Affiliation:
1Département de Microbiologie Infectiologie et d’Immunologie, Faculté de Médecine, Université Laval, Québec City QC G1V 0A6, Canada
2Département de Bioénergie, Collège Supérieur de Naturopathie du Québec, Montréal QC J5A 0E9, Canada
Email: herveagonsanou@yahoo.fr
Affiliation:
3Department of Environmental History and History of Sciences, University of Minas Gerais, Belo Horizonte 31270-901, Brazil
Affiliation:
2Département de Bioénergie, Collège Supérieur de Naturopathie du Québec, Montréal QC J5A 0E9, Canada
Explor Med. 2023;4:1168–1188 DOI: https://doi.org/10.37349/emed.2023.00201
Received: March 17, 2023 Accepted: June 16, 2023 Published: December 29, 2023
Academic Editor: Gennaro Daniele, Istituto di Ricovero e Cura a Carattere Scientifico, Italy
According to recent data reported, it is noted that lung cancer is the leading cause of cancer death internationally followed by cardiovascular diseases and diabetes. This disease is observed in both women and men and is related to lifestyle habits. Several causes are reported to be at the origin of lung cancer, especially smoking. It is important to note that the majority of lung cancers develop in the bronchi, that is to say at the level of the upper airways which lead to the lungs, which does not however make it possible to rule out the risk factors that come under environmental pollution since man breathes the air quality of the environment every day for his breathing. This review of the literature has made it possible to draw up a state of knowledge in order to understand the risk factors that increase lung cancer. More specifically, this work will make it possible to raise awareness in the field of the fight against cancer, in particular lung cancer.
Lung cancer causes more cancer deaths worldwide [1]. Cancer is a public health problem and one of the main causes of death in all countries of the world. In 2020, lung cancer remained the leading cause of cancer death with approximately 1.8 million deaths (18% of all cancer deaths), according to data reported by “Global Cancer Statistics 2020”. and the International Agency for Research on Cancer (IARC) [2]. The incidence and mortality related to this disease are presented in Figures 1 and 2 by a GLOBOCAN study report.
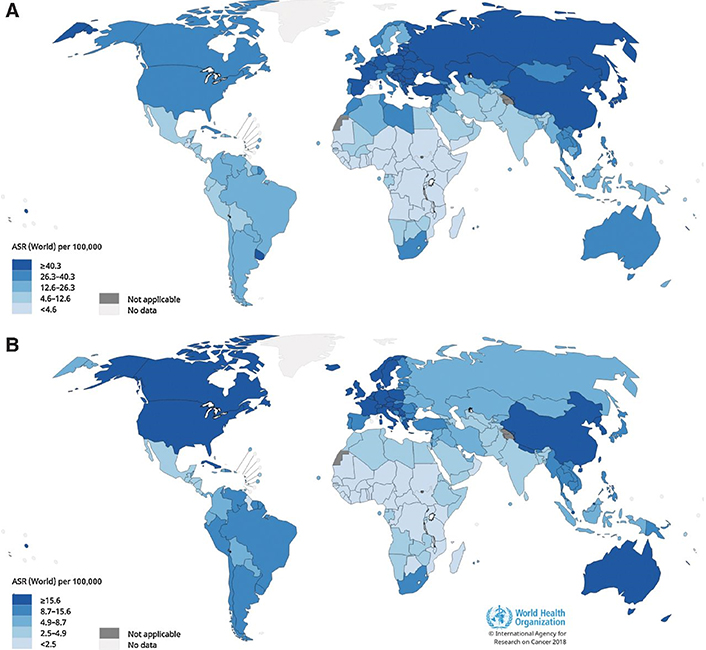
The incidence of lung cancer worldwide. (A) The age-standardized incidence rates of lung cancer in males using data from GLOBOCAN 2018. An increase in the incidence rate associated with lung cancer is seen in Micronesia, Polynesia, Central and Eastern Europe and East Asia and lowest in most of Africa; (B) the results published by GLOBOCAN 2018 on the age-standardized incidence rate of lung cancer in women. It is noted that the incidence of lung cancer in women is highest in North America, Northern Europe, Western Europe and Australia/New Zealand and lowest in most of Africa. ASR: age-standardized rate [3]
Note. Reprinted with permission from “Cancer Today” by IARC; c2018 (https://gco.iarc.fr/today/home). © IARC.
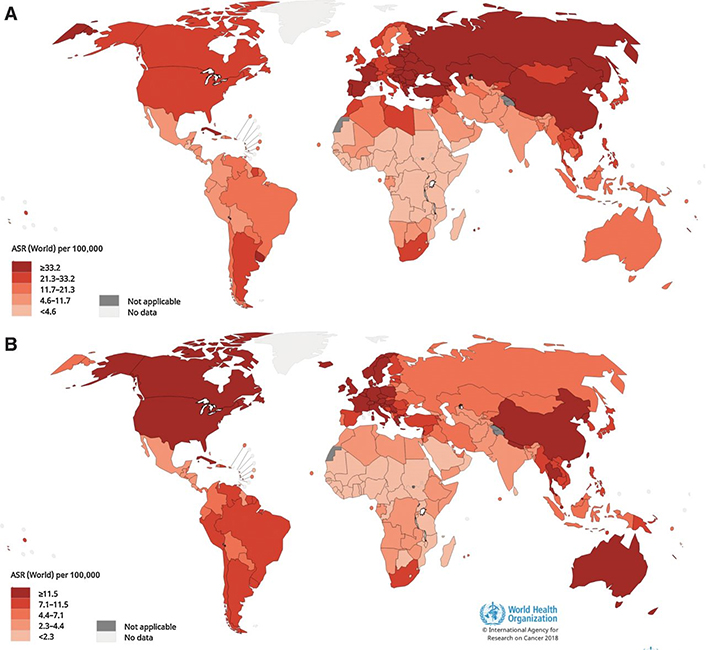
Estimated ASRs for lung cancer mortality worldwide using published data from the work of GLOBOCAN, 2018. (A) Cancer mortality rate age-standardized lung function in men. It is noted that this male lung cancer mortality rate is highest in Eastern Europe, Western Asia, Northern Africa and some East Asian countries and highest. low in most of Africa; (B) the age-standardized lung cancer mortality rates among females. Lung cancer mortality among women is found to be highest in North America, Northern Europe, Western Europe and Australia/New Zealand and lowest in most of Africa [3]
Note. Reprinted with permission from “Cancer Today” by IARC; c2018 (https://gco.iarc.fr/today/home). © IARC.
