Affiliation:
1Department of Cardiology, University of Belgrade and Serbian Heart Foundation, 11000 Belgrade, Serbia
Email: mostojic2011@gmail.com
ORCID: https://orcid.org/0000-0002-1250-7461
Affiliation:
2Department of Neurology, Medical Faculty, University of Banja Luka, 51000 Banja Luka, Bosnia and Herzegovina
Affiliation:
2Department of Neurology, Medical Faculty, University of Banja Luka, 51000 Banja Luka, Bosnia and Herzegovina
ORCID: https://orcid.org/0000-0002-7100-5189
Affiliation:
2Department of Neurology, Medical Faculty, University of Banja Luka, 51000 Banja Luka, Bosnia and Herzegovina
ORCID: https://orcid.org/0000-0001-6661-904X
Explor Cardiol. 2023;1:35–41 DOI: https://doi.org/10.37349/ec.2023.00005
Received: April 07, 2023 Accepted: June 01, 2023 Published: August 31, 2023
Academic Editor: Andrea Borghini, Institute of Clinical Physiology-National Research Council (IFC-CNR), Italy
Alcohol drinks, especially wine, have been described since 6,000 B.C. For many years in modern medicine, wine in moderation has been considered healthy for cardiovascular prevention, i.e., recommended by nutrition committees. Some regional guidelines still recommend one to two standard drinks per day. By the very recent (January 2023), World Health Organization and Canadian Guidance on alcohol emphasize that any alcoholic drink is hazardous to the health and the safe amount is zero. The risk starts with every single drop. It was also nicely summarized in the manuscript “Alcohol-dose question and the weakest link in a chemical interplay” (Explor Cardiol. 2023;1:15–25. doi: 10.37349/ec.2023.00003) especially from the standpoint of a researcher in the cardiovascular arena. The newest recommendations are based on observational studies and their meta-analysis, therefore establishing associations, pointing out that alcohol may somewhat prevent cardiovascular diseases and diabetes type 2, but with a significant increase in non-cardiovascular morbidity and mortality, especially cancers. Previous recommendations, therefore, may be obsolete as they were based on studies where abstainers from alcoholic beverages had inherent higher risks. The current controversy with conflicting guidelines for alcoholic beverage consumption in the era of precision medicine may stimulate more fundamental investigations up to genetic ones and find the cause-effect relations. In the era of precision medicine, it may come closer to discovering the causes of cancers and many other diseases, enabling predictions of reactions to alcoholic beverages by each person, not just in the population.
“Now, this is not the end. It is not even the beginning of the end. But it is, perhaps, the end of the beginning”—Winston Churchill (November 10, 1942 regarding the first military successes of the British army in North Africa).
Alcohol! The first image it brings to mind for most of us is a pitcher of red wine, parties, celebrations, having a good time, and of course, its health benefits for the cardiovascular system. In an article published in this issue of Exploration of Cardiology—“Alcohol-dose question and the weakest link in a chemical interplay” with an excellent overview of controversial effects on alcohol, as also seen by the authors’ original research (reference 22 in their overview), and by the research of the others [1], as well as a very recently published World Health Organization (WHO) Newsletter [2] and “Canada’s Guidance on alcohol and health” [3] claim that any amount of alcohol consumed can pose a risk to human health. The risk starts with the first drop. Although, Canadian Guidance does state, perhaps more as a consolation, that one or two standard drinks a week pose only a small risk to our general health (1 of 1,000 consumers may die prematurely). The equivalent of one standard drink is a glass of wine (142 mL, 12% alcohol), a bottle of beer (341 mL, 5% alcohol), a shot of hard liquor (43 mL, 40% alcohol) or a small bottle of cider (341 mL, 5% alcohol), altogether 17 mL or 13.6 g alcohol. Some countries have guidelines for a standard drink in milliliters and some in grams or glasses, although glasses can be of different sizes, which could be a bit confusing, too. Although, over recent years, guidelines all over the world have been showing a decreasing trend in the recommended safe doses of alcohol, so the zero-intake recommendation should not come as a surprise [1].
