Affiliation:
1Department of Psychiatry, Epidemiology of Psychiatric Disorders and Mental Health Research Unit, Faculty of Medicine, Chulalongkorn University, Bangkok 10330, Thailand
2Department of Psychiatry, King Chulalongkorn Memorial Hospital, Bangkok 10330, Thailand
Email: Rasmon.k@chula.ac.th
ORCID: https://orcid.org/0000-0002-5311-1930
Affiliation:
1Department of Psychiatry, Epidemiology of Psychiatric Disorders and Mental Health Research Unit, Faculty of Medicine, Chulalongkorn University, Bangkok 10330, Thailand
ORCID: https://orcid.org/0009-0006-4225-3163
Affiliation:
1Department of Psychiatry, Epidemiology of Psychiatric Disorders and Mental Health Research Unit, Faculty of Medicine, Chulalongkorn University, Bangkok 10330, Thailand
ORCID: https://orcid.org/0009-0004-8634-9592
Affiliation:
3Department of Radiology, Faculty of Medicine, Mahidol University, Bangkok 10400, Thailand
ORCID: https://orcid.org/0000-0002-2230-1782
Explor Med. 2023;4:441–452 DOI: https://doi.org/10.37349/emed.2023.00154
Received: January 04, 2023 Accepted: May 08, 2023 Published: August 30, 2023
Academic Editor: Richard M. Sherva, Boston University School of Medicine, USA
The article belongs to the special issue The Biological Basis of Substance Use Disorders
Aim: Cigarette smoking is an addictive behavior that requires high motivation to change, a phenotype related to the functional activity of the brain. The study aims to examine motivation to change among cigarette smokers and to study the association between functional brain activity and motivation to change smoking behaviors.
Methods: Motivation to change smoking behaviors of 107 current smokers receiving services in a university hospital was obtained using the Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES). Brain activities related to motivation to change were also explored in a subgroup using functional magnetic resonance imaging (fMRI).
Results: The results showed that most of the current smokers (n = 68, 63.6%) were low motivated to change despite receiving health-related services. Brain activities in the left of the temporal, frontal gyrus, and superior medial gyrus of smokers with motivation were greater activated than those without. In contrast, the brain activities in the left precentral gyrus and bilateral paracentral lobules of smokers without motivation were greater activated.
Conclusions: These preliminary results show the differences in brain activities between smokers with and without motivation to change and warrant further research to see if motivated smokers can quit smoking using a series of strategies based on their functional activities of the brain.
Motivation to change is the wants or needs that direct the change of a behavior toward a goal [1]. Motivation to change is a key component in the field of addiction, since it supports people with addiction problems to voluntarily change their addictive behaviors [2, 3]. The process of change, so-called the stage of change, consists of five stages that are precontemplation, contemplation, preparation, action, and maintenance [4]. The later the stages of change, the higher the motivation to change the addictive behaviors [5].
Cigarette smoking, an addictive behavior, has been reported worldwide and has been found to be a major risk to human health [6]. Cigarette smoking can cause lung cancer, respiratory diseases, cardiovascular diseases, and other diseases in various areas such as oral health, reproductive health, endocrine and immune function [7–13]. The combination of interventions such as nicotine replacement therapy, bupropion, varenicline, smoking cessation counseling, contingency management, relapse prevention, relaxation techniques, and cognitive behavioral therapy can improve smoking abstinence or reduce craving for smoking [14–16]. However, motivation to change is an important factor for cigarette smokers to voluntarily enter the treatment program or try to quit smoking by themselves, especially when receiving a medical intervention related to smoking harms [17]. Other factors related to smoking cessation success include older age at smoking onset, shorter duration of smoking, low level of nicotine dependence, being married, higher level of education, being employed, having mental illness [18–24], and altered functional brain connectivity in the insula network [25].