Research carried out in 2020 shows that lung cancer remains the leading cause of cancer death with approximately 1.8 million deaths (18%), followed by colorectal cancer (9.4%), liver (8.3%), stomach (7.7%), and breast in women (6.9%). Lung cancer is a preventable cancer and therefore the mortality associated with this type of cancer can be reduced considerably if the causative factors are addressed. Indeed, it is noted that in nearly 9 cases out of 10 cancers can be prevented by stopping smoking2. It is important to note that smokers are 22 times more likely to develop lung cancer during their lifetime compared to non-smokers. Individuals who do not use tobacco but who are exposed to tobacco smoke (standing next to a smoker) or who are exposed to environmental fumes at home, at work, or in other public places also run an increased risk of developing lung diseases, including chronic respiratory disease and lung cancer [2].
Hence the importance of taking adequate preventive measures and combating environmental pollution. The benefits of quitting smoking are almost immediate. Indeed, after only 20 min, the heart rate decreases. Within 2 to 12 weeks, circulation improves and lung function increases. In 1 to 9 months, the cough and shortness of breath decrease. After 10 years of quitting smoking, the risk of lung cancer drops to about half that of a smoker the risk of lung cancer drops to about half that of a smoker [2]. Lung cancer is prevalent in many countries around the world (Figure 3).
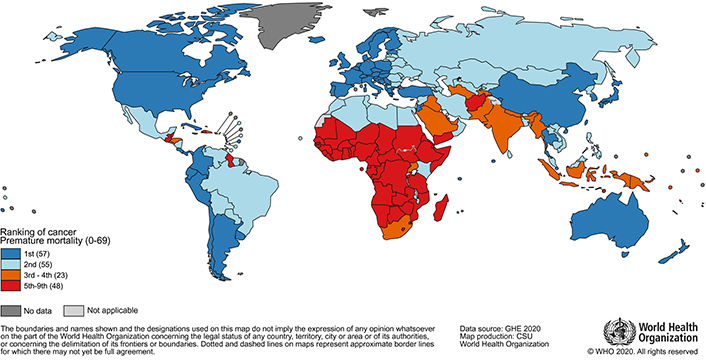
National ranking of cancer as a cause of death according to age < 70 years in 2019. Included in the legend is the number of countries represented in each group [4]
Note. Reprinted with permission from “Cancer Today” by IARC; c2020 (https://gco.iarc.fr/today/home). © IARC.
Many studies describe the factors in the development of lung cancer [5, 6].
Numerous studies have confirmed that smoking is the main cause of all major histological types of lung cancer. Studies of lung cancer since the early 1950s have demonstrated the carcinogenic effect of tobacco smoke on the lungs. This aspect has been taken into account by the authorities in public health recommendations for the well-being of the population since the 1960s [6]. Smoking duration should be considered the greatest risk factor for lung cancer in smokers [6]. Sometimes when a smoker quits smoking, the fact that he has already smoked for a certain amount of time complicates the explanation of the appearance of other pathologies in individuals [6–9]. But quitting smoking is very beneficial to prevent the appearance of lung cancer [6]. In some studies related to the identification of the causes of lung cancer, it has been reported that smoking is a powerful confounder as the latter has complicated several investigations carried out to clarify the role of smoking in the development of lung cancer [6–8]. Some epidemiological and biological studies demonstrate in non-smokers a link between exposure to cigarette smoke and the risk of lung cancer [6]. Smoking is known to cause 85% of lung cancer cases; however, in several population-based studies, only a fraction of long-term smokers develop lung cancer [10]. It has been confirmed that the development of lung cancer is related to the amount and duration of smoking in an individual, as well as to other causes of lung cancer. In the majority of cases, men and women who habitually smoke are respectively more likely to develop lung cancer than non-smokers [6–8, 10]. In addition, passive smoking or inhalation of second-hand smoke is associated with respiratory diseases and lung cancer in non-smokers. Many studies have reported that children who were exposed to passive smoking early may somehow be at high risk of developing lung cancer later in life [10]. It is also important to note that tobacco smoke contains polycyclic aromatic hydrocarbons (PAHs), which are known carcinogens that interact with and damage DNA, leading to lung cancer [6, 8–10]. This results in mutations at the DNA level, which trigger the appearance of lung cancer. It is found that these mutations are much more present and elevated in smokers than in non-smokers of the population [10]. This is why it is very important to develop prevention strategies to reduce the rate of cigarette consumption in the population and especially to raise awareness of this.
Studies have shown that the risk of developing lung cancer is increased in a family history of individuals who have had lung cancer [6, 10]. These studies reported a high and early familial risk of lung cancer [6, 10]. These lung cancer risks have been observed in these individuals even after a reduction in or cessation of smoking. The risk of lung cancer is also associated with a mutation of the p53 tumor suppressor gene [6, 10]. The family history, high-penetrance genes, and genetic polymorphisms are also factors in the occurrence of lung cancer [6]. Recent genome-wide association studies have identified several genetic polymorphisms that are involved in lung cancer [6]. These genes identified and implicated in lung cancer are listed in Table 1.
Genetic variants identified and implicated in lung cancer [6]
| Susceptibility loci | Tagging SNPs | Genes | References |
|---|---|---|---|
| 3q28 | rs4488809 | TP63 | [17–19] |
| 5p15.33 | rs402710 rs2736100 rs401681 | intron 1 of TERT CLPTM1L | [20–23] |
| 6p21.33 | rs4324798 rs3117582 | APOM, BAG6 | [20, 21, 24] |
| 8q21 | rs2741354 | [25] | |
| 9p21 | rs1333040 | CDKN2B-AS1 | [26] |
| 10q25.2 | rs7086803 | VTI1A | [27] |
| 12p13.33 | rs6489769 | RAD52 | [27] |
| 12q23.1 | rs12296850 | [28] | |
| 13q31.3 | rs2352028 | GPC5 | [29] |
| 15q25.1 | rs1051730 rs8034191 rs16969968 rs12914385 | CHRNA3, CHRNA5, and CHRNB4 | [20, 30, 31] |
| 17q24.3 | Rs7216064 | BPTF | [32] |
| 18p11.22 | rs11080466 rs11663246 | PIEZO2 | [33] |
| 22q12.2 | rs17728461 rs36600 | HORMAD2 LOC105372988 | [17] |
| SNP: single nucleotide polymorphism | |||
TP63: tumor protein 63; TERT: telomerase reverse transcriptase; CLPTM1L: cleft lip and palate transmembrane1-like; APOM: Apolipoprotein M; BAG6: Bcl-2-associated athanogen-6; CDKN2B-AS1: cyclin dependent kinase inhibitor 2B antisense RNA 1; VTI1A: Vps10p-tail-interactor-1a; RAD52: RAD52 homolog, DNA repair protein; GPC5: glypican-5; CHRNA3: cholinergic receptor nicotinic alpha 3 subunit; CHRNA5: cholinergic receptor nicotinic alpha 5 subunit; CHRNB4: cholinergic receptor nicotinic beta 4 subunit; BPTF: bromodomain PHD finger transcription factor; PIEZO2: piezo type mechanosensitive ion channel component 2; HORMAD2: hormonal regulators of muscle and metabolism in aging domain containing 2; LOC105372988: uncharacterized LOC105372988 [Homo sapiens (human)] gene type noncoding RNA. Blank space: not mentioned. References in the table refer to the ones in the original article [6] from which the table was reproduced
Note. Reprinted with permission from “Risk factors for lung cancer worldwide” by Malhotra J, Malvezzi M, Negri E, La Vecchia C, Boffetta P. Eur Respir J. 2016;48:889–902 (https://erj.ersjournals.com/content/48/3/889). © ERS 2016.
