Affiliation:
1Neurological Surgery, Hamad Medical Corporation, Doha, Qatar
Email: dr.alimsheik@gmail.com
ORCID: https://orcid.org/0000-0002-4033-1985
Affiliation:
3Bioethics, Lebanese University, Beirut, Lebanon
ORCID: https://orcid.org/0009-0004-7355-9486
Explor Neurosci. 2025;4:100689 DOI: https://doi.org/10.37349/en.2025.100689
Received: February 05, 2025 Accepted: April 29, 2025 Published: May 20, 2025
Academic Editor: Jussi Sipilä, University of Eastern Finland, Finland
The choroid plexus, pivotal for cerebrospinal fluid (CSF) regulation and blood-CSF barrier function, becomes a focal point for primary central nervous system lymphoma (PCNSL). This article delves into a case of this uncommon presentation, highlighting diagnostic challenges, treatment complexities, and post-treatment outcomes. A 30-year-old Lebanese patient with mild headaches and vomiting was initially diagnosed with vasculitis but later confirmed through endoscopic biopsy to have diffuse large B-cell lymphoma of the choroid plexus. Treatment with intravenous methotrexate, intrathecal cytarabine, rituximab, and radiotherapy led to gradual neurological improvement. Treatment strategies, aligned with PCNSL standards, include intravenous methotrexate, intrathecal cytarabine, rituximab, and radiotherapy, leading to gradual neurological improvement post-treatment. Prognostic factors, such as age and specific brain area involvement, guide tailored treatment plans. This report emphasizes the need for a multidisciplinary approach, increased awareness, and ongoing research for optimal outcomes in PCNSL cases involving the choroid plexus.
The choroid plexus is an intricate system of capillaries surrounded by specialized cells and performs multiple functions. Its key role involves the generation of cerebrospinal fluid (CSF) through the specialized ependymal cells that coat the brain’s ventricles. Additionally, the choroid plexus acts as a barrier within the brain, segregating blood from CSF, commonly referred to as the blood-CSF barrier [1]. Lymphomas are a category of cancers originating in the lymphatic system, where abnormal white blood cells proliferate in various lymph glands throughout the body [2]. Ranking as the sixth most prevalent cancer type, excluding non-melanoma skin cancer, lymphomas encompass diverse subtypes, among them central nervous system lymphoma (CNSL). Isolated lymphoma represents one of these subtypes [2, 3]. Primary CNSL (PCNSL) is a non-Hodgkin lymphoma that occurs outside the lymph nodes and is limited to the neural axis. It constitutes approximately 3–4% of all primitive brain neoplasms, primarily manifesting in deep supratentorial regions [3]. While ventricular involvement is relatively common, it usually stems from extension from a subependymal location. In the infrequently reported instances of primary ventricular forms, an origin from the choroid plexus is exceedingly rare, with only three cases documented in English literature to date [4].
While the precise origins of CNSL remain uncertain, certain factors may elevate the likelihood of developing the condition. These include having a compromised immune system due to conditions like acquired immunodeficiency syndrome (AIDS), other immune system disorders, or chronic immunosuppression resulting from organ transplantation [5]. Isolated CNSLs present with a distinctive set of symptoms, including headaches that intensify when lying flat, blurred vision, cognitive decline, disequilibrium, hearing difficulty, and a combination of confusion and weakness, potentially accompanied by nausea and vomiting. These specific neurological manifestations signify a unique clinical profile associated with isolated CNSLs, prompting careful medical evaluation to ascertain an accurate diagnosis and appropriate management [4, 5]. This article delves into a case of this uncommon presentation, highlighting diagnostic challenges, treatment complexities, and post-treatment outcomes.