Previous reports show that functional activities in various areas of the brain is associated with cessation of smoking. For example, decreased functional activity in the anterior cingulate cortex was related to reduced craving for smoking [26]. The subcortical caudate nucleus and many cortical brain areas were activated more strongly during extended smoking abstinence [27]. Experienced smokers had greater activity in the bilateral middle temporal gyrus when faced with cigarette decisions than occasional smokers [28]. However, smoking cessation can be predicted by motivation to change smoking behaviors [29]. To our knowledge, no research has studied the association between functional brain activity and motivation to change among cigarette smokers.
Thus, the present study aims to examine motivation to change among cigarette smokers who received health-related services in a university hospital and to study the association between functional brain activity and motivation to change smoking behaviors in the subpopulation of the sample. Knowing the association between motivation to change and functional activity in the brain could be the basic knowledge to understand human motivation directed toward the personal positive goal of changing oneself toward smoking cessation.
In this cross-sectional study, motivation to change smoking behaviors, severity of cigarette dependence, and demographics of the 107 current smokers—defined as having smoked in the past month—aged 18 or older who received services at a university hospital between 2014 and 2016 were obtained. Participants were recruited from the outpatient general psychiatric service and the routine medical check-up service [30], a service for healthy people who wanted to annually check their general health by themselves or by their workplace health programs. Individuals who participated in a smoking cessation program or research, and who used illegal substances (i.e., methamphetamine, opioids, cannabis, and kratom) or had other brain diseases (i.e., stroke, epilepsy, dementia, and movement disorders) were excluded.
Furthermore, 14 subjects from the check-up service were randomly selected to undergo the study of functional brain imaging activity related to motivation to change (see below). Subjects who were using any medications, having psychiatric diseases (i.e., psychotic disorders, mood disorders, anxiety disorders, obsessive-compulsive disorder, and alcohol dependence) were excluded from the brain imaging procedure. All participants gave their informed consent in writing and the study procedures were approved by the Institutional Review Board of the Chulalongkorn University Faculty of Medicine (No. 273/59).
All participants were interviewed using the Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES), the Semi-Structured Assessment for Drug Dependence and Alcoholism (SSADDA) and the Mini International Neuropsychiatric Interview (M.I.N.I.) lifetime. Sections A and B of the SSADDA were used to collect demographic data and to screen for medical illnesses of the participants [31]. The M.I.N.I. lifetime, a short structured diagnostic interview, was used to screen for psychiatric disorders and substance dependence [32, 33]. The level of current smoking dependence was assessed using the Fagerström Test for Nicotine Dependence (FTND) in the 14 healthy subjects before the study of functional brain imaging activity related to the motivation to change. The FTND had 6 questions labeled yes and no answers as scoring 1 and 0 respectively, and multiple-choice items are scored from 0 to 3. FTND scores of 0–2, 3–4 and 5–10 are defined as having low, moderate, and high levels of nicotine dependence [34].
SOCRATES was used to assess motivation to change smoking behaviors. The SOCRATES has 19 questions divided into 3 aspects, including recognition (of the problems; 7 questions), ambivalence (to change; 4 questions), and taking steps (of change; 8 questions). Each question has five Likert scores: 5 = totally agree, 4 = agree, 3 = uncertain, 2 = disagree, and 1 = totally disagree. In this study, the scores of the questions for each aspect were summed and interpreted into low and high levels of recognition (7–34 = low, 35 = high), ambivalence (4–16 = low, 17–20 = high), and taking steps (8–35 = low, 36–40 = high) based on the original version of SOCRATES that defined levels of each aspect from very low, low and moderate (combined into low level in this study) to high and very high levels (combined into high level in this study). The three aspects were then further interpreted and classified elsewhere into levels of the well-established stages of change [35] including precontemplation (no recognition at all), contemplation (still ambivalent to change), preparation (recognition, but still no action), and action/maintenance (already taken the steps to change and maintain the change). In this study, the low scores in all aspects of SOCRATES were defined as the precontemplation stage, the high scores only in the ambivalence aspect defined as the contemplation stage, the high scores only in the recognition aspect or both the recognition and the ambivalence aspects defined as the preparation stage, and the high scores in taking steps defined as action or maintenance stage. To define the motivation to change, only current smokers who were in the contemplation, preparation and action/maintenance stages were defined as having motivation to change, while those in the precontemplation stage were defined as having no motivation to change.