A case-control study of non-smokers shows that a diet rich in vegetables and fruit has some protective effect against lung cancer [6]. Meta-analysis studies have confirmed that the increased risk of lung cancer is seen in alcoholics who also smoke. Indeed, a combination of smoking and regular alcohol consumption has been shown to be a risk factor for lung cancer [6]. Also studies have pointed out that due to the strong correlation between alcohol consumption and smoking in many populations, it is therefore difficult to elucidate the impact of alcohol on lung carcinogenesis [6]. Many research studies have confirmed that alcohol consumption is strongly implicated in lung cancer. These include a pooled analysis of 7 prospective studies with 399,767 participants and 3,137 cases of lung cancer which showed that lung cancer was identified in those who consumed at least 30 g/day of alcohol than in those who did not [11].
The risk of developing lung cancer is associated with common exposures to ionizing radiation [6]. This risk factor for the development of lung cancer has been reported in survivors of the atomic bomb, as well as in patients treated with radiation therapy. It should also be noted that the increased risk of lung cancer due to exposure to ionizing radiation has been observed in miners who are exposed to radioactive radiation and its decay products in the course of their work [6].
Many environmental factors are involved in the development of lung cancer. Indeed, many case studies note that the indoor environment is heavily polluted by a complex mixture of gases and particles produced by combustion. Many studies conclude that solid exposure to fuel smoke has been associated with various diseases, including chronic obstructive pulmonary disease, acute respiratory infections, and various types of cancer, particularly lung cancer. It is important to point out that incomplete combustion leads to the emission of gases, including sulfur dioxide, carbon monoxide, carbon dioxide and nitrogen oxide, as well as PAHs, formaldehyde and metals heavy. It is therefore necessary to develop procedures to maintain the environment less polluted (healthy environment) to prevent environmental factors that can lead to lung cancer and especially to have better respiratory health [6, 10]. It should be noted that approximately half of the world’s population is at risk of developing certain serious respiratory diseases due to the current use of unprocessed biofuels and coal for cooking and heating [10]. Other cancer studies suggest that environmental factors have been implicated in the vast majority of human cancers, particularly lung cancer [6–10]. Factors like smoking, air pollution, exposure to cancer-causing chemicals, and alcohol consumption are environmental factors known to be linked to the development of cancer in humans, particularly lung cancer [6, 12]. It is also important to note that exposure to radon, heavy metals used in foundries and asbestos considerably increases the risk of developing lung cancer. Indeed, research also shows that exposure to radon, heavy metals used in foundries and asbestos significantly increases the risk of developing lung cancer without ignoring other health risks in humans [6, 12]. In Asia and in several regions of the world, indoor air pollution appears to be a major risk factor for lung cancer in non-smoking women [6]. A cohort study [6] carried out on the environment shows a slight increase in risk among people considered to be the most exposed to air pollution. Therefore, the IARC classifies outdoor air pollution as a lung carcinogen in humans [6].
Outdoor air pollution is also caused by other factors such as transportation, power generation, factories, industrial plants and agriculture, which increases the risk of respiratory and cardiovascular diseases not to mention lung cancer [10]. Pollution has been classified as a Group 1 human carcinogen by the IARC [10]. In air pollution, it should be noted that PAHs are among the main classes of carcinogens resulting from the incomplete combustion of wood or fuel as well as industrial emissions or vehicle exhaust gases. In recent years the means of transport (vehicles, motorcycles, etc.) have increased, which constitutes a major concern for the integrity of the environment. Studies by several research teams have shown that long-term exposure to PAHs increases the incidence of lung cancer [6–10]. Other valuable studies have provided insight that vehicle engine exhaust is a complex mixture of many carcinogenic and mutagenic chemicals implicated in lung tumorigenesis. Indeed, research conducted by Christiani [13] in 2021 leads to the conclusion that outdoor (ambient) air can contain a number of hazardous agents, and that the majority are generated by the combustion of fossil fuels, including carcinogens such as PAHs and metals such as chromium, arsenic and nickel. In the same previous studies by Christiani [13] in 2021, it is noted that depending on the sources of pollution, the constituents of “air pollution” vary according to place and period. Also studies by Christiani [13] and his team point out that particulate matter (PM), which is found in urban air, is a potential risk factor for lung cancer with increased PM exposure ≤ 2.5 μm in aerodynamic diameter. The work of Raaschou-Nielsen and his team reported by Kanwal [10] in this work in 2017 demonstrates that non-smokers and individuals residing near roads who find themselves in cities have a high risk of lung cancer associated with pollution of environmental air. Motor vehicle exhaust produces nitrogen oxide and nitrogen dioxide and is responsible for lung cancer in urban populations [10]. Lung cancer deaths are attributable to long-term exposure to ambient PM2.5 [14, 15]. It is described that exposure to PM2.5 is more harmful in men and the elderly. Air pollution is therefore responsible for lung cancer. There is also nowadays a phenomenon of passage from domestic air pollution to ambient air pollution [15]. PM2.5, which plays a very strong role in air pollution, has significant effects on human health in general and on lung cancer mortality in particular [15]. Ambient air pollution by benzene, toluene, ethylbenzene, and xylene (BTEX) has been shown to be linked to lung cancer in the population [16]. Pollution is one of the phenomena to fight for the prevention of lung cancer.
