Affiliation:
Department of Psychology, Washington State University, Pullman, WA 99164-4820, USA
ORCID: https://orcid.org/0000-0002-0160-7838
Affiliation:
Department of Psychology, Washington State University, Pullman, WA 99164-4820, USA
Email: carrie.cuttler@wsu.edu
ORCID: https://orcid.org/0000-0002-5890-2985
Explor Med. 2023;4:709–719 DOI: https://doi.org/10.37349/emed.2023.00171
Received: May 31, 2023 Accepted: July 25, 2023 Published: October 25, 2023
Academic Editor: Lindsay A. Farrer, Boston University School of Medicine, USA
The article belongs to the special issue Beyond Weed: Clinical Applications of Cannabis and Cannabinoids
Aim: Cannabis use for sleep-related problems is on the rise; however, little is known about the cannabis products people are using for sleep or the perceived effects of cannabis in comparison to more conventional sleep aids. Therefore, the aim of this study was to examine the products cannabis users prefer to use for sleep as well as their experiences with cannabis relative to more conventional sleep aids.
Methods: De-identified archival data from a Strainprint® survey of 1,216 individuals who use cannabis for sleep were analyzed.
Results: Participants predominantly reported smoking joints or vaping flower as their methods of administration, and seeking tetrahydrocannabinol (THC), cannabidiol (CBD), and the terpene myrcene in the cannabis they use for sleep. Only a small minority reported using cannabis in conjunction with conventional sleep aids. Comparisons of the self-reported effects of cannabis to conventional sleep aids revealed that participants reported feeling more refreshed, focused, better able to function, fewer headaches, and less nausea the morning after using cannabis for sleep than after using more conventional sleep aids or no sleep aids. However, they indicated they were more sleepy, anxious, and irritable in the mornings following the use of cannabis relative to other sleep aids. Participants were more likely to report red eyes and thirst and less likely to report nausea, anxiety, paranoia, and racing heart as side effects of cannabis relative to other sleep aids.
Conclusions: Knowledge gained from this survey will provide health professionals with a better understanding of why people are using cannabis for sleep and may help guide future more controlled research.
Insufficient sleep is a pervasive problem in modern society and is officially recognized as a public health epidemic by the Centers for Disease Control and Prevention [1]. Approximately 35% of adults in the United States (U.S.) report sleeping less than the recommended 7 h in a 24-hour period [2], and up to 40% report symptoms of insomnia [3]. The prevalence of insomnia and poor sleep quality in the U.S. is increasing and has led to a surge in prescription sleep aid (PSA) use [4]. The most used PSAs include various benzodiazepines and nonbenzodiazepines (e.g., Z-drugs) [5, 6]. Additionally, numerous prescriptions and over-the-counter (OTC) medications are used off-label for treating sleep problems, including herbal teas, antidepressants, antipsychotics, antihistamines, and melatonin [6, 7]. However, some of these drugs have a high potential for addiction and many are associated with undesirable side effects such as drowsiness, decreased alertness and concentration, memory impairment, and negative affect [5–7]. Moreover, prescription sedative-hypnotic use is associated with respiratory depression, cancer, infections, and injuries [8].
Emerging evidence indicates that many adults are turning to cannabis as an alternative to more conventional sleep aids and that they perceive cannabis to be an effective sleep aid. Trends towards the legalization of cannabis in North America have been associated with a decline in OTC sleep aid sales, with conventional sleep aid market shares declining 236% once cannabis dispensaries arrived [9]. Further, a survey of U.S. adults reporting recent use of sleep aids revealed that cannabis was the most reported drug used for sleep, with approximately 18% reporting use of cannabis to promote sleep, 11% reporting use of benzodiazepines, 11% reporting use of tricyclic antidepressants, and 4% reporting use of zolpidem for sleep [10]. Not surprisingly, use of cannabis for sleep appears to be even more prevalent among cannabis users, with 74% of recreational users [11] and from 45% [12] to 80% [13] of medical users reporting the use of cannabis for sleep. Moreover, the majority of recreational (> 80%) and medical (65%) cannabis users report reducing or stopping their use of more conventional sleep aids after initiating cannabis use [11, 14]. Collectively, these results indicate that a growing number of people are turning to cannabis as a substitute for more conventional sleep aids, but few studies have examined such practices, and as such it is not clear whether individuals perceive differences in the beneficial effects of cannabis versus more conventional sleep aids, or how common it is for people to combine cannabis with more conventional sleep aids.
