Affiliation:
1Department of Medicine, Amiri Hospital, Ministry of Health, Kuwait City 13110, Kuwait
†These authors contributed equally to this work.
Affiliation:
2Department of Microbiology, College of Medicine, Kuwait University, Kuwait City 13110, Kuwait
3Department of Allergy, Al-Rashed Allergy Center, Ministry of Health, Kuwait City 13110, Kuwait
†These authors contributed equally to this work.
Email: mona.alahmad@ku.edu.kw
ORCID: https://orcid.org/0000-0003-2950-5363
Affiliation:
3Department of Allergy, Al-Rashed Allergy Center, Ministry of Health, Kuwait City 13110, Kuwait
4Department of Laboratory Medicine, School of Medicine, Jiangsu University, Zhenjiang 212013, Jiangsu, China
5Department of Pulmonary Medicine, Abbassia Chest Hospital, Ministry of Health, Cairo 11517, Egypt
†These authors contributed equally to this work.
ORCID: https://orcid.org/0000-0002-7421-5085
Explor Asthma Allergy. 2024;2:118–126 DOI: https://doi.org/10.37349/eaa.2024.00034
Received: July 01, 2023 Accepted: February 29, 2024 Published: April 19, 2024
Academic Editor: Lawrence DuBuske, George Washington University Hospital, Immunology Research Institute of New England, United States
The article belongs to the special issue The Global Picture of Asthma after Guideline Changes and the COVID Pandemics
Aim: Asthma represents a significant health burden in Kuwait, with high prevalence rates among adults and children. Most asthma patients rely on government healthcare facilities for management, so there is a pressing need to optimize asthma care and treatment strategies. A cross-sectional paper-based survey was conducted to gather insights from allergists and pulmonologists across various healthcare facilities in Kuwait.
Methods: Twenty-six medical professionals participated, sharing their perspectives on asthma management practices and adherence to the Global Initiative for Asthma (GINA) 2022 guidelines through answering a modified single round Delphi survey.
Results: A high level of consensus on the practicality of guideline changes and the importance of spirometry in diagnosis were reported. However, agreement varied regarding optimal management strategies and medication preferences, indicating areas of divergence among experts. Notably, while there was strong support for inhaled corticosteroid (ICS)-long-acting β2 agonist (LABA) therapy during exacerbations, opinions differed on the use of short-acting β2 agonist (SABA) inhalers as rescue medication. Additionally, the study highlighted challenges in achieving higher levels of agreement, particularly regarding the frequency of inhaler technique checks and specialist referrals for severe asthma cases.
Conclusions: This study provided valuable insights into current asthma management practices in Kuwait and identified opportunities for consensus-driven strategies aligned with GINA guidelines. By incorporating diverse perspectives from expert allergists and pulmonologists, it contributed to the enhancement of asthma care and patient outcomes in Kuwaiti healthcare settings.
Asthma imposes a significant healthcare challenge in Kuwait, with prevalence rates ranging from 11% to 15% in adults and 18% in children [1]. The reliance on government healthcare facilities for asthma management is notable, with 90% of adults and 84% of children seeking care from these facilities [2].
In our pursuit of enhancing patient outcomes, a paper-based questionnaire resembling the structured consensus-building technique of Delphi methods with only a single round had been implemented [3]. This approach facilitated the collection of expert opinions from allergists and pulmonologists practicing in Kuwait. Experts were selected based on their specialized knowledge of asthma management across various healthcare facilities.
This study endeavors to comprehensively grasp contemporary asthma management practices by integrating varied perspectives. Through this methodology, the objective is to pinpoint prevailing deficiencies and formulate consensus-based strategies in line with the latest Global Initiative for Asthma (GINA) 2022 guidelines [4]. By bridging the divide between expert opinion and adherence to guidelines, the aim is to enhance the delivery of asthma care in Kuwait.
A cross-sectional paper-based survey was conducted throughout March 2023. A paper-based survey was created resembling the structured consensus-building technique of Delphi methods with only a single round [3], and participants were invited to complete the form. Allergists and pulmonologists working in Kuwait were invited to participate in the survey.
To determine the sample size, Minitab 17.1.0.0 for Windows (Minitab Inc., 2013, Pennsylvania, USA) was used. The expected frequency of allergists and pulmonologists dealing with asthma cases was 30% of total allergists and pulmonologists in Kuwait [5], along with a 95% confidence interval and a precision limit of 5%. Therefore, the minimum sample size was calculated to be 20 participants.
