.2).
The overall median recovery time of the children was 14 days (95% CI; 12.9–15.1). The Kaplan-Meier survival analysis indicated that there was a statistically significant difference in the median time to recovery on the variables of sex, residence, and admission MUAC level. There was a difference in median time to recovery with (log-rank = 5.615, p = 0.018) between males (13 days, 95% CI; 11.71–14.28) and females (16 days, 95% CI; 14.53–17.46). Also, those SAM children from urban areas recovered faster than those from rural areas (log-rank = 9.349, p = 0.002) (Table 2 and Figure 2).
Kaplan-Meier survival estimates for the median recovery time from SAM at the therapeutic feeding unit of WSUCSH, Southern Ethiopia, 2022 (n = 143)
| Characteristic | Category | Median recovery time (days) | p-value | ||
|---|---|---|---|---|---|
| Estimate | 95% CI | Log-rank; χ2-value | |||
| Sex | Male | 13 days | 11.71–14.28 | 5.615 | 0.018* |
| Female | 16 days | 14.53–17.46 | - | - | |
| Residence | Urban | 13 days | 10.74–15.25 | 9.349 | 0.002* |
| Rural | 15 days | 12.71–17.29 | - | - | |
| Exclusive breast feed | Yes | 13 days | 11.64–14.35 | 3.016 | 0.082 |
| No | 15 days | 13.79–16.20 | - | - | |
| Pneumonia co-infection | Yes | 16 days | 12.10–19.89 | 3.719 | 0.054 |
| No | 14 days | 13.23–14.76 | - | - | |
| MUAC level on admission | < 11.5 cm | 15 days | 13.70–16.29 | 3.897 | 0.048* |
| ≥ 11.5 cm | 14 days | 13.11–14.88 | - | - | |
| WFH/WFL level on admission | < –3 (SD) | 15 days | 13.83–16.16 | 3.087 | 0.079 |
| ≥ –3 (SD) | 13 days | 10.67–15.32 | - | - | |
*: significant at p-value < 0.05; -: no data. CI: confidence interval; MUAC: mid upper arm circumference; SAM: severe acute malnutrition; SD: standard deviation; WSUCSH: Wolaita Sodo University Comprehensive Specialized Hospital; WFH: weight for height; WFL: weight for length
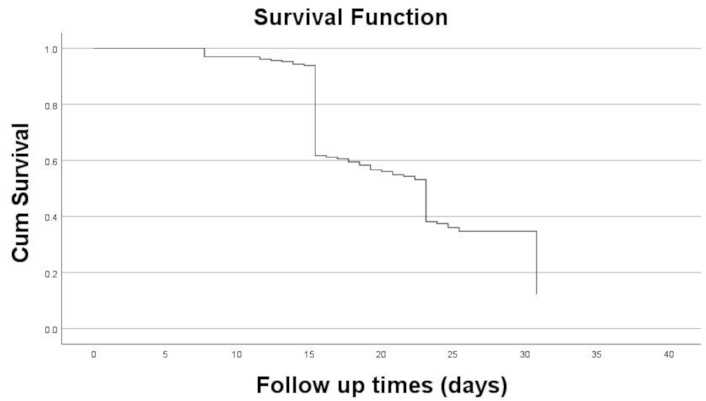
Life-table showing the overall survival function of the cohort; WSUCSH, 2022 (n = 143). WSUCSH: Wolaita Sodo University Comprehensive Specialized Hospital
A Cox proportional hazard model was tested to see the effect of predictor variables on the survival time and so; twenty-two independent variables were analyzed in the bivariate Cox proportional hazard analysis along with the dependent variable. However, only one variable (residence) was found to be independent predictor of survival time. i.e., SAM children from rural areas were with 0.266 times poor prognosis of survival as compared to SAM children from urban [adjusted hazard ratio (AHR) = 0.26, 95% CI: 0.13–0.55, p < 0.001] (Table 2 and Figure 2).
Independent variables underwent both bivariate and multivariable logistic regression; three of them were found to have significant association with the outcome variable. Also, presence of edema on admission and hypothermia on admission did not show significant association on bivariable analysis but these predictors show significant association with the outcome variable on the final logit model. Children who were hypothermic on admission were 83.1% less likely to recover as compared to those without hypothermia [adjusted odds ratio (AOR = 0.17, 95% CI: 0.03–0.94; p = 0.042)]. Likewise, children with diarrhea on admission were 72% less likely to recover from SAM as compared to those without diarrhea (AOR = 0.28, 95% CI: 0.12–0.66; p = 0.004). Also, children with edematous SAM were found to be less likely to recover from SAM than non-edematous ones (AOR = 0.21, 95% CI 0.07–0.64; p = 0.006). In addition, children who provided RUTF had more chance of recovery (AOR = 2.01, 95% CI: 0.92–4.96; p = 0.098) (Table 3). Other predictor variables like: exclusive breast feed for the first six months of age, time length of breast feed, and presence of cough on admission showed associations with the outcome variable but; that was not statistically significant.