Nowadays, it is important to carefully note that occupational exposures play a major role in the factors of the increased development of lung cancer, and the risk of lung cancer is also observed in a very high way among workers in a certain number of industries and professions [6]. It is also important to note that the most important occupational lung carcinogens would be PAHs, asbestos, silica, radon, and heavy metals [6].
It is important to note that the elements initially listed, namely smoking, food and alcohol, exposure to ionizing rays, environmental pollution are part of the lifestyle habits that can be corrected to prevent lung cancer. Several studies have identified risk factors for lung cancer as well as preventive measures against this pathology (Table 2).
Table summarizing the risk factors studied in research studies
| No. | Author(s) and year | Study | Lung cancer risk factors | Preventative measure |
|---|---|---|---|---|
| 1 | Siddiqui et al., 2022 [12]. | Lung cancer. | Smoking. Exposure to carcinogens such as asbestos. Environmental and genetic factors. Exposure to chromium, nickel, arsenic and PAHs. Other risk factors: asbestos and radon. | Smoking cessation in all individuals (effective preventive measure). Establish screening measures to significantly reduce morbidity and mortality associated with lung cancer. |
| 2 | Liu et al., 2021 [14]. | Lung cancer death attributable to long-term ambient particulate matter PM2.5 exposure in East Asian countries during 1990–2019. | Long-term exposure to ambient particles PM2.5. | Reduction of ambient particulate air pollution PM2.5: public health program required. |
| 3 | Wu et al., 2021 [15]. | The epidemiological trends in the burden of lung cancer attributable to PM2.5 exposure in China. | Air pollution by PM2.5. | Regulation of ambient air pollution. |
| 4 | Christiani et al., 2021 [13]. | Ambient air pollution and lung cancer: nature and nurture. | Air pollution by PAHs and metals such as arsenic, nickel and chromium. Increased PM exposure ≤ 2.5 μm. Genetic risk factors. | Reduction of air pollution. |
| 5 | Khorrami et al., 2021 [16]. | Multiple air pollutant exposure and lung cancer in Tehran, Iran. | Air pollution by:
| Reduction of air pollution. |
| 6 | Schabath et al., 2019 [3] | Cancer progress and priorities: lung cancer. | Tobacco smoking. Secondhand smoke. Electronic cigarettes. Other tobacco use (cigars, pipes, water pipes). Smoked cannabis. Radon. Asbestos. History of COPD, emphysema, or chronic bronchitis. History of asthma. History of pneumonia. History of Chlamydia pneumoniae. History of tuberculosis. HIV. | Smoking cessation. |
| 7 | Kanwal et al., 2017 [10]. | Familial risk for lung cancer (review). | Tobacco smoking. Environmental risks. Indoor air pollution. Outdoor air pollution. Heritable factors. | Smoking cessation. Fight against environmental pollution. |
| 8 | Malhotra et al., 2016 [6]. | Risk factors for lung cancer worldwide. | Tobacco smoking. Genetic risk factors:
Diet and alcohol. Chronic inflammation due to infections and other medical parameters. Ionizing radiation. Occupational exposures:
Air pollution. Other risk factors. | Stopping the consumption of tobacco in all its forms. Adopt a diet rich in vegetables and fruits, especially crucifers. |
| 9 | Molina et al., 2008 [11]. | Non–small cell lung cancer: epidemiology, risk factors, treatment, and survivorship. | Smoking. Secondary or passive smoking. Diet. Food supplements. Alcohol. Air pollution. Occupational exposure. Genetic risk factors. | Smoking cessation. Regular consumption of fruits and vegetables which are very rich in vitamins, antioxidant molecules and micronutrients such as:
β-cryptoxanthin (BCX) showed a more consistent protective effect. Carotenoids decrease lung cancer risk. Studies have shown that vitamins C and vitamin E have protective roles. |
COPD: chronic obstructive pulmonary disease; HIV: human immunodeficiency virus
According to the research work carried out by Chhikara’s team published in 2023 on “Global Cancer Statistics 2022: the trends projection analysis”, it is concluded that lung cancer is the main type of cancer where we had a rate high incidence and high death rate compared to other types of cancer [17]. The same observation is observed with the work carried out by GLOBOCAN and the World Health Organization (WHO), where it is noted that the incidence rate and the mortality rate of lung cancer are high compared to other types of cancer (Figures 4, 5, 6, 7, 8, and 9) [18]. Lung cancer mortality is very high in both men and women.
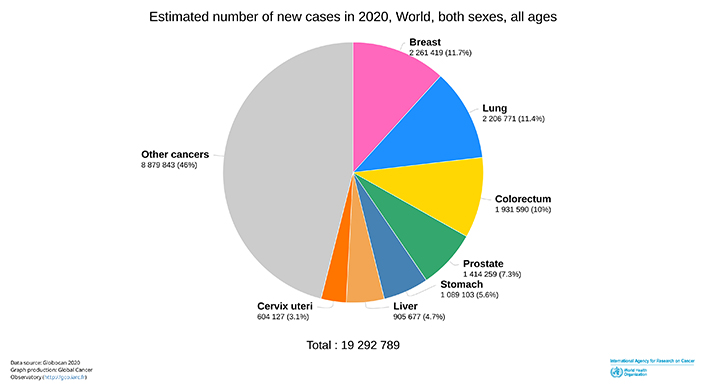
Estimated number of new cases in 2020, world, both sexes, all ages [18]
Note. Reprinted with permission from “Cancer Today” by IARC; c2020 (https://gco.iarc.fr/today/home). © IARC.
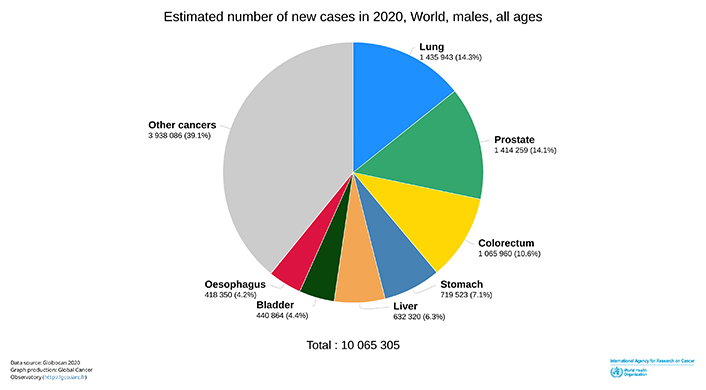
Estimated number of new cases in 2020, world, males, all ages [18]
Note. Reprinted with permission from “Cancer Today” by IARC; c2020 (https://gco.iarc.fr/today/home). © IARC.
