Affiliation:
3Department of Internal Diseases and Clinical Pharmacology, Medical University of Lodz, 91-347 Lodz, Poland
ORCID: https://orcid.org/0000-0002-7623-5389
Affiliation:
2Department of Cardiac Rehabilitation, The Biegański Hospital, 91-347 Lodz, Poland
ORCID: https://orcid.org/0000-0001-6297-2153
Affiliation:
1Chair and Department of Cardiology, Medical University of Lodz, 91-347 Lodz, Poland
ORCID: https://orcid.org/0000-0002-5850-8187
Affiliation:
1Chair and Department of Cardiology, Medical University of Lodz, 91-347 Lodz, Poland
ORCID: https://orcid.org/0000-0002-8194-0285
Affiliation:
1Chair and Department of Cardiology, Medical University of Lodz, 91-347 Lodz, Poland
Email: tomasz.rechcinski@office365.umed.pl
ORCID: https://orcid.org/0000-0001-7800-785X
Explor Cardiol. 2023;1:26–34 DOI: https://doi.org/10.37349/ec.2023.00004
Received: December 22, 2022 Accepted: March 28, 2023 Published: August 30, 2023
Academic Editor: Simon Rabkin, University of British Columbia, Canada
The article belongs to the special issue Common cardiovascular target for a wide gamut of contemporary health problems – thrombotic and arrhythmic sides of an inflammatory coin
Aim: The aim of this study was to compare initial and final exercise tolerance and to evaluate the determinants of exercise capacity improvement—after three weeks of inpatient cardiac rehabilitation.
Methods: A cohort of 494 patients after acute coronary syndrome (ACS), treated with primary coronary angioplasty (age 60 years ± 10 years, 27.5% women) was studied retrospectively. Possible correlations between improvement and age, gender, body mass index (BMI), left ventricular ejection fraction (LVEF) and the initial exercise capacity (EXT1) were assessed.
Results: The highest percentage of patients with improvement (43.6%) was in the medium tercile of LVEF (> 42% but ≤ 50%) and was more likely in the medium tercile of initial exercise tolerance [> 5.7 but ≤ 8.4 metabolic equivalent of tasks (METs)]. Receiver-operator characteristic (ROC) curves were developed and the following cut-off values were found: for LVEF > 43% (this value had 69.6% sensitivity in predicting improvement; the chance of improvement was 2.67 higher than in patients with LVEF ≤ 43%); for EXT1 ≤ 8.4 METs (this value had 70.8% sensitivity, the chance of improvement was 1.86 higher than in the other subgroup). No significant relationship between improvement and gender, age or BMI was found.
Conclusions: The combination of LVEF > 43% and EXT1 ≤ 8.4 METs relates to the highest probability of exercise tolerance improvement after cardiac rehabilitation.
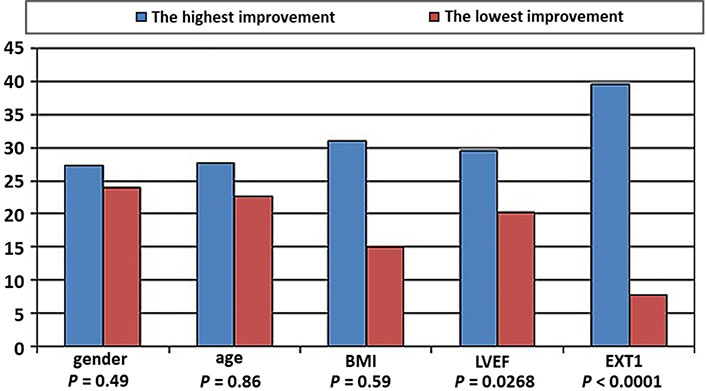
ACS patients referred to in-hospital cardiac rehabilitation (n = 492). Significance of differences in improvement of physical capacity between categories with the highest and lowest results
Cardiac rehabilitation after acute coronary syndrome (ACS) improves prognosis and quality of life [1, 2]. Despite its well-known beneficial effects [3], still not all patients are referred to rehabilitation [4]. Moreover, though new wards are created, the availability of rehabilitation is not always satisfactory. Currently, the centres which run programmes of rehabilitation after ACS offer them in three forms: stationary and two outpatient forms—in the centre and as telerehabilitation at the patients’ own homes. In addition, it is a fact that cardiac patients, even before starting the rehabilitation programme, ask the doctor what the expected effects of their participation in rehabilitation will be, since they are to spend the next few weeks on it. Therefore, it might be useful to determine in which patients’ cardiac rehabilitation will be the most efficient. In the present study, the aim was to investigate whether simple and easily acquired data may be informative of potential results of cardiac rehabilitation.