Despite the high prevalence of cannabis use for sleep, previous reviews on the efficacy of cannabis as a sleep aid have produced mixed results [15–17] with some indicating that findings may depend on the cannabinoid under investigation. For instance, Babson and colleagues [15] concluded that tetrahydrocannabinol (THC) may decrease sleep latency but could impair sleep quality in the long term, while cannabidiol (CBD) may reduce excessive daytime sleepiness. A more recent study found that higher concentrations of CBD were associated with better self-reported sleep outcomes, particularly for those aged 30+ [18]. Similarly, a naturalistic examination of insomnia symptom ratings from before to after acute cannabis use indicated that the use of higher concentrations of CBD (but not THC) was associated with greater perceived insomnia relief [19]. Additionally, the results of this study suggested that the use of pipes and vaporizers for administration may be associated with greater insomnia symptom relief relative to the use of joints [19]. To our knowledge, this is the only previous study to examine which methods of cannabis administration are perceived to be beneficial for sleep. Clearly, additional research on the perceived efficacy of different cannabinoids and methods of administration of cannabis for sleep is needed.
Finally, it is unclear whether people report different side effects from cannabis versus more conventional sleep aids. Previous survey studies have generally revealed that sleep-related cannabis side effects are rarely reported [12, 13]. However, in two sleep studies where participants were administered 15 mg of THC alone or in combination with 15 mg of CBD, participants reported an increase in sleepiness the next morning as well as changes in mood [20, 21]. However, these side effects may be less severe or impairing than the side effects they experience with other sleep aids, and therefore, contribute to the perception that cannabis is superior to more conventional sleep aids. To our knowledge, no previous research has directly compared the reported side effects of cannabis versus PSAs and OTC sleep aids.
The present study was guided by four primary objectives: i) to explore the aspects of sleep (e.g., falling asleep, staying asleep, achieving a deeper sleep) that medical cannabis users report using cannabis to improve, ii) to explore the types of cannabis, the cannabis constituents (e.g., THC, CBD, terpenes), and the methods of administration that medical cannabis patients most commonly report using for sleep, iii) to examine how often cannabis users report using cannabis alone or in combination with OTC sleep aids and/or PSAs, and iv) to compare perceived beneficial effects and adverse side effects of cannabis versus OTC sleep aids and PSAs.
De-identified data were obtained from Strainprint®, which houses a medical cannabis technology platform in Canada. Strainprint® advertised their study via email to individuals who use their app and compensated respondents with 100 bonus Strainpoints. The Washington State University Office of Research Assurances determined that analysis of this archival survey data was exempt from the need for review by the Institutional Review Board (IRB). Strainprint® obtained informed consent from all participants and authorized our use of the data for research purposes. The inclusion criteria were being a user of the Strainprint® app, being 18 years of age or over, self-reported sleep issues, and use of cannabis to help with sleep.
Interested candidates were directed to a survey hosted by Strainprint® that was designed to assess demographic characteristics (age and gender), sleep issues, use of OTC sleep medications and PSAs (current and/or past), types of cannabis products and methods of administration used for sleep, preferred cannabis constituents for sleep, aspects of sleep that cannabis is perceived to help with, how often cannabis is used in combination with OTC and/or PSAs, as well as beneficial and adverse effects experienced when using cannabis, OTC, and PSAs.
A total of 1,255 individuals initiated the survey, however, 39 of them reported that they do not use cannabis to help with sleep. After excluding those individuals, the final sample comprised 1,216 participants. The sample was predominately female (55.9% female, 33.4% male, 1.6% other, 0.7% prefer not to say, 8.4% missing), and ranged in age from 18 to 77 [mean (M) = 42.52, standard deviation (SD) = 12.66].
Further characteristics of the sample including the types of sleep issues they reported suffering from (more than one could be endorsed), reported medical issues, the length of time they have experienced sleep issues, the length of time they have used cannabis for sleep, and the frequency they use cannabis as a sleep aid are shown in Table 1. As shown, over half of the sample reported difficulty falling asleep (82.2%), feeling tired the next day (68.1%), waking during the night for no reason (67.1%), difficulty going back to sleep (61.6%), and difficulty functioning the next day due to poor sleep (53.9%). Further, the majority (64.9%) of the sample reported that they have been suffering from these sleep issues for more than five years and nearly 70% of respondents reported using cannabis to help with sleep for at least one year. Also as shown in Table 1, most respondents (68.0%) reported they use cannabis as a sleep aid every night.