List of predictor variables from bivariate and multivariate logistic analysis with each respective association for the treatment outcome variable, WSUCSH, 2022 (n = 143)
| Independent variables | Treatment outcome | COR (95% CI) | AOR (95% CI) | p-value | |
|---|---|---|---|---|---|
| Recovered | Censored | ||||
| Exclusive breast feed, % yes | 44 (65.5%) | 23 (34.3%) | 1.45 (0.75–2.89) | 1.26 (0.54–2.95) | 0.585 |
| Odema, % yes | 32 (56.2%) | 25 (43.8%) | 0.72 (0.36 –1.42) | 0.21 (0.07–0.64) | 0.006* |
| Diarrhea, % yes | 34 (50%) | 34 (50%) | 0.42 (0.21–0.82) | 0.28 (0.12–0.66) | 0.004* |
| Hypothermia, % yes | 8 (44.4%) | 10 (55.5%) | 0.46 (0.17–1.26) | 0.17 (0.03–0.94) | 0.042* |
| MUAC level, < 11.5 cm | 45 (51.7%) | 42 (48.3%) | 0.54 (0.25–1.15) | 0.34 (0.10–1.13) | 0.078 |
| WFH level, < –3 (SD) | 66 (57.9%) | 48 (42.1%) | 0.52 (0.21–1.28) | 0.35 (0.10–1.21) | 0.098 |
| RUTF given, % yes | 36 (51.4%) | 34 (48.6%) | 2.13 (0.92–4.96) | 2.01 (0.92–4.96) | 0.098 |
| Time length on breast feed | 87 (60.8%) | 56 (39.2%) | 1.04 (0.99–1.09) | 1.03 (0.96–1.09) | 0.377 |
*: significant at p-value < 0.05. AOR: adjusted odds ratio; CI: confidence interval; COR: crude odds ratio; MUAC: mid upper arm circumference; RUTF: ready-to-use therapeutic food; SD: standard deviation; WFH: weight for height; WSUCSH: Wolaita Sodo University Comprehensive Specialized Hospital
In our study, among 143 children with SAM who enrolled in the cohort; (60.8%) recovered, (32.9%) transferred out for other medical reasons or outpatient treatment program, (4.2%) defaulted and (2.1%) cases died during the follow-up period. So, based on the above standards: as we compared the nutritional recovery rate from our study (60.8%), it was found to be below the line of the project standard limit. Likewise, there are studies with lower recovery rates than the project standard, like: the study done at Northern Uganda [13], Jima University [15], and Debre Berhan Hospital [16] showed 67%, 25.6%, and 55.9% recovery rate respectively. But, contrary to our study result, studies from Yirgalem Hospital [17, 18], Woldia Hospital [1, 19], and Paulos Hospital [20, 21] showed greater recovery rates of 78%, 85%, and 79% respectively. This deviation may be due to the higher nutritional transfer rate in our study setting which was (32.9%) as it could affect the number of nutritional recoveries.
The defaulter rate (4.2%) and case fatality rate (2.1%) in this study were found to be within the standard limits of the project. And this was an appreciable result in this study specially to keep down the death rate in this hospital alongside improving the nutritional recovery rate. Similarly, there were studies with case fatality rates within the desired limit of the standard [15, 17, 22]. But, differing from our study; studies from Uganda and Yirgalem showed the higher case fatality rates [13, 18]. Our success may be due to lower prevalence of co-morbidities like: tuberculosis and HIV in our study subjects as compared to those studies with higher case fatality rates. The overall incidence rate of recovery in this study was; 4.8 cases per 100 child days of observation. This finding was comparable with findings from Adem et al. [14].
In this study, the overall average weight gain for the children who recovered from wasting was 7.6 g/kg/day which was also below the national standard (≥ 8g/kg/day). This nonachievement may be due to inadequate or incomplete amount provision of the daily prescribed therapeutic feeding to the SAM children and or due to untreated infection.
From the time to event analysis of this study: In the first week of admission, only 8 (9%) of the children were recovered while 49 (56.3%) were recovered within two weeks of admission. The total percentage of recovery within 3 weeks of admission was estimated to be 95.4%. This result was comparable to different studies those with the majority of the admitted children recovered within the first three weeks of admission [18, 23].
From Kaplan-Meier survival analysis of this study: the overall follow-up time of the whole cohort was 1,802 child days. The median recovery time of the recovered children was 14 days (95% CI; 12.9–15.1) and this result was in agreement with the international recommendation which establishes it to be less than four weeks for inpatient management of SAM [14]. In addition, this result was in line with the study result from North Shoa which showed that; the median recovery time of 15 days (95% CI: 14.09–15.908). But, comparing to other studies: studies done in India [24], Malawi [25], and Ethiopia Oromia Regional State, Jimma Medical Center [15] reported 15.5 days, 49 days, and 26 days respectively which all were with longer median recovery time than ours. This success may be due to the fact that; there was lower co-infection prevalence in our study population as compared to those studies. The possible explanation for this is that: presence of co-infections with SAM could negatively affect the prognosis of nutritional recovery.