The study group of this retrospective study consisted of 494 patients after ACS, treated with primary coronary angioplasty. The mean age was 60 years ± 10 years, and 27.5% of subjects were women. The prevalence of modifiable risk factors is presented in Figure 1.
All the patients underwent an inpatient cardiac rehabilitation programme involving 3 weeks of physical training, 5 sessions a week. This cardiac rehabilitation programme included endurance and resistance training. The exercises were conducted with the use of cycloergometer, stepper, multi-gym as well as the following equipment: weights, balls, exercise bands. The daily training plan included: in the morning—30 min of general exercises, at noon—interval training using a cycloergometer, and in the afternoon—general improving exercises combined with resistance exercises or Nordic walking classes. The type and intensity of the exercises were determined by a physician who based it on the patient’s clinical status and on the results of the treadmill exercise test or of cardiopulmonary exercise testing. During the exercises, heart rate and blood pressure were monitored and the whole session was supervised by a physiotherapist. This comprehensive cardiac rehabilitation programme also included psychological care as well as dietary and educational components.
The benefit from cardiac rehabilitation, i.e., improvement of exercise capacity (IMPR)—is understood as increased exercise capacity in the final exercise capacity (EXT2) compared to the result of the initial exercise capacity (EXT1). It is also calculated as the proportion between the results of the EXT2 and EXT1 [based on metabolic equivalent of tasks (METs)] and expresses in percentages [IMPR (%)] using the following equation: [(EXT2/EXT1) – 1] × 100%. The possible impact on IMPR of the following parameters is assessed: age, gender, body mass index (BMI), left ventricular ejection fraction (LVEF) and the EXT1. Age, LVEF, EXT1, BMI are analysed as real numbers but are subsequently transformed into categorical variables: terciles according to age, LVEF, EXT1 and 5 categories of BMI.
Initially, the group is divided according to IMPR as a binary variable (improvement obtained or no improvement). The subsets are checked for differences regarding age, BMI, LVEF, EXT1 using a student’s t-test or the Mann-Whitney test. Then using a χ2 test, the percentage of patients with or without improvement in the terciles of age, LVEF, EXT1 and 5 categories of BMI is assessed. In order to assess the relationship between age, BMI, LVEF, EXT1 and IMPR (%), correlation analysis (Spearman’s rank correlation coefficient) is performed. The relationship between IMPR (%) and the categorical variables is analyzed using the Mann-Whitney or the Kruskal-Wallis test. Receiver-operator characteristic (ROC) curves are developed for variables which are found significant in the initial analysis to determine the cut-off values optimal for IMPR prediction. P < 0.05 is considered to be statistically significant.
The patients in whom improvement is obtained had significantly higher LVEF than the patients with no improvement (47.0% ± 9.2% vs. 43.4% ± 9.6%, P = 0.0002). The highest percentage of patients with IMPR (43.6%) and the lowest percentage of patients without IMPR (24.1%) are observed in the medium tercile of LVEF values (higher than 42% but ≤ 50%); the percentage of patients with IMPR is lower in the first and third tercile (27.2% and 29.2% of patients with IMPR, respectively, P < 0.0001). Also, IMPR is more likely in the medium tercile of EXT1 > 5.7 but ≤ 8.4 METs than in the other two terciles (P = 0.0078). The highest percentage of patients without IMPR (43.5%) belongs to the third tercile EXT1 > 8.4 METs. Details are presented in Tables 1 and 2.