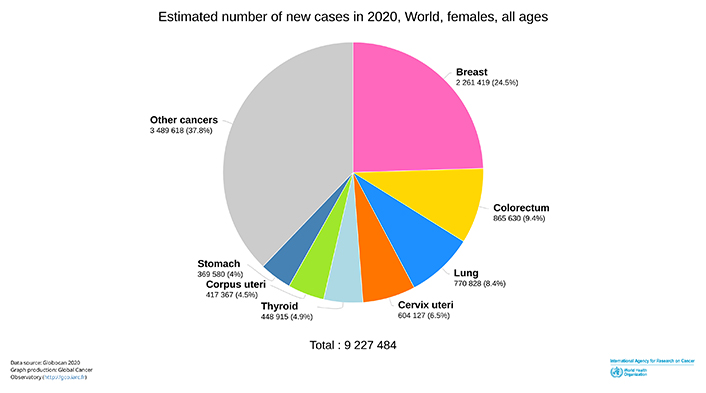
Estimated number of new cases in 2020, world, females, all ages [18]
Note. Reprinted with permission from “Cancer Today” by IARC; c2020 (https://gco.iarc.fr/today/home). © IARC.
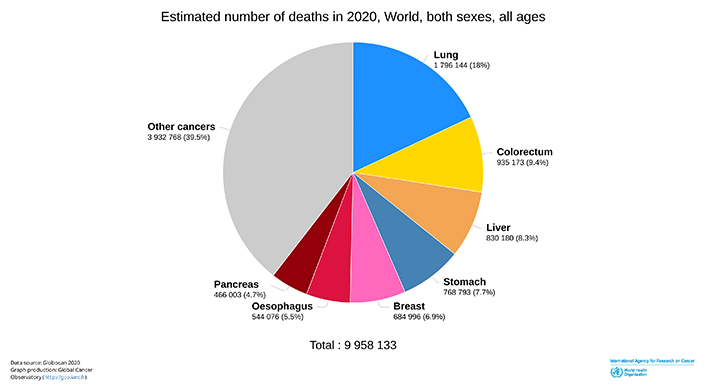
Estimated number of deaths in 2020, world, both sexes, all ages [18]
Note. Reprinted with permission from “Cancer Today” by IARC; c2020 (https://gco.iarc.fr/today/home). © IARC.
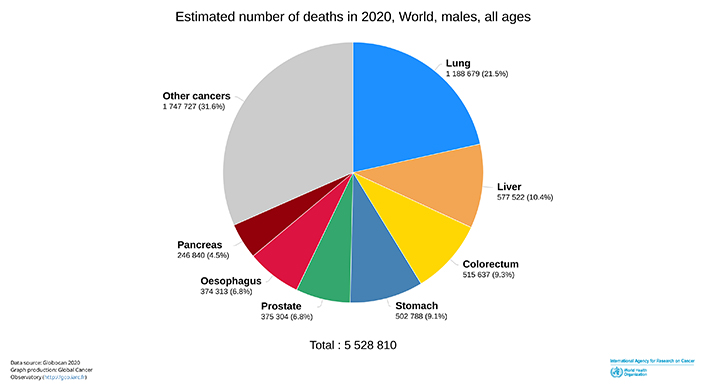
Estimated number of deaths in 2020, world, males, all ages [18]
Note. Reprinted with permission from “Cancer Today” by IARC; c2020 (https://gco.iarc.fr/today/home). © IARC.
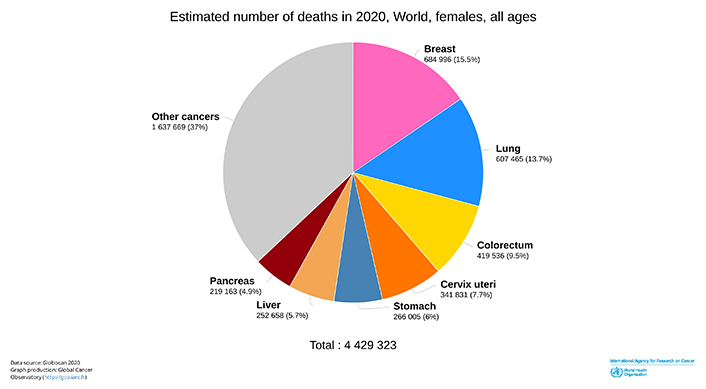
Estimated number of deaths in 2020, world, females, all ages [18]
Note. Reprinted with permission from “Cancer Today” by IARC; c2020 (https://gco.iarc.fr/today/home). © IARC.
This article has highlighted the causes of the development of lung cancer: lifestyle habits, genetic factors, and environmental pollution. This review article makes it possible on the one hand to shed light in general on the development factors of this cancer in order to adopt adequate preventive measures by correcting our lifestyle habits which are responsible for the appearance and development of this cancer. And on the other hand, this article sheds light on environmental factors including environmental pollution in order to allow the development of regulations and health policies to curb this environmental pollution which is involved in lung cancer.
According to a 1983 WHO meeting on lung cancer, “lung cancer is the leading cause of cancer death in many industrialized countries, and it is quite possible that it will soon reach the same sad superiority in developing countries. It ranks first among the causes of male cancer death in the following countries or territories: Federal Republic of Germany, Australia, Austria, Belgium, Bulgaria, Cuba, Denmark, Egypt, United States of America, Finland, France, Greece, China (Hong Kong), Hungary, Ireland, Israel, Italy, Luxembourg, New Zealand, Netherlands, Philippines, Poland, German Democratic Republic, Romania, United Kingdom, Singapore, Switzerland, Czechoslovakia, Thailand, Uruguay, Yugoslavia and Zimbabwe (Bulawayo). Nowadays in some countries, the worrying phenomenon is the increase in the incidence of lung cancer more in women than in men” [19]. Also, in this same article [19], it is noted that “At the origin of 80% to 90% of all lung cancers recorded in industrialized countries, the main cause of which was related to tobacco consumption”. Its harmful effects have been widely studied and discussed, and WHO Expert Committees have already made important recommendations concerning measures to be taken in the fight against smoking [19]. It must be said that lung cancer has long been a major concern of public health at the international level, as well as the fight against smoking, which is the main cause of lung cancer. Preventive measures are more reinforced nowadays for the fight against smoking in the context of the development of lung cancer [20, 21]. Nowadays the incidence of lung cancer has become very complex in men than in women [22–24]. Compared to the report of the WHO meeting in 1983, the rise of lung cancer nowadays among women becomes more and more astonishing [25, 26]. Nowadays, it is noted that the incidence and mortality of lung cancer have increased significantly among women worldwide [27]. Curbing smoking would greatly reduce not only the appearance of lung cancer but also the mortality linked to smoking and lung cancer without forgetting of course the other factors of lung cancer [20]. Indeed, a study on the impact of reducing smoking on lung cancer mortality in the United States from 1975 to 2000 shows that reducing and controlling smoking is very effective in fighting lung cancer, and thus curb mortality due to smoking and lung cancer [28]. Also, environmental pollution being a factor of lung cancer [29, 30], it is fundamental to fight against all forms of pollution for better prevention of lung cancer. Indeed, population and economic growth in countries along with increased urbanization present a new risk of cancer development such as the exposure of a large number of people to air pollution [31].