Subjects who passed the screening criteria for the brain imaging study underwent brain scan using functional magnetic resonance imaging (fMRI). Before the scan, participants completed the FTND and were asked to refrain from smoking for at least 1 h. Before entering the scanner, participants were instructed to look at the picture shown on a 15.24 cm × 22.86 cm screen projected onto a mirror mounted on the head coil (approximately 45.72 cm distance from head). A visual fMRI cigarette cue reactivity task consisted of 5 min 36 s runs in block design which included the 11 s grayscale picture before the first block, the 27 s neutral images that consisted of 9 images (each image was shown in 3 s), the 27 s smoking-related images that consisted of 9 images (each image was shown in 3 s), and the 27 s control grayscale image. The 27 s neutral images, the 27 s smoking-related images, and the 27 s control grayscale image were systematically ordered and shown in 4 blocks. The task was constructed using iMovie (Video creator tool).
All brain scans were performed at the Advanced Diagnostic Imaging Center. The Philips Ingenia 3.0T scanner was used. Task-based functional scans were acquired using an echo-planar pulse sequence with repetition time (TR) = 2,000 ms, echo time (TE) = 35 ms and flip angle = 90°. Each pulse recorded 24 oblique axial slices with a thickness of 6 mm; matrix size was 96 × 96 generating 2.4 × 2.4 × 6 mm voxels.
Analyses were performed separately for smokers from the psychiatric service and those from check-up services. Descriptive statistics were used to explain demographics, the severity of nicotine dependence, motivation to change smoking behavior, and stage of change. The three aspects of motivation to change, including recognition, ambivalence, and taking steps of the SOCRATES scores, were shown in mean and standard deviation (SD), and the overall SOCRATES scores were presented in Z-score. The t-test, the chi-square test and Fisher’s exact test were used to compare the differences in demographics, motivation to change smoking behavior, and stage of change between smokers from the two services using SPSS version 22.0.
The imaging data were analyzed using Statistical Parametric Mapping (SPM) version 2. Regarding the data preprocessing process, functional images were slice-timing corrected, realigned to the mean image of the first functional run (motion-corrected), smoothed with a Gaussian kernel with a full-width half maximum (FWHM) of 6 mm, and normalized into the Montreal Neurological Institute (MNI) template. Regarding the calculation of parameters to identify differences in the magnitude of the Blood Oxygenation Level Dependent (BOLD) signal for smokers with and without motivation, contrast maps were created by contrasting the parameter estimates. The two-sample t-test was used to analyze differences between groups at a significant level of 0.05 and 0.001 for correction for multiple tests.
All current cigarette smokers recruited in the study were male. Of 107 smokers, 24 (22.4%) were from the psychiatric clinic and the other 83 (77.6%) smokers were from the routine medical check-up clinic. Although the smokers of the psychiatric services in the study had a lower level of education than those of the medical check-up clinic (P = 0.002), other demographics (e.g., age, marital status, and employment status) were not different (Table 1).