Differences between the subgroups with or without IMPR (terciles for age, LVEF and EXT1 or pentiles for BMI)
| Categorical variables | The percentage of patients within the tercile or category in the subgroup with IMPR | The percentage of patients within the tercile or category in the subgroup without IMPR | P |
|---|---|---|---|
| Age | |||
| ≤ 56 years | 37.5% | 31.7% | 0.4596 |
| > 56 years but ≤ 64 years | 32.4% | 34.5% | |
| > 64 years | 30.1% | 33.8% | |
| Gender | |||
| Male | 73.1% | 69.7% | 0.4417 |
| Female | 26.9% | 30.3% | |
| BMI | |||
| ≤ 25 | 19.5% | 28.9% | 0.1816 |
| > 25 but ≤ 30 | 50.4% | 42.8% | |
| > 30 but ≤ 35 | 23.2% | 20.7% | |
| > 35 but ≤ 40 | 5.2% | 4.8% | |
| > 40 | 1.7% | 2.8% | |
| LVEF | |||
| LVEF≤ 42% | 27.2% | 49.7% | < 0.0001 |
| > 42% but ≤ 50% | 43.6% | 24.1% | |
| > 50% | 29.2% | 26.2% | |
| EXT1 | |||
| ≤ 5.7 METs | 35.0% | 30.3% | 0.0078 |
| > 5.7 METs but ≤ 8.4 METs | 35.8% | 26.2% | |
| > 8.4 METs | 29.2% | 43.5% | |
Differences between the subgroups with or without IMPR
| Variable | In the subgroup with IMPR Mean ± SD | In the subgroup without IMPR Mean ± SD | P |
|---|---|---|---|
| Age | 59.8 ± 10 | 61.6 ± 9.9 | 0.0617 |
| BMI | 28.4 ± 4.2 | 28 ± 5 | 0.1713 |
| LVEF | 47 ± 9.2 | 43.4 ± 9.6 | 0.0002 |
| EXT1 | 7.1 ± 2.9 | 8.2 ± 6.5 | 0.0556 |
As far as IMPR (%) is concerned, there is a positive correlation with the LVEF value (correlation coefficient r = 0.0887, P < 0.05) and a negative correlation with the EXT1 value (r = −0.316, P < 0.05). Generally, this shows that cardiac rehabilitation is the more effective the higher LVEF the patients have, but also the lower exercise capacity they present in the EXT1. In patients within the medium tercile of LVEF, the IMPR (%) value is 29.6%, which is significantly better than the IMPR (%) value of 20.2% in the first tercile, P = 0.0227. In patients who obtain EXT1 values > 8.4 METs (the highest or third tercile), the IMPR (%) value is only 7.8%, while in the medium tercile it is 26.9% and in the first tercile it is the most prominent—39.7%. These differences are significant with P < 0.0001. Details are presented in Tables 3 and 4.