Let’s take wine, for example, it’s been manufactured since 6,000 B.C. It was first described in the Caucasus and then in Persia, Roman Empire, Armenia, etc. In Serbia, the first description of wine has been dating back to 2,200 B.C. in The Age of Bronze, and it has been with us ever since. France, the second largest wine manufacturer (preceded only by Italy) and the largest exporter of wine, was introduced to wine in 600 B.C. For centuries, the highest quality wine has been an exclusive privilege of tzars, kings, and emperors [4]. There is well known so-called French paradox [5]. Namely, the French people have fewer cardiovascular illnesses, although they share similar risk factors with other countries, presumably because of France’s high levels of red wine consumption, which was not true because of the effect of confounders.
Now, 8,000 years later, we have an interesting situation, as some still valid guidelines, such as the American nutrition guidelines for 2020 to 2025, although they do not recommend that people who do not consume alcohol should start to do so, they still recommend two standard drinks per day for men and one for women, equating to 14 or 7 standard drinks per week, respectively [6]. So, can we afford to ignore the WHO and Canadian guidelines, then? Yes, we can; however, if the recommendations prove correct, they won’t benefit our health. The dilemma is especially important for medical professionals, who need to provide advice to their consumers (by consumers, we mean the consumers of medical knowledge and information, as many of them are not yet our patients). For example, in the interview of Miodrag Ostojic with the oldest daily newspaper in the Balkans, on September 17, 2008, it was recommended that 150 mL of red wine might be consumed three times a week (having reduced the recommended dose and actually come closer to the recently recommended Canada’s Guidance, to avoid leading the public to the conclusion that if a little bit of something is healthy, more of the same will be even more beneficial), and emphasizing that this consumption could lead to some reduction in the occurrence of cardiovascular illness (as stated in the recommendations), without saying that that level of consumption would only pose a small risk to their health. Soon, a written comment came by an anonymous reader: “it was inappropriate for Professor Ostojic to propagate the consumption of alcohol at all” (the original interview may be obtained by demand from the personal file of Miodrag Ostojic). It was an excellent, thoughtful comment, which also turned out to be prophetic, as it predicted the recent Canada’s Guidance.
Recommendations about nutrition tend to be based on observational studies, as randomized controlled studies are rare. In contrast with the tobacco industry, which is still profitable, though, where the manufacturers are strictly regulated in the ways they market their products or influence federal and state institutions to promote their interests, the food and alcohol manufacturing industry enjoys the lack of regulations, which enables the alcohol manufacturing industry to promote its interests freely by marketing their products and influencing and lobbying the federal and state governing and regulatory bodies. For example, there was a randomized control study that started on February 5, 2018 called Moderate Alcohol and Cardiovascular Health Clinical Trials (MACH), with a budget of 100 million dollars [similar to the International Study of Comparative Health Effectiveness With Medical and Invasive Approach (ISCHEMIA) trial] and was supposed to include 7,800 people older than 50 years of age, with a risk of cardiovascular disease greater than average.
It was to follow the occurrence of diabetes mellitus type II (DM2) or cardiovascular disease over six years in people who consume one standard drink a day, 15 g to 17 g of alcohol, in comparison to people who do not consume alcohol at all. It is significant to emphasize that in forming the budget for this research, two-thirds of the financing companies contributing to the budget consisted of major alcohol manufacturers. Somehow, because of the irregularities in negotiating the budget and designing the research protocol on June 15, 2018 National Institute for Health found a way to abort the research only after 105 random patients were studied (half of which were sipping wine for free). Consequently, the grant was withdrawn [7, 8]. As a scientific explanation for grant withdrawal, which has rarely happened, the Mendelian randomization analysis study, which found the hazardous effect of alcohol, was cited [9]. However, Mendelian randomization studies have their inherent limitations [10].
Almost 20 years ago, as a reaction to the polypill manuscript, an article was published in the same journal (British Medical Journal, 2004) about polymeal, healthy nutrition that’s more delicious than polypill and which would be effective in 75% of cases in the primary prevention of cardiovascular diseases, and as part of which, apart from garlic and vegetables, the biggest effect on cardiovascular health has a daily glass of red wine (150 mL), providing the prevention rate of 32% [11]. But those calculations for polypill and polymeal have not been achievable in practice, thus outlining their shortcomings.