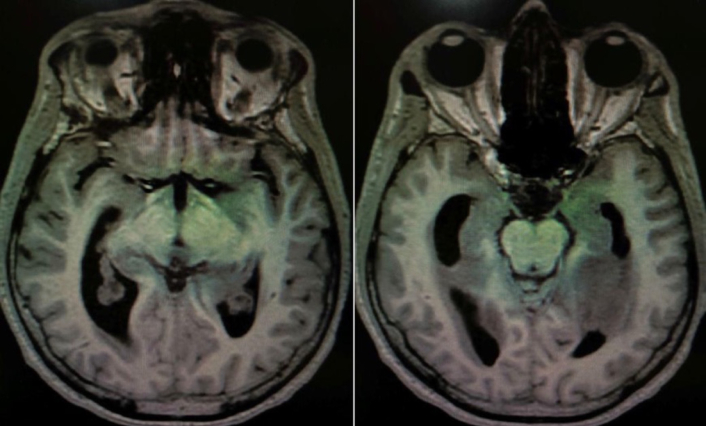
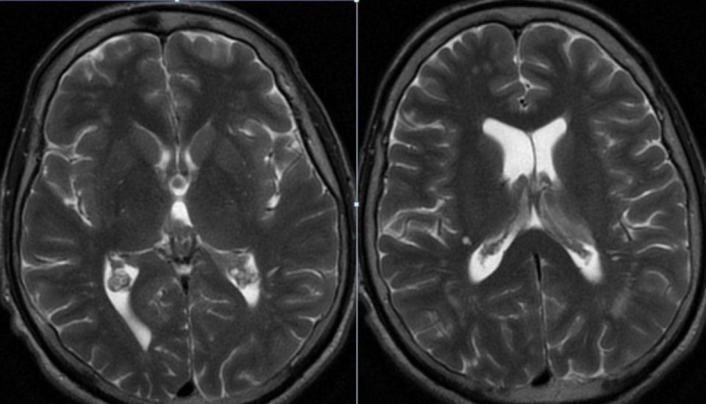
A 30-year-old male Lebanese patient was received at the emergency department initially manifesting mild headache and emesis over the weekend in the inaugural week of March 2023. Preliminary laboratory analyses yielded normative outcomes. A cranial computed tomography (CT) exhibited regular findings except for marginal engorgement of the choroid plexus within the lateral ventricles (Figure 1). Despite the absence of neurologic deficits, subsequent magnetic resonance imaging (MRI) disclosed a comparable indefinite irregularity of the choroid plexus (Figures 2 and 3). CSF examination demonstrated standard parameters for glucose, protein, white blood cells, and red blood cells. Additional inquiries, encompassing echocardiography and carotid imaging, yielded unremarkable results. The patient lacked notable medical history but exhibited elevated cholesterol levels and was on a regimen of aspirin 81 mg, clopidogrel 75 mg, and atorvastatin 40 mg. Following discharge with analgesic therapy, the family reported alleviation of the headache. However, a few days later, the patient revisited the emergency department with exacerbated cognitive impairment, confusion, and lethargy. A second urgent MRI unveiled heightened choroid plexus congestion and hypodense lesions in the pons (Figures 4 and 5). Lumbar puncture (LP) indicated elevated white blood cells, elevated glucose, and diminished protein levels, culminating in a vasculitis diagnosis. Steroid therapy, namely methylprednisolone 500 mg every 12 h, was initiated. Concomitantly, further deterioration of the neurological status of the patient ensued despite steroid therapy, leading to choroid plexus edema and hydrocephalus, necessitating ventriculoperitoneal shunt (VPS) placement. The patient’s condition deteriorated further, with a Glasgow Coma Scale score of 10, Karnofsky’s performance status at 10–20%, and Zubrod stage 4. An urgently conducted choroid plexus biopsy during the same procedure revealed evidence of diffuse large B-cell lymphoma (DLBCL). Postoperative complications in the intensive care unit necessitated a second VPS due to hydrocephalus and obstruction of the initial catheter by proliferating choroid plexus tissue (Figure 6). Despite diminished reflexes and increased oxygen requirements, the patient remained responsive to pain. DLBCL treatment involved intravenous methotrexate, intrathecal cytarabine, and rituximab, followed by 18 radiotherapy sessions. Post-chemotherapy, the patient exhibited confusion, short-term memory deficits, and orientation primarily toward immediate family members. However, a gradual improvement in neurological status was noted during the radiotherapy course. As of August 2023, the patient has completed the requisite radiotherapy sessions. During the last assessment in December 2024, the individual was conscious, cooperative, and oriented. Lingering minor lower limb weakness is progressively improving through physiotherapy. On the Karnofsky scale, the patient registers at 60%, corresponding to Zubrod stage 2.