Comparing demographics, SOCRATES scores and motivation to change the smoking behaviors between current smokers from psychiatric and routine medical check-up services
| Demographics | Psychiatric service N = 24 Mean (SD) or n (%) | Check-up service N = 83 Mean (SD) or n (%) | P-values |
|---|---|---|---|
| Age (years) | 39.17 (10.30) | 40.73 (13.46) | 0.599 |
| Marital status | 0.572 | ||
| Single | 14 (58.3) | 43 (51.8) | |
| Married | 10 (41.7) | 40 (48.2) | |
| Education | 0.002* | ||
| ≤ High school | 21 (87.5) | 44 (53.0) | |
| > High school | 3 (12.5) | 39 (47.0) | |
| Employment | 1.000 | ||
| No | 2 (8.3) | 6 (7.2) | |
| Yes | 22 (91.7) | 77 (92.8) | |
| SOCRATES scores | |||
| Overall | 0.05 (1.12) | –0.01 (0.97) | 0.790 |
| Recognition | 25.46 (7.14) | 24.29 (6.27) | 0.437 |
| Ambivalence | 14.63 (3.88) | 14.58 (3.17) | 0.952 |
| Taking steps | 26.63 (6.68) | 27.11 (7.61) | 0.779 |
| Stages of change | 0.546 | ||
| Precontemplation | 14 (58.3) | 54 (65.1) | |
| Contemplation or higher | 10 (41.7) | 29 (34.9) |
* P < 0.01
The mean scores for three aspects of motivation to change are presented in Table 1. All current smokers in the psychiatric service or the medical check-up service had low levels in the three aspects of motivation to change, including recognition (25.46 ± 7.14 and 24.29 ± 6.27), ambivalence (14.63 ± 3.88 and 14.58 ± 3.17), and taking steps (26.63 ± 6.68 and 27.11 ± 7.61). The overall scores on recognition, ambivalence, and the dimension of taking steps were not different between current smokers from psychiatric and non-psychiatric clinics (P > 0.05).
Regarding the stage of change and motivation to change, 68 (63.6%) of 107 current smokers were in the precontemplation stage of change, the stage that did not reflect motivation to change. Specifically, 58.3% and 65.1% of current smokers from the psychiatric service and the routine medical check-up service, respectively, were in the precontemplation stage of change and were not statistically different from each other in their motivation to change (P > 0.05) (Table 1).
Of the 14 current smokers who underwent fMRI, 4 (28.6%) and 10 (71.4%) were found to have and lack motivation to change smoking behaviors, respectively. Current smokers with motivation to change did not differ from those without regarding to age, body mass index (BMI), marital status, education, employment, age of starting smoking, and duration of smoking. However, smokers with motivation to change had higher levels of nicotine dependence than current smokers without motivation to change (P = 0.001) (Table 2).
Comparing demographics of current smokers with and without motivation to change their smoking behaviors
| Demographics | With motivation (N = 4) Mean (SD) or n (%) | Without motivation (N = 10) Mean (SD) or n (%) | P-values |
|---|---|---|---|
| Age (years) | 45.00 (3.92) | 34.60 (10.83) | 0.092 |
| BMI | 25.17 (4.18) | 24.84 (4.22) | 0.896 |
| Marital status | 0.689 | ||
| Single | 3 (75.0) | 7 (70.0) | |
| Married | 1 (25.0) | 3 (30.0) | |
| Education | 0.670 | ||
| ≤ High school | 1 (25.0) | 2 (20.0) | |
| > High school | 3 (75.0) | 8 (80.0) | |
| Employment | N/A | ||
| No | 4 (100.0) | 10 (100.0) | |
| Yes | 0 (0.0) | 0 (0.0) | |
| Age of smoking onset (years) | 16.75 (0.96) | 15.70 (2.50) | 0.438 |
| Duration of smoking (years) | 28.25 (4.65) | 18.90 (11.38) | 0.144 |
| Level of nicotine dependence | 4.75 (0.96) | 1.70 (1.34) | 0.001* |
* P < 0.01; N/A: not applicable
Cigarette smokers with motivation to change, compared to those without motivation to change, elicited brain activation in four clusters in the brain (Table 3 and Figure 1), including the left inferior temporal gyrus, the middle temporal gyrus, the superior frontal gyrus, and the superior medial gyrus. On the contrary, current smokers without motivation, comparing with those with motivation to change, caused brain activation in 3 clusters (Table 4 and Figure 2), including the left precentral gyrus and the bilateral paracentral lobe. After multiple comparison correction, none of the results remained statistically significant.