Recently, on October 17, 2022 there was a paper published in The American journal of Clinical Nutrition [12] (which was not cited in Canada’s Guidance, probably because of the timing of the publication), where the United Kingdom (UK) Biobank was followed by 312.388 patients without DM2 in the duration of 10.9 years (median), where it was found that with those patients who were consuming alcohol moderately and mostly in the form of wine and, it is very important to emphasize, during the meal, not on an empty stomach, there is a 12% less risk of suffering from DM2 (mostly with the people who consumed more than 100 g and less than 200 g a week, as assessed by a questionnaire) which was one of the final goals of the aborted MACH study [12]. Dr. Keneth Mukmal, the lead researcher of the MACH study, whose 100-million-dollar funding was withdrawn, published in the same journal editorial titled “Limited alcohol consumption and lower risk of diabetes: can we believe our own eyes?” [13]. But it should be outlined the limited value of periodic questioners in nutritional science [14].
In addition, on October 7, 2022 a paper was published in The American journal of Clinical Nutrition (which also was not cited in Canada’s Guidance) from Sao Paulo, Brazil. It is a three-week randomized “crossover” study, including 42 men consummating 250 mL of red wine daily, five days a week. It studied its influence on the metabolome in the blood and gut microbiota and found some beneficial changes [15]. The research on gut microbiota is the hottest topic in medicine today. The pharmaceutical industry invests vast amounts of money in promoting healthy changes in gut microbiota use in human treatment.
However, it has to be emphasized that Canada’s Guidance does not negate the “J” curve for alcohol, ischemic heart disease and DM2 (as if they have referenced the work published by UK Biobank researchers). Still, moderate alcohol consumption as outlined in Canada’s Guidance, increases the risk of some subtypes of cardiovascular diseases like hypertension, atrial fibrillation and hemorrhagic stroke.
So, if alcohol can decrease cardiovascular mortality and the occurrence of diabetes, which non-cardiovascular mortality does it increase then? The risk of mortality is caused by malignant diseases, especially oropharyngeal, laryngeal, liver, colorectal, breast malignancy [16, 17], liver cirrhosis, epilepsy, not to mention death by violence, traffic accidents, etc. The proportion of drinkers worldwide has remained the same since 1990; due to population growth, absolute numbers increased from 983 million to 1.34 billion in 2020. An especially worrisome fact is that 59.1% belong to the 15–39 year age group [16].
In Figure 1, possible harms and benefits are presented. The argument that a decrease of DM2 will decrease its related diseases has not been proven by any study [17].
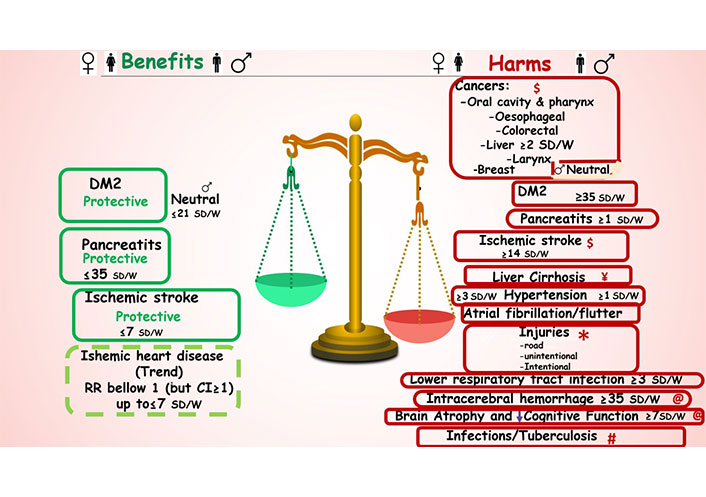
Alcohol effects as estimated by relative risk (RR) and confidence intervals (CI) and diagnostic tools on different diseases derived and compiled from references [2, 3, 8, 12, 16, 17, 21, 22]. If framed text is in the center relates to both genders. Subarachnoid hemorrhage had a RR, RR > 1, but a high CI, so not significant: therefore not presented being neutral. If the number of standard alcoholic drink per week (SD/W) is not filled in, it is ≥ 1. The highest relative proportions of disability-adjusted life years (DALYs) for causes associated with harmful alcohol consumption were reported by Global Burden of Diseases researchers by super-region, age group, and sex in 2020. $ Cancers: high-income countries in age group 40–64 years; ¥ liver cirrhosis: Central Europe, Eastern Europe, and Central Asia, Latin America and Caribbean, South Asia and Sub-Saharan Africa, especially males; * injuries: 15–39 years in all regions; @ intra cerebral hemorrhage and brain atrophy and decrease in cognitive function: high-income countries in age group ≥ 65 years, hypertension, high body mass index and low educational level are predisposing risk factors; # tuberculosis: low-income countries in the age group 15–40 years
It is still under debate if moderate consumption of alcohol may lead to systolic and/or diastolic heart failure [18–20].