The survey was divided into two sections. The first one covered employment-related information. The second section evaluated the sixteen consensus statements that derived from the GINA 2022 guidelines [4], which covered four main themes; familiarity with GINA 2022 guidelines, diagnosis confirmation, management optimization, and recommended follow-up and maintenance. The questionnaire offered respondents a 3-point scale to rate their agreement with each statement, ranging from “Disagree” to “Agree” responses to the consensus statements were calculated and further analyzed; the widely accepted threshold for consensus is 75% based on percent agreement. Consensus was defined as high if ≥ 75%, and very high if ≥ 90% of respondents agreed with a statement [3, 6].
The statistical analysis was performed by Minitab 17.1.0.0 for Windows (Minitab Inc., 2013, Pennsylvania, USA). The normality of data was examined using the Shapiro-Wilk test. Categorical data were presented as numbers and percentages (%), and continuous data as mean and standard deviation.
Twenty-six medical professionals participated in the study, with an average age of 42 years and a standard deviation of approximately 5 years. The inter-quartile range (IQR) spanned from 35 years to 48 years, and the gender distribution was equal among the participants. All of them had at least a master’s degree in pulmonary medicine or allergy and immunology. The minimum years of experience of all participants was 8 years in dealing with cases of bronchial asthma.
More than 80% of participant agreed that changes in GINA 2022 guidelines were practical with their asthmatic patients (88.5%) (Table 1 and Figure 1), and they were familiar with it (84.6%), which represents a higher degree of consensus [Aspect 1 (86.6%), as shown in Figure 2].
Responses to the consensus statements
| Consensus statements | Total participants (n = 26) | ||
|---|---|---|---|
| Disagree | Neutral | Agree | |
| GINA 2022 guidelines consensus statements | |||
| 1. The GINA 2022 guidelines are practical in the patient population that I cover | 0 (0%) | 0 (0%) | 23 (88.5%) |
| 2. I am familiar with the changes in the GINA 2022 guidelines | 0 (0%) | 1 (3.8%) | 22 (84.6%) |
| Confirmation of diagnosis and identifying risk factors | |||
| 3. At a global level, spirometry before and after bronchodilator is the most useful initial investigation (GINA 2022) | 1 (3.8%) | 1 (3.8%) | 21 (80.8%) |
| 4. Confirmation of asthma diagnosis with lung function testing, before commencing long-term treatment, is common practice | 4 (15.4%) | 4 (15.4%) | 15 (57.7%) |
| 5. Treatment of modifiable risk factors in every asthmatic patient is highly recommended and practiced | 1 (3.8%) | 0 (0%) | 22 (84.6%) |
| 6. Patients with apparently mild asthma are still at risk of serious adverse events [7, 8] | 0 (0%) | 3 (11.5%) | 20 (76.9%) |
| Management | |||
| 7. The recommended first-line rescue inhaler, for the majority of patients is a short-acting β2 agonist (SABA) inhaler, e.g., Albuterol | 8 (30.8%) | 6 (23.1%) | 10 (38.5%) |
| 8. Low-dose inhaled corticosteroid (ICS)-formoterol as the reliever, is the preferred strategy because of the evidence that using ICS-formoterol as a reliever reduces the risk of exacerbations compared with using a SABA reliever, e.g., Albuterol | 0 (0%) | 3 (11.5%) | 20 (76.9%) |