Sample cannabis use patterns for sleep
| Sleep and medical issues | % | Durations and frequency of use | % |
|---|---|---|---|
| Sleep issues (N = 1,216) | Length of sleep issue (N = 1,201) | ||
| Difficulty falling asleep | 82.2% | Less than 3 years | 19.9% |
| Feeling tired the next day | 68.1% | 3–5 years | 15.1% |
| Waking during the night for no reason | 67.1% | 5 years or more | 64.9% |
| Difficulty going back to sleep | 61.6% | Length of cannabis use for sleep (N = 1,200) | |
| Difficulty functioning next day from poor sleep | 53.9% | Less than 1 year | 30.2% |
| Waking too early | 39.6% | 1–3 years | 38.0% |
| Other sleep issues that make me feel tired | 24.8% | 3–5 years | 13.6% |
| Generally sleep well except the occasional night | 4.0% | More than 5 years | 18.3% |
| Waking up during the night from noise or light | 0.0% | Frequency cannabis used for sleep (N = 1,199) | |
| Medical issues (N = 1,216) | Every night | 68.0% | |
| Heartburn/stomach issues | 79.4% | A few times a week | 23.9% |
| Anxiety | 61.8% | Once a week | 3.2% |
| Chronic pain | 48.5% | A few times a month | 3.7% |
| Depression | 48.3% | Once a month | 0.3% |
| Post-traumatic stress disorder | 28.6% | Less than once a month | 0.9% |
| Sleep apnea | 15.5% | ||
| Asthma | 10.0% | ||
| Narcolepsy | 1.1% | ||
| Other | 84.5% | ||
| None | 8.0% | ||
The data were analyzed by computing the percentage of participants who endorsed each response option on the survey. A series of chi-square analyses were conducted to compare the percentages of respondents who endorsed experiencing a variety of outcomes the morning after they use cannabis, PSAs, OTCs, or no sleep aids as well as the percentages of respondents who endorsed experiencing different side effects of cannabis, PSAs, and OTCs.
Participants were asked to report how cannabis helps with their sleep and were given the following response options (they could endorse as many as applied): relaxes my body, relaxes my mind, uninterrupted sleep, deeper sleep, and longer sleep. The vast majority reported that cannabis helps to relax their mind (83.0%) and body (81.0%). Further, 56.2% reported it helps them get a deeper sleep, 41.6% reported it helps them get a longer sleep, and 36.3% reported it provides them with uninterrupted sleep.
Participants were asked what formats (i.e., methods of administration) of cannabis products they use to help with sleep, what kinds of cannabis products help them sleep better, and whether they consider specific cannabinoids or terpenes when they are choosing a product for their sleep issue. The 624 participants (51.3% of the sample) who said yes to the latter question were asked to indicate which specific cannabinoids and terpenes they consider. Multiple response options could be endorsed for the questions pertaining to the method of administration and the cannabinoids/terpenes they consider. As further detailed in Table 2, the majority of the sample (60.0%) reported a preference for high-THC products for sleep. Consistent with this, 78.8% reported seeking THC in the cannabis they use for sleep, 47.1% reported seeking CBD, and 49.0% reported seeking the terpene myrcene in the cannabis they use for sleep. Participants predominantly reported smoking cannabis in joint form (46.1%), vaping flower (42.6%), or using oils (42.5%).