The relation between the IMPR and the patients’ characteristics (terciles for age, LVEF and EXT1 or pentiles for BMI)
| Categorical variables | Mean IMPR (%) ± SD | P |
|---|---|---|
| Age | ||
≤ 56 years > 56 years but ≤ 64 years > 64 years | 22.7 ± 32 24.4 ± 32 27.7 ± 46.7 | 0.8681 |
| Gender | ||
Male Female | 27.3 ± 43.5 23.9 ± 34.4 | 0.4961 |
| BMI | ||
≤ 25 > 25 but ≤ 30 > 30 but ≤ 35 > 35 but ≤ 40 > 40 | 22.4 ± 35 24.1 ± 33.8 31 ± 47.7 18.7 ± 23.7 15.2 ± 27.6 | 0.5928 |
| LVEF | ||
≤ 42% > 42% but ≤ 50% > 50% | 20.2 ± 32.8 29.6 ± 44.3 23.9 ± 30.6 | 0.0268 |
| EXT1 | ||
≤ 5.7 METs > 5.7 METs but ≤ 8.4 METs > 8.4 METs | 39.7 ± 50.4 26.9 ± 27.2 7.8 ± 18.4 | < 0.0001 |
The relation between the IMPR and the patients’ characteristics
| Variable | Correlation coefficient r for IMPR (%) | P |
|---|---|---|
| Age | −0.0097 | NS |
| BMI | 0.0408 | NS |
| LVEF | 0.0887 | < 0.05 |
| EXT1 | –0.316 | < 0.05 |
NS: nonsignificant
No significant relationship between IMPR or IMPR (%) and gender, age or BMI is found (the above tables). Therefore, only LVEF and EXT1 are included in the further analysis.
A ROC curve for LVEF is developed (Figure 2) and a cut-off value which allows to predict correctly the probability of improvement in 65% of patients is identified. This improvement is related to LVEF > 43%, while lack of improvement is related to LVEF ≤ 43%. The area under the curve (AUC) is 0.607 [95% confidence interval (CI), 0.562–0.650]. The chance of improvement is 2.67 higher in subjects with LVEF > 43% than in those with LVEF ≤ 43%. For this cut-off value, sensitivity is 69.6%, specificity—53.8%, the positive predictive value is 78.4% and the negative predictive value is 42.4%.
A ROC curve is also developed for EXT1 (Figure 3) and a cut-off value is found that allow to correctly predict the probability of improvement after the rehabilitation programme in 62.8% of patients. This improvement is related to EXT1 ≤ 8.4 METs, while lack of improvement is related to EXT1 > 8.4 METs. AUC is 0.555 (95% CI, 0.510–0.599). The probability of improvement is 1.86 higher in subjects with EXT1 ≤ 8.4 METs than in those with > 8.4 METs. For this cut-off value, sensitivity is 70.8%, specificity—43.4%, the positive predictive value is 75.1% and the negative predictive value is 38.2%.
The performance in the exercise test is an important prognostic factor in patients after myocardial infarction. Better exercise tolerance is related to favourable prognosis [5, 6]. The results of this study indicate that the value of exercise capacity before the physical exercise programme as well as ejection fraction (rather than age, gender or BMI) should be considered in qualifying patients after ACSs for a stationary rehabilitation programme in order to achieve the highest improvement in physical exercise capacity. These findings are in opposition to some previously published studies.
In previous studies it was noted that women rarely undergo cardiac rehabilitation and that they represent only 20–30% of all patients [7]. Female gender was related to older age, greater cardiovascular burden, and more days needed to complete the rehabilitation programme in comparison with men. Women were also more likely to drop out during the training cycle [8]. In a study conducted among 60 female and 172 male patients, who participated in a minimum of 10 out of the 24 training sessions recommended in an outpatient cardiac rehabilitation ward, significant improvement in exercise capacity was obtained by both genders, but in women the improvement assessed in a 6-min walk test was even greater [9]. However, there is also evidence in the literature that patients may benefit from cardiac rehabilitation similarly regardless of age or gender [10]. In this study population, women were in the minority. However, neither age nor gender was a notable determinant of the improvement achieved.
In a large group of 3,997 patients with coronary artery disease, participating in a 12-week cardiac rehabilitation programme, it was suggested that improvement in obese subjects was significant, but less prominent than in their non-obese counterparts [11]. The results of this study do not support that conclusion, because IMPR (%) was not different in consecutive BMI categories.
Previous studies and guidelines indicate that the lack of damage to the left ventricle after myocardial infarction should not discourage participation in a rehabilitation programme. On the other hand, a low LVEF (< 35%) indicates a high cardiac risk during exercise [12, 13].