| 9. Compared with as needed SABA, the use of ICS-formoterol reduced the risk of severe exacerbations by 60–64% [SYmbicort Given as needed in Mild Asthma (SYGMA) 1, novel Inhaled Steroid Treatment as Regular Therapy in Early Asthma (START)] | 2 (7.7%) | 3 (11.5%) | 18 (69.2%) |
| 10. SABA, e.g., Albuterol inhaler, as the reliever, is the non-preferred strategy; it is less effective than track 1 (the reliever is as needed low-dose ICS-formoterol) for reducing severe exacerbations | 2 (7.7%) | 5 (19.2%) | 16 (61.5%) |
| 11. Regular use of SABA, even for 1–2 weeks, is associated with increased airway hyperresponsiveness (AHR), reduced bronchodilator effect, increased allergic response, and increased eosinophils [9, 10] | 9 (34.6%) | 1 (3.8%) | 13 (50%) |
| 12. Track 2 (SABA is the reliever medication) involves using as needed SABA as a reliever, and taking the ICS whenever SABA is taken | 6 (23.1%) | 3 (11.5%) | 14 (53.8%) |
| 13. Patients with exacerbations should receive at least a medium dose of ICS-long-acting β2 agonist (LABA) before considering an add-on long-acting muscarinic antagonist (LAMA) | 1 (3.8%) | 2 (7.7%) | 20 (76.9%) |
| 14. LAMAs, e.g., Spiriva, should not be used as monotherapy for asthma (i.e. without ICS) because of the increased risk of severe exacerbations [11] | 2 (7.7%) | 0 (0%) | 21 (80.8%) |
| Maintenance | |||
| 15. Checking the inhaler technique in every patient is highly recommended and practiced at every visit | 0 (0%) | 4 (15.4%) | 19 (73.1%) |
| 16. Every patient with suspected severe asthma should be seen within 12 weeks of referral to an appropriate specialist severe asthma service | 2 (7.7%) | 2 (7.7%) | 19 (73.1%) |
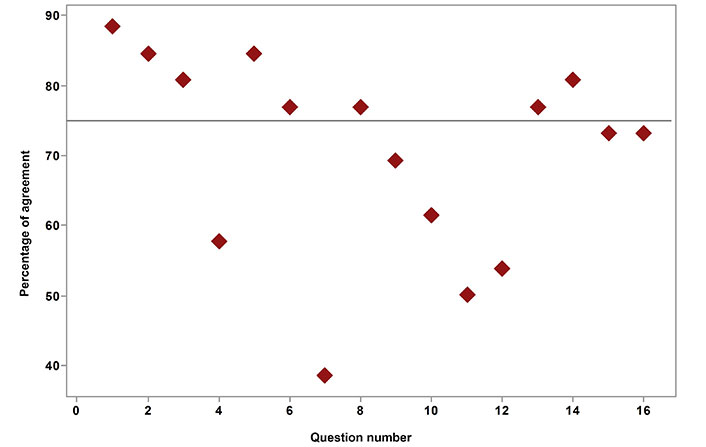
Frequency of agreement toward GINA 2022 consensus statements. The transverse line represented the threshold for consensus; consensus was defined as high if ≥ 75%, and very high if ≥ 90% of respondents agreed with a statement
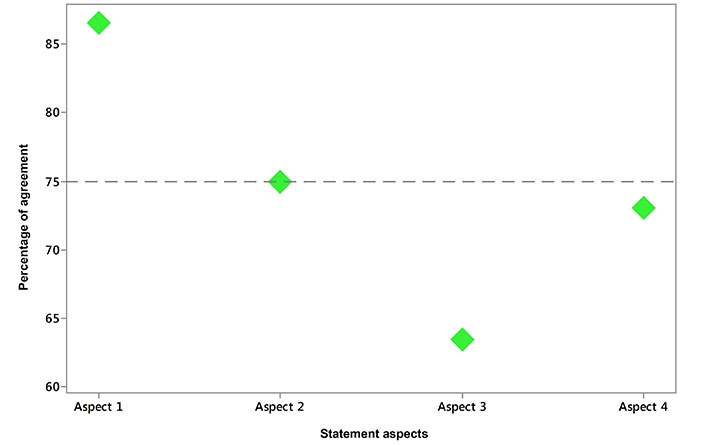
Percentage of agreement toward statement aspects. Aspect 1: familiarity with GINA 2022 guidelines; Aspect 2: diagnosis confirmation; Aspect 3: management optimization; Aspect 4: recommended follow-up and maintenance. The transverse line represented the threshold for consensus; consensus was defined as high if ≥ 75%, and very high if ≥ 90% of respondents agreed with a statement
The participants had a high level of agreement (80.8%) regarding spirometry before and after bronchodilators for diagnosing asthma. However, only 57.7% of them considered requesting lung function tests before starting long-term treatment to be a practical investigation. Four out of 26 participants (15.4%) were neutral towards this statement (Table 1).
The participants showed a high level of agreement on the importance of treating modified risk factors (84.6%) and taking into account the symptoms of patients with mild asthma, which can become severe (76.9%). Overall, the consensus level for diagnosis was still high, with more than 75% agreement (Aspect 2 in Figure 2).
The majority of participants did not fully agree with the optimal management statement of GINA 2022 guidelines, with only 63.5% expressing their support (Aspect 3 in Figure 2).