Studies also show that air pollution on our health is involved in the development of many cancers including lung cancer. It shows in Figures 10 and 11 that the image of environmental pollution.

Environmental pollution [32]
Note. Reprinted from “Ambient air quality in the Czech Republic: past and present” by Hůnová I. Atmosphere. 2020;11:214 (https://www.mdpi.com/2073-4433/11/2/214). CC BY.

Environmental pollution [33]
Note. Reprinted with permission from “Pollution de l’air” (https://cancer.ca/fr/cancer-information/reduce-your-risk/know-your-environment/air-pollution). © 2023 Société canadienne du cancer.
Air pollution is a collection of chemicals, particles and other elements released into the air that cause health problems (Figure 12) including lung cancer. Molecules of these fumes that spill into the environment interact with DNA and cause not only cancers but cardiovascular disorders and pulmonary pathologies. Molecules of these fumes that spill into the environment interact with DNA and cause not only cancers but cardiovascular disorders and pulmonary pathologies [34].
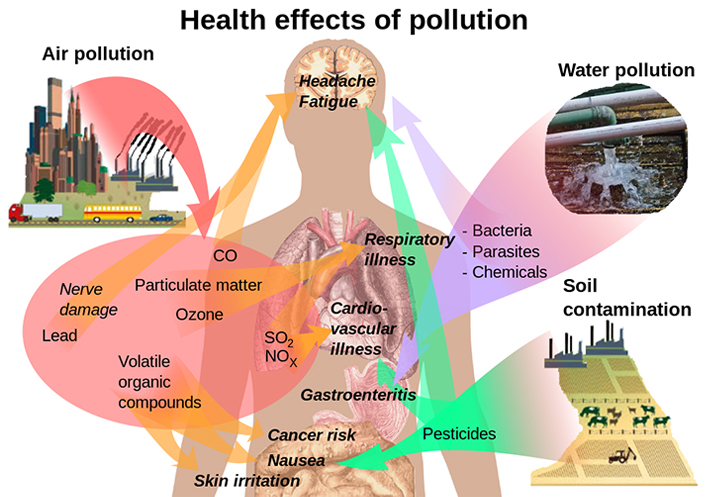
The effects of pollution on health [35]
Note. Reprinted from “File:Health effects of pollution.svg” by Häggström M (https://commons.wikimedia.org/wiki/File:Health_effects_of_pollution.svg). CC0.
Many molecular compounds are in smoke that are known to be involved in cancer, including aromatic heterocyclic amines (AHAs) which are a family of substances that are formed during the cooking of meat and fish and which are also present in cigarette smoke or car exhaust as shown in Figure 13 [34, 36]. They are classified by the IARC as carcinogenic to humans.

Heterocyclic amines (HA) are chemical compounds present in cigarette smoke, formed during the cooking of meats, fish or poultry, especially when the meat is grilled at high temperatures or cooked for a long time. (A) [37], (B) [38], (C) [39], (D) [40]
Note. (A) Reprinted from “Chain smoking” by Wikipedia (https://en.wikipedia.org/w/index.php?title=Chain_smoking&oldid=1144148289). CC BY-SA; (B) reprinted from “Barbecue” by Wikipedia (https://en.wikipedia.org/w/index.php?title=Barbecue&oldid=1165454282). CC BY-SA; (C) reprinted from “Mobile source air pollution” by Wikipedia (https://en.wikipedia.org/w/index.php?title=Mobile_source_air_pollution&oldid=1165092353). CC BY-SA; (D) reprinted from “File:Cuisson de sardines au barbecue.jpg” by Wikipedia (https://commons.wikimedia.org/wiki/File:Cuisson_de_sardines_au_barbecue.jpg). CC BY-SA.
Several studies, including the research work of Mazières and his team [41, 42], show that smoking is the main cause of lung cancer. Several risk factors are involved in the development of lung cancer (Figure 14).
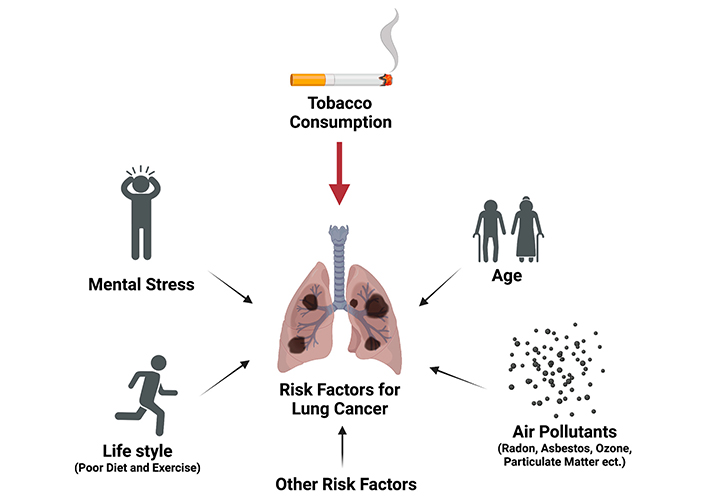
Lung cancer risk factors [43]
Note. Reprinted from “Opportunities and challenges of Kava in lung cancer prevention” by Freeman B, Mamallapalli J, Bian T, Ballas K, Lynch A, Scala A, et al. Int J Mol Sci. 2023;24:9539 (https://www.mdpi.com/1422-0067/24/11/9539). CC BY.