Regions of the brain where current smokers with motivation displayed greater brain activities than those without motivation
| Regions* | Brodmann areas | Peak MNI coordinates | ||
|---|---|---|---|---|
| x | y | z | ||
| Left inferior temporal gyrus | 20 | –55 | –24 | –23 |
| –55 | –30 | –18 | ||
| Left middle temporal gyrus | 21 | –65 | –27 | –13 |
| Left superior frontal gyrus | 11, 12 | –11 | 43 | 46 |
| –11 | 38 | 51 | ||
| Left superior medial gyrus | N/A | –9 | 36 | 54 |
* Two sample t-test, P < 0.05 uncorrected. None of the areas remain significant after multiple comparison correction (adjusted significant threshold at P = 0.001). N/A: not applicable
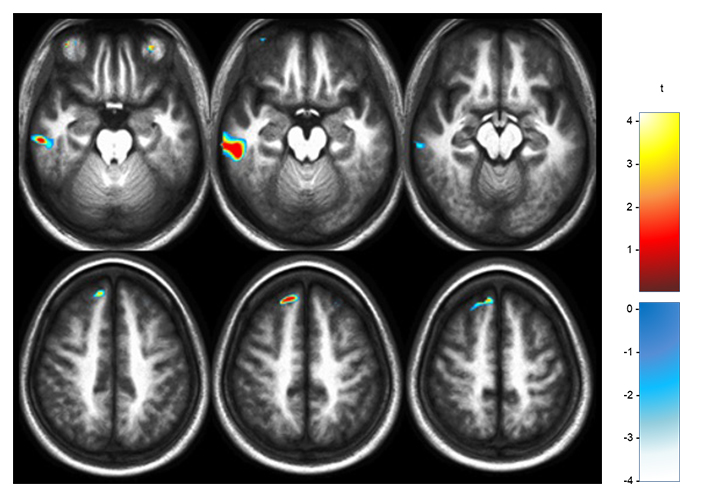
Axial views that showed significant clusters where current smokers with motivation showed greater brain activities than those without motivation. Voxel height threshold at significant of P = 0.05, uncorrected. None of the areas remain significant after multiple comparison correction (adjusted significant threshold at P = 0.001). t: t-test
Regions of the brain in which current smokers without motivation displayed greater brain activities than those with motivation
| Regions* | Brodmann areas | Peak MNI coordinates | ||
|---|---|---|---|---|
| x | y | z | ||
| Left precentral gyrus | 4 | –20 | –22 | 71 |
| Right paracentral lobule | N/A | 7 | –24 | 70 |
| 8 | –26 | 71 | ||
| Left paracentral lobule | N/A | –19 | –25 | 71 |
| –15 | –29 | 79 | ||
* Two sample t-test, P < 0.05 uncorrected. None of the areas remain significant after multiple comparison correction (adjusted significant threshold at P = 0.001). N/A: not applicable
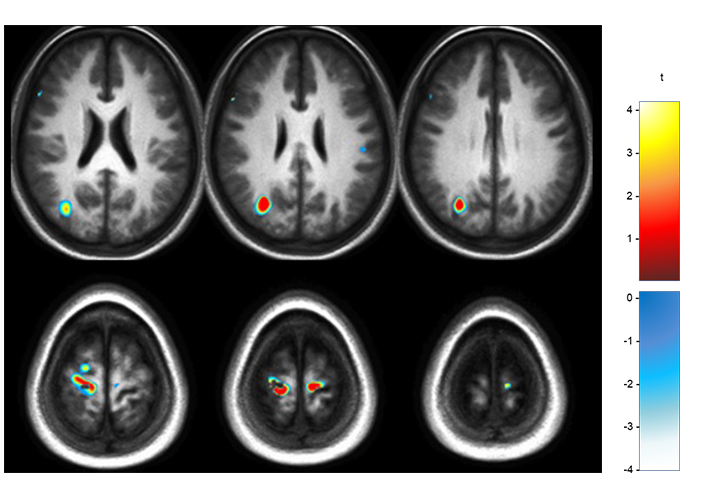
Axial views that showed significant clusters in which current smokers without motivation showed greater brain activities than those with motivation. Voxel height threshold with significance of P < 0.05, uncorrected. None of the areas remain significant after multiple comparison correction (adjusted significant threshold at P = 0.001). t: t-test
To our knowledge, this is the first study to explore the brain functions of motivation to change smoking behaviors. Although the sample size was small due to the nature of the preliminary results, altered brain functions were detected in different areas of the brain between smokers with and without motivation to change. Furthermore, low motivation for change was observed among most smokers who already received health-related services in psychiatric or routine medical check-up services. The only variable found in the study that is related to having more motivation to change among smokers is the higher severity of their dependence on cigarettes or cigarette smoking. However, previous studies found other variables related to less motivation to change, such as younger age [36] and a higher BMI [37].