Respondents’ preferences for types and forms of cannabis used for sleep
| Types and forms of products | % | Cannabis constituents | % |
|---|---|---|---|
| Types of cannabis products (N = 1,186) | Cannabinoids used for sleep (N = 624) | ||
| High THC | 60.0% | THC | 78.8% |
| Balanced THC:CBD | 21.7% | CBD | 47.1% |
| Not sure | 6.4% | Cannabinol (CBN) | 18.1% |
| High CBD | 5.3% | Terpenes used for sleep (N = 624) | |
| Doesn’t matter | 4.2% | Myrcene | 49.0% |
| Form of cannabis product (N = 1,216) | Linalool | 26.9% | |
| Joints | 46.1% | Limonene | 24.7% |
| Oil | 42.5% | Beta caryophyllene | 19.1% |
| Vape flower | 42.6% | Terpinolene | 13.5% |
| Edibles | 34.9% | Humulene | 7.1% |
| Vape pen | 33.9% | Nerolidol | 4.0% |
| Capsules | 14.6% | ||
Participants were asked whether they have used OTC sleep medications or PSAs in the past, whether they currently use OTC sleep medications or PSAs, and whether they currently use cannabis in conjunction with OTC sleep medications or with PSAs. Most (81.8%) reported that they do not currently use OTC medications or PSAs; however, 53.2% reported using PSAs in the past, and 60.6% reported using OTC sleep medications in the past. Only 4.4% reported using cannabis in combination with OTC medications and 7.9% reported using PSAs in combination with cannabis.
Those participants who endorsed using all three types of sleep aids were asked to think about how they feel when they wake up in the morning and then to indicate which sleep aid(s) (cannabis, OTC medications, PSAs, and no sleep aid) provide a series of positive and negative outcomes in the morning (e.g., more refreshed, more focused, sleepy). For each, participants could endorse multiple sleep aids as producing each outcome. As shown in Table 3, chi-square analyses indicated that of the 526 people who have used all three types of sleep aids, significantly more reported that they feel more refreshed, more focused, and better able to function the morning after using cannabis relative to OTC sleep aids, PSAs, or no sleep aids. Participants also reported fewer headaches and less nausea the morning after using cannabis relative to other sleep aids or no sleep aids. However, significantly more participants endorsed feeling more sleepy, more anxious, and more irritable the morning after using cannabis relative to other sleep aids or no sleep aids.
Reported morning outcomes (N = 526)
| Outcomes | Cannabis n (%) | PSA n (%) | OTC n (%) | No aid n (%) | Chi-square |
|---|---|---|---|---|---|
| More refreshed | 466 (88.6%a) | 9 (1.7%b) | 4 (0.8%b) | 11 (2.1%b) | χ2 = 1,284.48, P < 0.001 |
| More focused | 421 (80.0%a) | 8 (1.5%b) | 2 (0.4%b) | 28 (5.3%c) | χ2 = 1,093.13, P < 0.001 |
| Better able to function | 394 (74.9%a) | 8 (1.5%b) | 1 (0.2%b) | 23 (4.4%c) | χ2 = 1,037.19, P < 0.001 |
| Fewer headaches | 402 (76.4%a) | 6 (1.1%b) | 3 (0.6%b) | 12 (2.3%b) | χ2 = 1,106.96, P < 0.001 |
| Less nauseous | 384 (73.0%a) | 3 (0.6%b) | 2 (0.4%b) | 7 (1.3%b) | χ2 = 1,094.08, P < 0.001 |
| Sleepy | 118 (22.4%a) | 51 (9.7%b) | 20 (3.8%c) | 27 (5.1%c) | χ2 = 110.93, P < 0.001 |
| More anxious | 128 (24.3%a) | 36 (6.8%b) | 10 (1.9%c) | 31 (5.9%b) | χ2 = 160.68, P < 0.001 |
| More irritable | 119 (22.6%a) | 32 (6.1%b) | 17 (3.2%c) | 37 (7.0%b) | χ2 = 123.64, P < 0.001 |
Percentages with no superscripts or the same superscripts do not differ significantly from those in the same row while those with different superscripts are significantly different from those in the same row at P < 0.05. Missing data and not applicable responses were as follows: more refreshed = 36, more focused = 67, better able to function = 100, less headaches = 103, less nauseous = 130, sleepy = 310, more anxious = 321, more irritable = 32
Participants who endorsed using all three types of sleep aids (cannabis, PSAs, OTC) were also asked to report the side effects they experience when using each type of sleep aid. As shown in Table 4, significantly more participants reported they experience red eyes and thirst when using cannabis compared to PSAs and OTC sleep medications. In contrast, significantly more participants reported that they experience nausea, anxiety, and racing heart when using OTC sleep medications or PSAs compared to cannabis. Finally, more participants reported paranoia as a side effect of PSAs than cannabis.