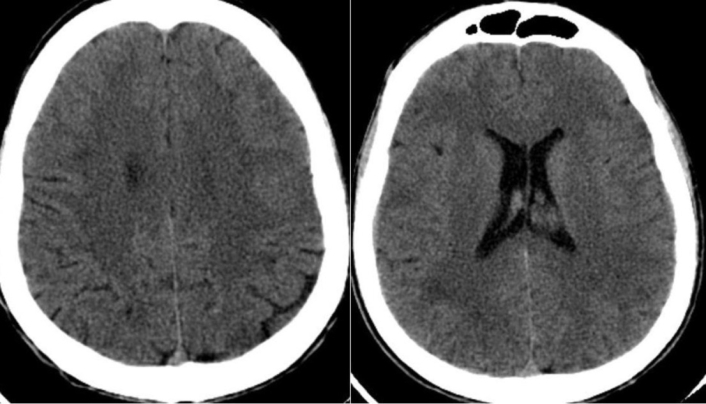
First computed tomography (CT) in the axial view showing an isodense congestion of the choroid plexus: left lateral ventricle
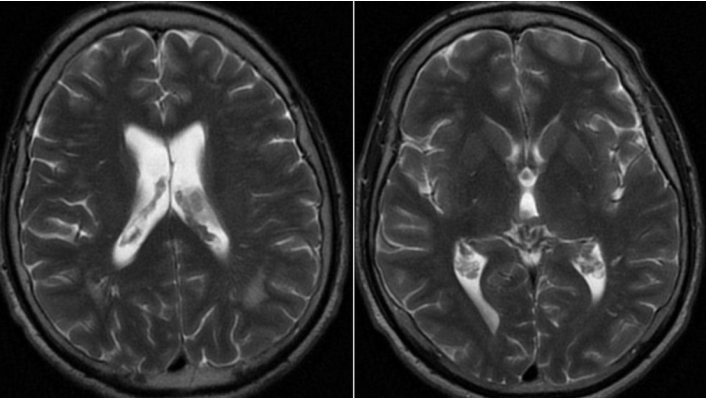
Magnetic resonance imaging (MRI) of the head in axial view: T2-weighted sequence showing an isointense congestion of the choroid plexus
Computed tomography (CT) in the axial view showing a hypodense congestion of the choroid plexus and invasion into the subependymal tissue of the left lateral ventricle
Magnetic resonance imaging (MRI) of the head in axial view: T2-weighted sequence showing an increased isointense congestion of the choroid plexus: bilateral lateral ventricles
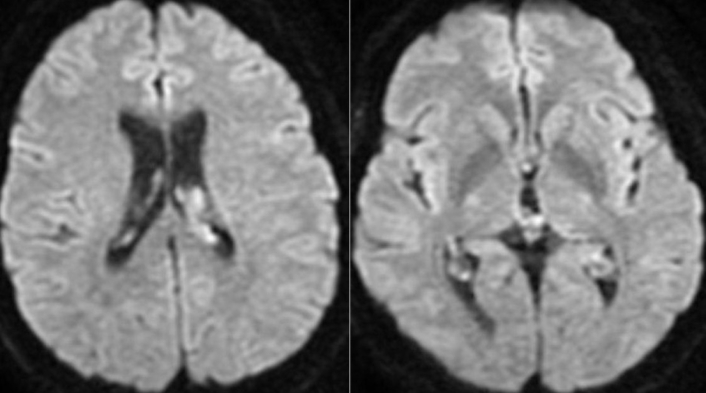
Diffuse-weighted magnetic resonance imaging (MRI) in the axial view showing a high signal in the choroid plexus of the lateral ventricles
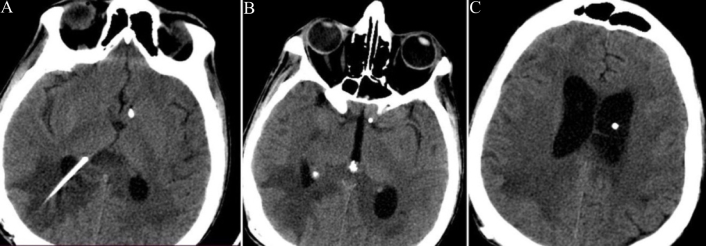
Computed tomography (CT) in the axial view showing a hypodense congestion of the choroid plexus and invasion and hypodensity in the subependymal tissue of the left lateral ventricle. Note the ventricular catheter of the ventriculoperitoneal shunt (VPS) in the figures 6A, 6B, and 6C showing its trajectory
The diagnosis of isolated CNSLs involves a multi-modal approach [6]. A CT scan typically reveals hyperdense foci, while MRI often shows enhancing choroid plexus lesions extending from the lateral ventricles to the temporal horns. LP may exhibit non-specific changes indicative of CNS involvement [6]. However, the definitive confirmation is usually achieved through an endoscopic biopsy of the choroidal lesion. This comprehensive diagnostic process helps accurately identify isolated CNSLs and guides healthcare professionals in formulating appropriate treatment strategies based on the confirmed pathology.