Only 38.5% agreed with using a SABA inhaler as a rescue medication, while 76.9% favored using low-dose ICS and LABA as a reliever. Additionally, 69.2% preferred the ICS-formoterol regimen over using SABA as needed, noting that it reduces the risk of severe exacerbations by 60–64%. Furthermore, 61.5% believed using SABA as a reliever was not a priority. Half of the participants acknowledged that regular SABA use, even for 1–2 weeks, could lead to increased AHR, reduced bronchodilator effect, increased allergic response, and increased eosinophils. Most participants (53.8%) chose track 2 as their preferred option.
In exacerbations, the agreement was higher (76.9%) among participants for receiving at least a medium dose of ICS-LABA before considering add-on LAMA. Additionally, 80.8% agreed that LAMA should not be used as a monotherapy for asthma (i.e. without ICS), as it could increase the risk of severe exacerbations (Table 1 and Figure 1).
Regarding checking inhaler technique in every patient at every visit and those with suspected severe asthma should be seen within 12 weeks of referral to an appropriate specialist severe asthma service; even though 73.1% of the participants agreed with those two recommendations, this percentage of consensus did not reach the threshold value of higher agreement as with Delphi method (75%) (Aspect 4 in Figure 2).
The GINA guidelines were updated in 2022 to suggest different methods to diagnose asthma in patients already taking controller medication. Spirometry tests before and after, using a bronchodilator are recommended for an accurate diagnosis [12]. Peak expiratory flow (PEF) meter can be used as an alternative method to confirm the diagnosis over two weeks. However, it is standard practice to confirm the diagnosis of asthma through lung function testing before starting long-term treatment [4]. In this study, only 57.7% of participants requested lung function tests before starting long-term treatment, which falls below the consensus threshold of 75%. That could be an important factor that precipitates misdiagnosis of asthma in Kuwait, however, as mentioned by Kavanagh et al. [13], in primary care, it is often difficult to find objective tests for diagnosing asthma. This fact often leads to misdiagnosis, which can either result in unnecessary treatment or delayed alternative diagnoses. However, if asthma is not diagnosed in time, it can lead to daily symptoms and serious exacerbations. So far, to reduce misdiagnosis and improve patient outcomes, it is crucial to have standardized diagnostic approaches, including objective measurements taken before treatment [13].
The GINA 2022 guidelines recommend assessing inhaler use, lung function, and managing comorbidities to improve asthma control. Comorbid conditions like obesity, chronic rhinosinusitis, sleep apnea, gastroesophageal reflux disease (GERD), and mental health issues can worsen symptoms [4]. Addressing these factors is vital for better outcomes. In this study, there was a strong agreement among healthcare providers (84.6%) on treating modifiable risk factors, with 76.9% recognizing the risk of mild symptoms progressing to severe asthma. Thus, it reflects how much allergists and pulmonologists in Kuwait were aware of the importance of addressing modified risk factors of asthma and its value in optimizing asthma management, improving patient outcomes, and reducing the burden of the disease on individuals and healthcare systems.
The GINA 2022 strategy report advises against using the term “mild asthma” in clinical practice due to the risk of patients assuming they do not need controller treatment [4]. If used, healthcare providers must ensure patients understand the persistent risk of severe attacks despite mild symptoms. Communicating that using treatment options containing ICS, particularly those with formoterol as relievers, significantly reduces this risk is required. Studies show that a significant percentage of adults with acute asthma, near-fatal asthma, and asthma-related deaths experienced symptoms less than once a week, underscoring the importance of proactive management and adherence to appropriate treatments, as even mild asthma can lead to life-threatening complications [7, 8].
Additionally, the GINA 2022 guidelines suggested that SABA as a reliever could serve as an alternative strategy for a first-line rescue inhaler [4]. However, only 38.5% of respondents agree with this statement, indicating a discrepancy with the latest GINA guidelines. The inclusion of this statement in the current questionnaire aimed to gauge familiarity with recent changes. It is crucial to consider whether physicians believe that more patients are still using SABA inhalers as relievers in current practice or if their providers have transitioned them to a different option.
According to the current survey, 76.9% of participants favored using low-dose ICS-formoterol as a reliever for asthma management. Studies show that it reduces exacerbation risk by 60–64% compared to SABA relievers like Ventolin [14]. Combo inhalers also decrease exacerbation risk [15]. Since 2019, GINA guidelines have emphasized treating all asthma patients with ICS-containing medications and discontinuing SABA use alone due to severe exacerbation risks. Using SABA as a reliever is not preferred over track 1, which involves ICS-formoterol use. Familiarity with track 2 (ICS with SABA as needed) was lower [4]. Regular SABA use, even briefly, can increase AHR, reduce bronchodilator effects, and worsen allergic responses [9, 10, 16].