Reported side effects
| Side effects | Cannabis n (%) | PSA n (%) | OTC n (%) | Chi-square |
|---|---|---|---|---|
| Red eyes | 230 (43.7%a) | 44 (8.4%b) | 41 (7.8%b) | χ2 = 223.26, P < 0.001 |
| Thirst | 357 (67.9%a) | 146 (27.8%b) | 94 (17.9%c) | χ2 = 194.96, P < 0.001 |
| Nauseous | 13 (2.5%a) | 158 (30.0%b) | 95 (18.1%c) | χ2 = 119.24, P < 0.001 |
| Anxious | 45 (8.6%a) | 155 (29.5%b) | 109 (20.7%c) | χ2 = 59.26, P < 0.001 |
| Paranoid | 51 (9.7%a) | 95 (18.1%b) | 59 (11.2%a) | χ2 = 16.08, P < 0.001 |
| Racing heart | 52 (9.9%a) | 87 (16.5%b) | 102 (19.4%b) | χ2 = 16.39, P < 0.001 |
Percentages with no superscripts or the same superscripts do not differ significantly from those in the same row while those with different superscripts are significantly different from those in the same row at P < 0.05. Not applicable responses were as follows: red eyes = 191, thirst = 76, nauseous = 249, anxious = 229, paranoid = 285, racing heart = 269
Finally, participants were asked to indicate the average number of hours of sleep they obtain when they use cannabis, OTC medications, PSAs, and no sleep aids. As shown in Figure 1, the majority of the sample (n = 769, 63.2%) reported getting the recommended 6–8 h of sleep with cannabis alone, while less than 20% of the sample reported getting 6–8 h of sleep with a PSA (n = 186, 15.3%), OTC sleep medication (n = 159, 13.1%), cannabis combined with a sleep aid (n = 181, 14.9%), or when using no sleep aid (n = 116, 9.5%).
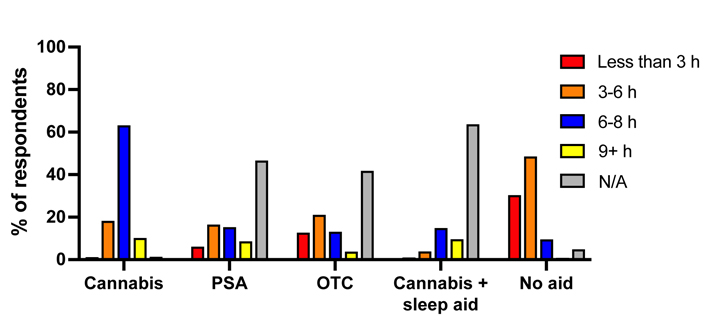
Percentage of sample reporting hours of sleep following use of various sleep aids. N/A: not applicable
Cannabis is commonly used to help with sleep. However, most previous studies on cannabis and sleep have not assessed which forms of cannabis are preferred to help with sleep or attempted to compare the perceived beneficial effects and side effects of cannabis compared to OTC sleep aids and PSAs. The results from this survey of respondents using cannabis to aid with sleep help to fill these gaps in the literature.
Findings from the current study indicate that cannabis is perceived to help relax the mind and body, as well as help achieve deeper, longer, and more uninterrupted sleep. These findings are consistent with the broader literature demonstrating that cannabis is often reported to relieve stress and tension [22], as well as some empirical evidence suggesting that cannabis is effective in improving objective measures of sleep disturbances. For instance, several placebo-controlled laboratory investigations have found that cannabis decreases objective sleep latency [21, 23, 24]. A similar laboratory study found that middle-of-the-night awakenings decreased with cannabis administration [25]. Similarly, a daily sleep diary study found that using cannabis as a sleep aid was associated with longer sleep duration and shorter middle-of-the-night awakenings but was also associated with increased next-day fatigue [26]. A separate cross-sectional survey of cannabis users and non-users found that cannabis use was associated with better overall sleep quality and reduced sleep latency [27]. Finally, other recent work indicates that using cannabis closer to bedtime was associated with decreased sleep latency, but not with nighttime awakenings [28]. Overall, the literature suggests that cannabis can be beneficial for some aspects of sleep, however, additional objective research is needed to determine which aspects of sleep are positively affected and which are negatively affected by cannabis.