Patients diagnosed with the choroid plexus subtype of PCNSLs have several treatment options available [7]. These include radiation therapy, chemotherapy including intravenous methotrexate and intrathecal cytarabine, steroid therapy, targeted therapy, high-dose chemotherapy with stem cell transplant, and immunotherapy. As medical research advances, new treatment modalities are continuously being explored in clinical trials. It’s important to note that these treatments may bring about side effects, and patients are encouraged to consider participation in clinical trials, which can be undertaken before, during, or after initiating standard cancer treatments. Regular follow-up tests are typically recommended to monitor the patient’s response to treatment and adjust the therapeutic approach as necessary for optimal outcomes [7]. The prognosis for the choroid plexus subtype of CNSLs is influenced by various factors, with certain indicators suggesting a poorer outlook [8]. Patients aged older than 60 years tend to have a less favorable prognosis. Additionally, elevated levels of serum lactate dehydrogenase and an increased concentration of CSF protein are associated with poorer outcomes. The involvement of non-hemispheric areas of the brain, such as the periventricular, basal ganglia, brainstem, and cerebellum, is considered a negative prognostic factor [9]. Furthermore, the presence of intraocular disease along with concurrent brain involvement contributes to an unfavorable prognosis. Recognizing these poor prognostic factors is crucial for healthcare professionals in tailoring treatment plans and providing patients with comprehensive and informed care [9].
The presented case of PCNSLs originating from the choroid plexus is noteworthy due to its rarity and the complex clinical course observed in the patient. This case contributes valuable insights into the diagnostic challenges, treatment modalities, and post-treatment outcomes associated with the choroid plexus subtype of PCNSL [1–3]. The diagnostic journey in this case underscores the multifaceted nature of PCNSL diagnosis. Initial presentations of mild cephalalgia and emesis, coupled with normal laboratory results, posed a challenge in identifying the underlying pathology. The initial cranial CT revealed marginal engorgement of the choroid plexus, prompting further investigation [4, 7, 8]. Subsequent MRI played crucial roles in narrowing down the differential diagnosis, culminating in the identification of DLBCL through a choroid plexus biopsy [10]. This emphasizes the significance of a multi-modal diagnostic approach in cases where CNSLs, particularly those involving the choroid plexus, may present with atypical symptoms. The treatment strategy implemented in this case reflects the complexity of managing PCNSL with choroid plexus involvement. The initiation of steroid therapy, a common approach in CNSLs, led to unexpected adverse effects, including choroid plexus edema and hydrocephalus, necessitating VPS placement [11]. The challenges in managing complications underscore the need for a careful balance in therapeutic interventions, considering the delicate nature of the CNS structures involved. The utilization of intrathecal methotrexate, rituximab, and radiotherapy in the treatment regimen aligns with current standards for PCNSL [7–9]. The post-treatment outcomes, while showing a gradual improvement in neurological function, also highlight the persistence of complications, including confusion and short-term memory deficits. These findings underscore the importance of long-term follow-up and rehabilitation strategies to optimize the patient’s overall quality of life.
Prognostic factors, as discussed in the Introduction, play a crucial role in guiding treatment decisions and predicting outcomes. In this case, factors such as the patient’s age, serum lactate dehydrogenase levels, and the involvement of non-hemispheric brain areas were associated with a poorer prognosis. The recognition of these factors during the disease is pivotal for tailoring treatment plans and providing comprehensive and informed care.
This case report contributes to the existing body of literature by providing a detailed account of a rare presentation of PCNSL originating from the choroid plexus. The complexities in diagnosis, treatment, and post-treatment outcomes underscore the importance of a multidisciplinary approach involving neurology, oncology, and neurosurgery. Additionally, it emphasizes the ongoing need for research to enhance our understanding of this rare subtype and explore novel treatment modalities for improved patient outcomes.
CNSL: central nervous system lymphoma
CSF: cerebrospinal fluid
CT: computed tomography
DLBCL: diffuse large B-cell lymphoma
MRI: magnetic resonance imaging
PCNSL: primary central nervous system lymphoma
VPS: ventriculoperitoneal shunt
A Msheik: Conceptualization, Methodology, Investigation, Formal analysis, Writing—original draft, Supervision, Project administration. ZAM: Validation, Writing—review & editing, Resources, Supervision. A Mawassi: Data curation, Software, Visualization, Writing—review & editing.
The authors declare that they have no conflicts of interest.
This case report complies with the ethical principles outlined in the Declaration of Helsinki. Ethical approval was obtained from the Institutional Research Board (IRB) at Al Zahraa Hospital University Medical Center (ZHUMC).
Written informed consent was obtained from the patient before inclusion in this case report.
Written informed consent for publication was obtained from the patient, ensuring that all identifying information has been anonymized to maintain confidentiality.
The raw data supporting the conclusions of this manuscript will be made available by the authors, without undue reservation, to any qualified researcher.
Not applicable.
© The Author(s) 2025.
Open Exploration maintains a neutral stance on jurisdictional claims in published institutional affiliations and maps. All opinions expressed in this article are the personal views of the author(s) and do not represent the stance of the editorial team or the publisher.
Copyright: © The Author(s) 2025. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 1597
Download: 15
Times Cited: 0