Smoking, diet and alcohol, genetic risk factors, exposure to ionizing radiation, occupational exposure, environmental pollution are factors that are involved in the development of lung cancer. As for occupational exposure, this must be a major policy objective in terms of the health and well-being of the population in order to put in place safety measures and better working conditions for workers. The young people of today being the next generation of tomorrow, we must plan and multiply more awareness sessions to raise awareness among young people against smoking in order to considerably reduce the smoking rate in our communities. The various factors studied in this article in relation to the development of lung cancer have an important impact on the state of health and well-being. These factors are not only implicated in the appearance of lung cancer but also in other types of cancer.
For example, the consumption of alcohol is also implicated in pathologies such as liver cancer [44–47], hepatocellular carcinoma [45, 46, 48] and cirrhosis [49].
Indeed, alcoholic beverages are implicated in the appearance of malignant tumors of the oral cavity, pharynx, larynx, esophagus, liver, colon and breast [44]. It should be emphasized that the metabolism of alcohol in the liver leads to the production of reactive oxygen molecules, the induction of cytochrome P450 activity and the reduction of antioxidants [44]. It shows in Figure 15 that the induction of cancer by alcohol consumption.
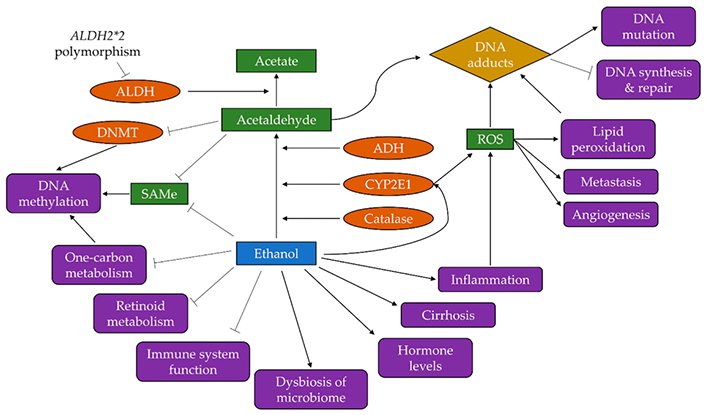
Mechanism of cancer induction by alcohol [50]. ALDH: aldehyde dehydrogenase; DNMT: DNA methyltransferase; SAMe: S-adenosylmethionine; ADH: antidiuretic hormone; CYP2E1: cytochrome P450 2E1; ROS: reactive oxygen species
Note. Reprinted from “Alcohol and cancer: epidemiology and biological mechanisms” by Rumgay H, Murphy N, Ferrari P, Soerjomataram I. Nutrients. 2021;13:3173 (https://www.mdpi.com/2072-6643/13/9/3173). CC BY.
Several mechanisms demonstrate how excessive alcohol consumption leads to the development of cancer. It must be said that one of the important mechanisms explaining how alcohol induces cancer is presented here. The following figure (Figure 16) below translates a diagram presenting the mechanisms by which alcohol can induce carcinogenesis. At first it must be said that ethanol (alcohol) is oxidized to acetaldehyde by ADH, which binds to DNA. This phenomenon is made possible thanks to mutations or polymorphism phenomena. Acetaldehyde can cause hybrid protein adducts that will destabilize the functioning of proteins that regulate lipid peroxidation and nucleic acid oxidation. Excessive alcohol consumption will therefore lead to the induction of the CYP2E1 pathway and may indirectly contribute to the significant production of acetaldehyde and ROS. Excess alcohol increases the catabolism of retinoic acid by CYP2E1. The interaction of retinoids with different signaling pathways, including estrogen signaling, can promote the proliferation and establishment of precancerous cells. Chronic consumption of ethanol (alcohol) is also associated with a considerable failure of the immune surveillance capacity of tumor cells [51].
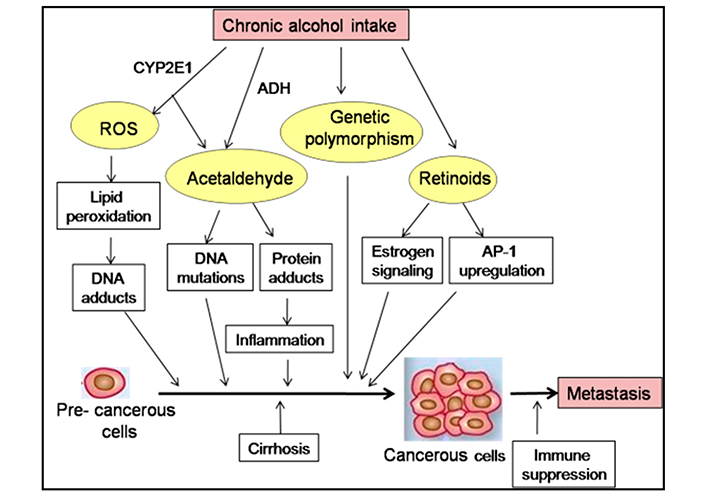
Mechanism of cancer induction by alcohol [51]. AP-1: activator protein-1
Note. Reprinted from “Alcohol and cancer: mechanisms and therapies” by Ratna A, Mandrekar P. Biomolecules. 2017;7:61 (https://www.mdpi.com/2218-273X/7/3/61). CC BY.
Smoking contributes to the development of cancer by attacking important functions of cells in the body [52]. The following figure (Figure 17) shows how smoking induces cancer. Smoking induces carcinogenesis by causing metabolic changes at the DNA level, the formation of carcinogenic DNA adducts and will also lead to mutations. This will mainly cause the inhibition of genes such as p53 which is a tumor suppressor; and mutations in the Kirsten rat sarcoma viral oncogene homolog (KRAS) oncogene [53, 54]. Smoking is considered a major risk factor in the development of lung disease worldwide. Oxidative stress (OS) and/or lipid peroxidation (LP) induced by cigarette smoke are implicated in the pathogenesis of lung cancer [55].