The majority of participants reported that they prefer inhalation of cannabis via joints (46.1%) or vaping cannabis flower (42.6%) for sleep. This may be because of the short latency of onset with inhalation [29] and the high percentage of respondents who indicated difficulty falling asleep. It was somewhat surprising that only 33.8% of participants reported using edibles and 14.1% reported using capsules as these are longer lasting [29] and as such may be more beneficial for maintaining sleep. Nevertheless, these results are consistent with a cross-sectional survey of medical cannabis users’ patterns of use which revealed inhalation is the most common method of use [30].
Most participants (60%) in the present study also reported preferring high THC cannabis products for sleep which is also consistent with findings from broader medical cannabis studies [30]. Further, the vast majority (78.8%) reported specifically seeking THC in the cannabis they use for sleep and nearly half reported seeking CBD and the terpene myrcene. In line with these findings, one self-report study revealed that the use of higher concentrations of THC was associated with reports of shorter sleep onset latency and less difficulty falling asleep [24]. Similarly, prior studies have revealed that individuals with insomnia and greater sleep onset latency were more likely to report using cannabis products with higher concentrations of CBD [31] and one naturalistic study found that CBD is associated with significantly better self-reported symptom relief than THC [19]. In contrast, Nicholson and colleagues [21] found mixed effects of THC and CBD, such that THC was generally associated with sedating effects, while CBD was associated with alerting effects. Additionally, one rodent study on the terpene myrcene suggests that the terpene produces sedative effects [32]. Collectively, the self-report findings from the present study support the prior research indicating that THC, CBD, and myrcene may be beneficial for reducing sleep-related issues. Nevertheless, more controlled objective sleep studies manipulating concentrations of these cannabinoids and this terpene are needed to corroborate these self-reports.
More than half of the sample reported that they use cannabis as a sleep aid every night. Additionally, while over half of the sample reported using OTC sleep aids or PSAs in the past, the overwhelming majority (81.8%) reported that they do not currently use OTC sleep aids or PSAs, suggesting a potential drug-sparing effect with cannabis. Only a small percentage of the sample reported that they use cannabis in combination with their OTC sleep aids (4.4%) or PSAs (7.9%) which is encouraging as potential drug interactions between cannabis and sleep aids are poorly understood [33]. While the present study did not directly probe whether participants were specifically substituting their OTC sleep aids, and/or PSAs with cannabis, these findings are in line with past research indicating that more than half of medical cannabis users report using cannabis as a substitute for their prescription drugs [30] and that most medical cannabis users reported reducing or terminating their use of PSA and OTC sleep aids [11, 14].
Participants were more likely to self-report feeling more refreshed, more focused, better able to function, and experiencing fewer headaches and less nausea the morning after using cannabis relative to PSAs, OTC sleep aids, and no sleep aids. However, they also reported feeling more sleepy, anxious, and irritable the morning after cannabis use, relative to the morning after using OTC sleep aids, PSAs, and no aid. Unlike long-acting sedative-hypnotics and alcohol, cannabis is not associated with a “hangover” effect [34], however previous studies have found that people report feeling sleepy with fatigue, and changes in mood such as lethargy, inefficiency, an inability to concentrate, and dullness the morning after cannabis use [20, 21, 26]. Several studies have also examined the effects of OTC sleep medications and PSAs on next-day functioning. Adverse side effects related to prescription hypnotics tend to be dose and time dependent, such that higher doses and administration in closer proximity to waketime are associated with subjective and objective reports of impaired cognition and excessive daytime sleepiness [5, 35]. While widely used and available, less is generally known about any next-day effects of OTC sleep aids, and additional research is needed to fully understand the efficacy and potential side effects of these drugs [36, 37]. However, excessive daytime sleepiness has been reported as a possible side effect of melatonin and antihistamines [36]. While the present findings are novel, they are subjective and given that self-report sleep indices (e.g., latency to fall asleep) compare poorly to laboratory [e.g., electroencephalogram (EEG)] measures, more objective research is needed to compare morning outcomes after administering cannabis, OTC sleep aids, PSAs, or no sleep aid.