Also, it has been shown in numerous studies that alcohol is bad for brain health. In an observational study of 25.378 UK Biobank participants, no safe level of alcohol consumption for brain health was found, as estimated by magnetic resonance imaging and cognitive tests [21]. One study found that using one standard drink more (a glass of wine) was associated with brain changes equivalent to two years of aging [22].
Interestingly enough, previous studies (some iconic, like Framingham Heart Study and Seven Countries Study) on which previous recommendations were based analyzed the effects of alcohol on cancer, brain health, and heart failure, with the conclusion that was no harm induced in moderate drinkers [23–29]. Previous recommendations, therefore, may be obsolete as they were based on studies where, as found by additional analysis, abstainers from alcoholic beverages had inherent higher risks [8].
As previously stated, most of our scientific knowledge in these recommendations is based on observational studies, which point out a link between alcohol consumption and different illnesses. Our calculations are usually considered correct until proven wrong. Everyone knows at least someone who has spent their life drinking alcohol daily and yet lived a very long life. To be clear, here, in this text, we do not discuss or refer to alcoholism as an addiction but rather to the effects of consuming small or moderate doses of alcohol.
Recently, a Yellow III study was reported on the American College of Cardiology in 2023, showing that 20% of patients on statins and proprotein convertase subtilisin/kexin type 9 inhibitors do not display any positive effects of fibrous cap thickness and cholesterol content in the plaque. As the genome analysis of these patients’ peripheral blood mononuclear cells explained these results, there is hope that genetic blood tests could be developed to predict non-responders. Similarly, we need genome studies for alcohol consumption that could uncover any possible cause-and-effect connections.
In any case, the intention of this text is not to spoil the pleasure of socializing but to focus on alcohol indulgence, which will only in the years ahead be studied in detail to explain and further expand our collective knowledge.
The current controversy, with conflicting guidelines for alcoholic beverage consumption, may stimulate more fundamental investigations up to genetic ones and find the cause-effect relations in the era of next-generation evidence-based medicine [30], i.e., precision medicine.
Hopefully, we may come closer to discovering the causes (etiopathogenesis) of cancers and many other diseases, enabling us to predict reactions to alcoholic beverages by each person, not just in the population. “The risk starts with the first drop” [2]. “Canada has a right to know” [3]. The planet should not ignore these dramatic warnings.
Regarding ignoring the alcohol zero paradigm then, Albert Einstein’s quote (Weak people revenge. Strong people forgive. Intelligent people ignore), may sound too cynical. On the other side, Max Plank’s quote (Nobel Prize winner 1918): “The new scientific truth does not triumph by convincing its opponents and making them see the light, but rather because its opponents eventually die and a new generation grows up that is familiar with it” sounds too pessimistic.
Very subtle and balanced statement of Dr. Emmanuela Gakidou (corresponding author of “Global Burden of Diseases 2020 Alcohol Collaborators research” [16]. (which has already undergone criticism) hopefully will resonate with medical professionals and the lay public “Our message is simple; young people should not drink, but older people may benefit from drinking small amounts. While it may not be realistic to think young adults will abstain from drinking, we do think it’s important to communicate the latest evidence so that everyone can make informed decisions about their health”. That statement is compatible with common sense.
Our manuscript aims to highlight the above-mentioned new knowledge, which may be controversial to the previous, and inspire further research in the era of precision medicine to be enjoyed by new generations.
DM2: diabetes mellitus type II
MACH: Moderate Alcohol and Cardiovascular Health Clinical Trials
UK: United Kingdom
MO: Conceptualization, Data curation, Formal analysis, Methodology, Funding acquisition, Project administration. VD, TKP, and DV: Data curation, Formal analysis, Investigation, Methodology.
The authors declare that they have no conflicts of interest.
Not applicable.
Not applicable.
Not applicable.
Not applicable.
Not applicable.
© The Author(s) 2023.
Copyright: © The Author(s) 2023. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 9298
Download: 29
Times Cited: 0