In addition, the Kaplan-Meier survival analysis indicated that: there was a statistically significant difference in the median time to nutritional recovery for the variables of sex, residence, and admission MUAC level. Accordingly: male children were found to achieve faster nutritional recovery than female children (log-rank = 5.615, p = 0.018) with the median recovery time of 13 and 16 days for males and females respectively. Also, those SAM children from urban areas recovered faster than those from rural areas (log-rank = 9.349, p = 0.002). This variation may be due to the differences in appropriate child feeding practices especially on the prescribed daily energy and protein intakes. Furthermore: those SAM children with admission MUAC level below 11.5 cm achieved slower median nutritional recovery time by one day as compared to SAM children with MUAC level above 11.5 cm (log-rank = 3.897, p = 0.048). This difference could be scientifically explained as: children with lower MUAC value of 11.5 cm could have poor prognosis of recovery from SAM as this value indicates the severity of the malnutrition state [15, 19].
Notably, although the presence of edema and hypothermia at the time of admission did not exhibit significant associations in the bivariable analysis, both emerged as significant predictors within the final adjusted logistic regression model. Specifically, pediatric patients presenting with hypothermia upon admission exhibited an 83.1% reduced likelihood of recovery relative to their normothermic counterparts; (AOR = 0.17, 95% CI: 0.03–0.94; p = 0.042). This was comparable to the study from Uganda and western Ethiopia [13, 17]. Likewise, children with diarrhea on admission were 72% less likely to recover from SAM as compared to those without diarrhea (AOR = 0.28, 95% CI: 0.12–0.66; p = 0.004). This result was comparable to the study result from Zambia [25]. Also, children with edematous SAM were found to be less likely to recover from SAM than non-edematous ones; (AOR = 0.21, 95% CI 0.07–0.64; p = 0.006). This finding was comparable with the study results from Woldia [1], Bahir Dar [26], and Debre Berhan [23].
In addition, children who provided RUTF had 36% more chance of recovery (AOR = 2.01, 95% CI: 0.92–4.96; p = 0.098). Other predictor variables like: exclusive breast feed for the first six months of age, time length of breast feed, and presence of cough on admission showed associations with the outcome variable but; that was not statistically significant.
Limitation of the study could be due to use of the total enumerative sampling technique, the representativeness of the sample may be limited and also, even if our study design requires large sample size by its nature, we were limited to small sample size according to our resource limitations, this may impact our study finding generalizability power. Further multicenter and large sample size-based studies should be conducted for detailed investigation of predictors and management strategies to solve severe malnutrition problems in developing countries. Management strategies should address recent advances in role of AI in nutrition management or implementing Internet of Things (IoT) systems for remote monitoring and other technologies [27, 28].
The study highlighted suboptimal recovery rates and average daily weight gain among children treated for SAM. Diarrhea, hypothermia, and edema on admission were associated with lower nutritional recovery rates. These findings underscore the need for targeted interventions to address these factors and improve treatment outcomes in children with SAM.
AOR: adjusted odds ratio
CIs: confidence intervals
MUAC: mid upper arm circumference
RUTF: ready-to-use therapeutic food
SAM: severe acute malnutrition
SD: standard deviation
WFH: weight for height
WFL: weight for length
WSUCSH: Wolaita Sodo University Comprehensive Specialized Hospital
We are grateful to the Wolaita Sodo University Comprehensive Specialized Hospital Antiretroviral Therapy Clinic staff for providing the data.
DM: Conceptualization, Funding acquisition, Data curation, Formal analysis, Investigation, Writing—original draft, Writing—review & editing. AT and TB: Conceptualization, Writing—review & editing. All authors read and approved the submitted version.
The authors declare that there are no conflicts of interest.
Ethical approval number CHSM/ERC/06/14 for this study was obtained from Institutional Ethical Review Committee of Wolaita Sodo University College of Medicine and Health Sciences. The study adhered to the Declaration of Helsinki.
The informed consent to participate in the study was obtained from the parents of all participants.
Not applicable.
The data that support the findings of this study are available from the corresponding author upon reasonable request.
This study was funded by Wolaita Sodo University Office of Vice President for Research and Technology Transfer Grant Number [6114/2021]. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
© The Author(s) 2025.
Open Exploration maintains a neutral stance on jurisdictional claims in published institutional affiliations and maps. All opinions expressed in this article are the personal views of the author(s) and do not represent the stance of the editorial team or the publisher.
Copyright: © The Author(s) 2025. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 2411
Download: 34
Times Cited: 0