Previous research has revealed that sleep-related side effects from cannabis are rare [13] and medical users report that the side effects from prescription drugs are worse compared to those associated with medical cannabis [38], which is consistent with findings from the present study indicating that more people reported experiencing nausea, anxiety, paranoia, and racing heart as side effects of PSAs or OTC sleep medications than with cannabis. It is known that more conventional sleep aids can produce undesirable and potentially dangerous side effects such as drowsiness, decreased alertness and concentration, memory impairment, nausea, and negative affect [5–7]. Participants in the current study were only more likely to report experiencing dry mouth and red eyes when using cannabis compared to OTC sleep aids and PSAs, which is somewhat consistent with previous research demonstrating that dry mouth and red eyes are among the most reported adverse reactions to cannabis [30]. In general, the use of cannabis for sleep-related issues was perceived as more advantageous than OTC medications and PSAs. However, more controlled objective research is needed to verify these perceived effects as well as the levels of distress produced by side effects from OTC medications, PSA, and cannabis.
Limitations include potential selection bias, the use of a subjective measure of sleep and issues with some of the survey items, as well as the use of a cross-sectional survey design. Specifically, the sample comprised individuals already using cannabis for sleep; therefore, likely overrepresents individuals who find cannabis effective for their sleep issues. Similarly, most participants reported using cannabis for sleep for over one year so the extent to which the findings would generalize to less experienced users is unclear. Further, the majority of the sample reported multiple medical conditions and the degree to which cannabis is perceived to benefit sleep by providing symptom relief from these conditions is unclear.
The study is also limited by the use of retrospective self-reports of sleep which may be biased as individuals are often poor at subjectively assessing their sleep. As such, self-reports tend to be less accurate than objective investigations. Further, the use of an unvalidated survey that included the term “deeper sleep” may have produced less accurate results than a validated scale with the more conventional term “sleep quality” as the depth of sleep is often unknown by individuals and requires more objective means to measure in a valid manner. As such, future research should employ more traditional validated sleep scales and/or objective sleep measures. Additionally, the survey did not measure whether respondents were using other drugs/substances (e.g., alcohol, opioids) in combination with cannabis or what proportion of respondents were using illicit cannabis products as opposed to legal products subject to lab testing and labeling. The latter would be important with respect to their self-reported preferred products for sleep and their considerations of cannabinoids/terpenes in products used for sleep.
Finally, the cross-sectional nature of the study precludes the ability to establish causal or directional relations. Additionally, the degree to which self-reported effects are due to placebo effects is unknown.
Nevertheless, these limitations are offset by several strengths. Specifically, the obtained data were from a large sample of medical cannabis users who use a variety of cannabis products for a variety of sleep-related issues. As such, the study has high ecological validity and should translate to other individuals who use cannabis for sleep-related problems.
The present study expands upon prior research on medical cannabis and sleep by revealing that individuals who use cannabis for sleep-related problems prefer products high in THC, CBD, and the terpene myrcene; that combined use of cannabis with more conventional sleep aids is uncommon; and that cannabis is perceived to produce mixed morning outcomes and fewer side effects than more conventional sleep aids.
This study has medical and clinical implications for people suffering from sleep-related problems. Specifically, knowledge gained from this study will provide health professionals with a better understanding of why people are using cannabis instead of more conventional sleep aids. Additionally, the information gathered from this study may help guide future more controlled objective research comparing the effects, side effects, and morning outcomes of cannabis relative to more conventional sleep aids.
CBD: cannabidiol
OTC: over-the-counter
PSA: prescription sleep aid
THC: tetrahydrocannabinol
U.S.: United States
AS: Data curation, Formal analysis, Writing—original draft, Writing—review & editing. CC: Data curation, Formal analysis, Visualization, Project administration, Supervision, Writing—original draft, Writing—review & editing.
The authors declare they have no conflicts of interest.
The Washington State University Office of Research Assurances determined that this study was exempt from the need for review by the Institutional Review Board (IRB).
Strainprint® obtained informed consent from all participants as part of the terms of use of their platform.
Not applicable.
Data are available upon request to carrie.cuttler@wsu.edu.
Not applicable.
© The Author(s) 2023.
Copyright: © The Author(s) 2023. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Gregory Giordano ... Angela D. Bryan
Lucile Rapin ... Michael Dworkind
Elizabeth N. R. Schjelderup ... Alasdair M. Barr
Hannah Thurgur ... David J. Nutt
Cassandra L. Taylor, Schuyler A. Pruyn
Gerhard Nahler
Trevor R. Norman