GINA advises against using SABAs without ICS due to severe exacerbation risks, lack of anti-inflammatory properties, and potentially worsened eosinophilia [4]. Instead, GINA recommends budesonide/formoterol as a reliever [17–19]. Low-dose ICS-formoterol reduces severe attack risks, hospital visits, and systemic corticosteroid needs [20, 21]. ALPACA study findings support avoiding LAMA monotherapy in asthma; combining LAMA with ICS-LABA does not improve symptoms [11]. Triple therapy is not superior to ICS-LABA for moderate to severe asthma dyspnea [22]. LAMA monotherapy increases severe exacerbation risks, while initial ICS use with or without bronchodilators optimizes safety and symptom assessment [22], as 80.8% of the participants agreed. Checking the inhaler technique during every visit is highly recommended and practiced by 73.1% of the participants, as proper technique is crucial for effective asthma treatment and improved outcomes [23].
Optimizing the inhaler technique is vital for effective asthma management [24]. However, healthcare providers encounter barriers such as limited time, insufficient resources, and a need for educators [25]. To overcome these challenges, providers can refer patients to professionals who provide brief training or online resources [26]. Checking inhaler techniques during patient encounters can also help identify errors [24]. Improving inhaler techniques can lead to better asthma management [26]. Additionally, 73.1% of our participants recommend that patients with suspected uncontrolled asthma see an appropriate specialist within 12 weeks.
The questionnaire utilized in this study had numerous strengths. Firstly, it was developed with the input of asthma experts who provided their insights and perspectives. This data ensured that the survey captured valuable information from professionals with extensive knowledge and experience in asthma management. Secondly, the questionnaire considered the latest updates and changes in the GINA 2022 guidelines, providing valuable insights into implementing these updates. These strengths helped provide a comprehensive and informed assessment of healthcare providers’ perspectives on asthma management.
Even though, the study has certain limitations that should be acknowledged. Firstly, employing a single round of modified Delphi methods, which was different from the traditional Delphi technique, even though it can still provide valuable insights, particularly in exploratory phases of research or when used as part of a larger mixed-methods approach. The second limitation was the selection of respondents, which may have introduced bias, as those most familiar with the GINA guidelines were likely included, potentially excluding primary care physicians with different perspectives. The third limitation, the total number of responses was small, and not all questions were answered, which could impact the generalizability of the findings. Finally, the absence of patient perspectives is a limitation, as their viewpoints may differ significantly from those of specialist physicians, and including their opinions could have provided a more comprehensive understanding of asthma management. These limitations underscore the need for future research to address these gaps and obtain a broader range of perspectives to enhance the findings’ validity and applicability.
Based on the updated GINA guidelines, this study assessed physician consensus on critical statements related to asthma management. The high consensus among respondents demonstrated a clear understanding of the guidelines. Objective lung function testing, comorbid conditions, and early use of ICS were emphasized. Some physicians still favored SABA inhalers, but there was agreement on the effectiveness of low-dose ICS-formoterol. LAMA monotherapy was not recommended, and checking inhaler technique and follow-up were highlighted. Limitations include single round modified Delphi survey, respondent bias, a small sample size, and the absence of patient perspectives. These findings highlight the perspective view of allergists and pulmonologists who deal with asthma cases in everyday practice, which could influence how asthma management is optimized.
AHR: airway hyperresponsiveness
GINA: Global Initiative for Asthma
ICS: inhaled corticosteroid
LABA: long-acting β2 agonist
LAMA: long-acting muscarinic antagonist
SABA: short-acting β2 agonist
YO, MAA, and AA equally contributed to: Investigation, Data curation, Formal analysis, Writing—original draft, Writing—review & editing. All authors read and approved the final manuscript.
The authors declare that they have no conflicts of interest.
The study was approved by the Ethics Committee of Kuwait University and the Ministry of Health (1239/2023) and complied with the Declaration of Helsinki.
Informed consent to participate in the study was obtained from all participants.
Not applicable.
The raw data could be available from the corresponding author upon reasonable request.
Not applicable.
© The Author(s) 2024.
Copyright: © The Author(s) 2024. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Riyad Allehebi, Hamdan AL-Jahdali
Maria Michelle Papamichael, Charis Katsardis
Yuto Hamada ... Peter Gerard Gibson
Andrea Giovanni Ledda ... Stefano Del Giacco
Teresa Garriga-Baraut ... Margarita Tomás-Pérez
