4 results in Exploration of Cardiology
Latest
Sort by :
- Latest
- Most Viewed
- Most Downloaded
- Most Cited
Open Access
Case Report
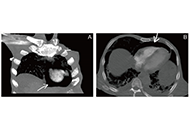
Uncommon threads: pneumopericardium complexity following liver catheter removal in pancreatic cancer
Ahmed Basuoni ... Marwa Makhlouf
Published: August 06, 2024 Explor Cardiol. 2024;2:178–182
Open Access
Protocol
Vascular senescence and atherosclerotic plaque vulnerability: investigating the telomere-mitochondria crosstalk—rationale and design of the VICTORIA Study
Jonica Campolo ... Maria Grazia Andreassi
Published: July 24, 2024 Explor Cardiol. 2024;2:168–177
This article belongs to the special issue Molecular Mechanisms of Cardiovascular Aging

Open Access
Original Article
Percutaneous versus open cannulation for mechanical support in patients with right ventricular failure after left ventricular assist device placement
Amit Prasad ... Behzad Soleimani
Published: July 18, 2024 Explor Cardiol. 2024;2:158–167

Open Access
Case Report
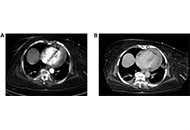
Cardiac tamponade after thrombectomy
Shruthi Sivakumar ... Suzette Graham-Hill
Published: July 17, 2024 Explor Cardiol. 2024;2:148–157
Journal Information