In presented study LVEF ≤ 43% was in fact an indicator of poor improvement in the physical exertion capacity. The results allow authors to speculate that perhaps in patients with LVEF ≤ 43% a differently designed rehabilitation programme could be more effective [14].
To the authors’ knowledge, though EXT1 is widely used for the purposes of rehabilitation course planning, it was not described as a powerful predictor of rehabilitation effectiveness before. Since higher LVEF may not be accompanied by higher exercise tolerance in some patients, it seems reasonable to take into consideration both parameters simultaneously.
The authors are aware of some limitations of the presented study. First of all, a distinction is not done between patients with different types of ACS—unstable angina, non-ST-elevation myocardial infarction or ST-elevation myocardial infarction. The only measure of consequences of the advancement of coronary atherosclerosis is the systolic function of the left ventricle and not the number of previous coronary events, the number of diseased coronary arteries or the number of percutaneous coronary interventions).
The next limitation of this study is the issue of compliance to the recommended pharmacotherapy. It can be only assumed that, as those were hospital patients, the adherence to medical therapy was supervised by medical staff and it was equal or close to 100%.
Also, the calculation of improvement is a disputable aspect of this study. It is chosen to show it as the proportion between final and initial results. It has to be emphasized, however, that an improvement of 1.5 METs will be a 12.5% better result for a patient who begins the cardiac rehabilitation program with the capacity of 12 METs, and 50% for one who begins it with 3 METs.
Some available meta-analyses provide evidence that cardiac rehabilitation reduces mortality or the re-hospitalization rate—since it was not the aim of the study, information from the follow-up of these patients is not presented [15, 16]. Also, information about the impact of comorbidities (chronic obstructive pulmonary disease, rheumatoid arthritis or thyroid diseases, etc.) as well as the influence of psychological factors (e.g., type D or type A personality) are not involved in the analysis.
The authors conclude that according to their results, the most promising target subgroup of patients in whom significant improvement in physical exertion capacity may be expected, are those with ejection fraction > 43% but EXT1 limited to ≤ 8.4 METs. This information may be of importance for physicians deciding about the referral to one of three available forms of cardiac rehabilitation: stationary, outpatient, or telerehabilitation, and in the discussion with patients about to start cardiac rehabilitation on the subject of their expectations of the effects of the programme.
In the future it would be interesting to analyse the correlation between the profiles of patients and the form of rehabilitation, that is, to establish which patients would benefit more from stationary rehabilitation and which from a form of non-stationary rehabilitation.
ACS: acute coronary syndrome
BMI: body mass index
EXT1: initial exercise capacity
EXT2: final exercise capacity
IMPR: improvement of exercise capacity
LVEF: left ventricular ejection fraction
METs: metabolic equivalent of tasks
ROC: receiver-operator characteristic
We thank Mr. Janusz Wróblewski, for his linguistic help with the manuscript and Ms. Aneta Rózga for her statistical calculations.
BUL and TR: Conceptualization, Investigation, Writing—original draft. EW, KWD and UCG: Investigation, Date curation. JDK and MK: Validation, Writing—review & editing, Supervision. All authors read and approved the submitted version.
The authors declare that they have no conflicts of interest.
The protocol of presented study was approved by the Local Ethics Commission at Medical University of Lodz, Poland. This manuscript complies with the Declaration of Helsinki.
Informed consent to participate in the study was obtained from all participants.
Not applicable.
The datasets analyzed for this study can be obtained from the corresponding author.
Not applicable.
© The Author(s) 2023.
Copyright: © The Author(s) 2023. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 3323
Download: 24
Times Cited: 0
Bogusława Nowak ... Karina Wierzbowska-Drabik
Piotr Hamala, Karina Wierzbowska-Drabik
Maria Możdżan ... Karina Wierzbowska-Drabik
Annamaria Del Franco ... Iacopo Olivotto
Miłosz Broncel, Marlena Broncel