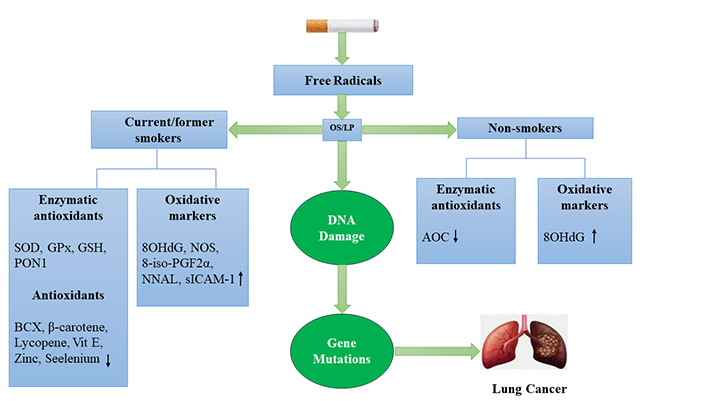
Mechanisms that contribute to tobacco-caused lung cancer [55]. ↓: Decrease; ↑: Increase; SOD: superoxide dismutase; GPx: glutathione peroxidase; GSH: glutathione; PON1: paraoxonase; Vit E: vitamin E; 8OHdG: 8-hyroxy-2-deoxyguanosine; NOS: nitric oxide synthase; 8-iso-PGF2α: 8-iso-prostaglandin-F2alpha; NNAL: 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol; sICAM-1: soluble intercellular adhesion molecule-1; AOC: antioxidant capacity
Note. Reprinted from “Dietary antioxidants and lung cancer risk in smokers and non-smokers” by lsharairi NA. Healthcare (Basel). 2022;10:2501 (https://www.mdpi.com/2227-9032/10/12/2501). CC BY.
Smoking also contributes to the collapse of the immune system and thus increases the risk of cancer in most organs, mainly the lung [56].
It has also recently been demonstrated that smoking destabilizes the functions of alveolar macrophages, which are sentinel cells strategically positioned at the interface between the lumen of the respiratory tract and the alveolar spaces [57, 58]. They are the most abundant immune cells and the first line of defense against inhaled particles and pathogens [57, 58].
Other studies have also shown that apart from lung cancer caused by smoking, cigarette smoke also destabilizes the immune system, promotes inflammation and the development of allergy (Figure 18) [59].
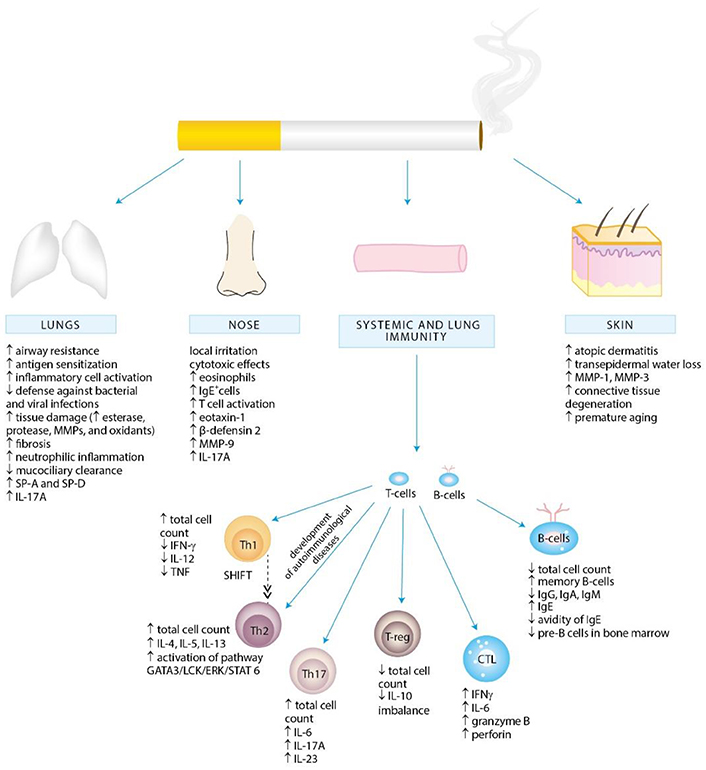
Cigarette smoke exposure-associated alternations in local and systemic immunity promoting inflammation and allergy development [59]. SP: surfactant protein; IL: interleukin; T-cell: T lymphocyte; MMP: matrix metalloproteinase; IFN-γ: interferon-gamma; GATA3: GATA binding protein 3; LCK: lymphocyte-specific protein tyrosine kinase; ERK: extracellular signal-regulated kinase; STAT: signal transducer and activator of transcription; Th: helper T; T-reg: regulatory T cell; CTL: cytotoxic T lymphocytes; B-cells: B lymphocytes; Ig: immunoglobulin
Note. Reprinted from “Tobacco smoke induces and alters immune responses in the lung triggering inflammation, allergy, asthma and other lung diseases: a mechanistic review” by Strzelak A, Ratajczak A, Adamiec A, Feleszko W. Int J Environ Res Public Health. 2018;15:1033 (https://www.mdpi.com/1660-4601/15/5/1033). CC BY.
From the previous figures, it is important to note that lung cancer is not only the cancer that ranks first among all types of cancer, but also more prevalent in men than in women. For this reason, it would be very important to conduct a specific study to know more in depth why this cancer is higher in men than in women in terms of incidence and mortality. This will make it possible to properly orient the prevention strategies to curb this pathology.
This article helps to understand that lung cancer is the leading cause of cancer death in the world and a preventable disease that can be effectively prevented by taking adequate preventive measures. It is found that smoking remains the main risk factor for the development of lung cancer. Besides smoking, it is also important to consider other factors such as chronic lung disease, lung infections, environmental and occupational exposures, and lifestyle factors. As long as smoking remains the main risk factor for lung cancer, prevention of the disease would be centered on abstinence from consumption or stopping smoking, without forgetting the appropriate measures to be taken to fight against air pollution. Cancer is more prevalent in men than in women. Indeed, a rigorous study will make it possible to understand more in depth the factors of the development of this pathology in its complexity and would help policy makers and medical practitioners to make decisions concerning the implementation of strategies to reduce the incidence and mortality. of this pathology. This will also allow the implementation of the means of sustainable prevention without forgetting the sensitization of the population which is very important in this fight for the prevention of cancers.
CYP2E1: cytochrome P450 2E1
IARC: International Agency for Research on Cancer
PAHs: polycyclic aromatic hydrocarbons
PM: particulate matter
ROS: reactive oxygen species
WHO: World Health Organization
HA: Conceptualization, Project administration, Writing—original draft, Writing—review & editing. RF: Conceptualization, Writing—original draft, Writing—review & editing. MB: Writing—original draft, Writing—review & editing. All authors have read and accepted the published version of the manuscript.
The authors declare they have no conflicts of interest.
Not applicable.
Not applicable.
Not applicable.
Not applicable.
Not applicable.
© The Author(s) 2023.
Open Exploration maintains a neutral stance regarding jurisdictional claims in published maps and institutional affiliations.
Copyright: © The Author(s) 2023. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