Smokers from other specific populations, such as minorities [38] or young smokers [39] had little motivation to quit smoking. In this study, most smokers that were in the precontemplation stage had little motivation to change smoking behaviors even though they were receiving health services. Regarding smokers from the psychiatric service, the low motivation to change is consistent with the studies from the Australian mental health inpatients [40], the Canadian acute-care psychiatry units inpatients [41], and the US acute and long-term psychiatric inpatients [42] or patients with psychotic disorder [43] that psychiatric patients had low motivation to quit smoking. The prevalence of smokers in psychiatric patients was high [44], and their mental health could predict the success of smoking cessation [24] or relapse to substance use that led to family, legal, economic, and social problems.
Although most demographics were not different between smokers from the psychiatric service and the routine medical check-up service in the study, smokers with mental illness tended to have lower levels of education than those without, consistent with a previous study [45], as people with mental health problems tended to have more difficulty studying in schools than those without [46]. However, smokers with or without mental illness did not differ in motivation to change smoking behaviors, consistent with previous studies that showed the same pattern of motivation to change between smokers with mental disorders and general healthy smokers [47, 48] that requested the same practices to improve motivation to change among smokers with or without mental disorders.
In contrast, smokers who had medical diseases or health concerns related to smoking were more likely to be in the contemplation stage and had more motivation to quit smoking [17, 45, 49, 50], as well as other substances such as alcohol or other drugs [51]. Additionally, smokers with more severe nicotine dependence, were more likely to have more medical diseases and were more likely to have greater motivation to change. In the previous analysis of the overlapping cohort in the routine check-up service, smokers with poorer health status, older age, and more severe nicotine dependence were associated with greater motivation to change [30]. However, the result is inconsistent with the study of the North Indian population that showed that smokers in the precontemplation or contemplation stage had a higher level of nicotine dependence than those at the preparation stage [52]. Furthermore, a study of substance use disorder among the population receiving treatment showed a negative correlation between nicotine dependence levels and motivation to change [53]. Different populations and motivation measurements could be the reasons for the inconsistencies between the studies that warrant further study.
Greater activation in the left inferior temporal gyrus and superior frontal gyrus when watching smoking signals among smokers with motivation to change than those without is consistent with the study of cue-induced craving for smoking in a virtual environment [54]. Furthermore, greater brain activation was shown in the left middle temporal gyrus and the superior medial gyrus among motivated smokers. These brain regions are associated with information perception [55], self-awareness [56], and executive functions [57] and could help smokers gain more awareness or recognition of their smoking behaviors.
On the contrary, greater activation in the left precentral gyrus and the bilateral paracentral lobule when watching the cigarette signal among smokers without motivation to change is consistent with the study showing the activated precentral gyrus by the smell of cigarettes [58]. This region of the brain could be affected by olfactory and visual signals of cigarettes and more stimulated in smokers without motivation. However, previous studies on motivation to quit other substances such as cocaine showed other areas of the brain, including the frontal, occipital, temporal, and cingulate cortices, were more activated among less motivated participants [59].
Several limitations deserve to be mentioned. First, only 14 subjects underwent the MRI examination, including 4 subjects who were motivated to change smoking behaviors and 10 subjects who were unwilling to change. Because the sample size was too small, the difference between the two groups could not be robust, so that correction for multiple comparisons would increase the threshold of significant level and none of the results remained significant after the multiple testing correction. Second, in addition to the small sample size due to the nature of this being a preliminary study, most of the participants in this study were male and received hospital services, therefore generalizing the results to the general population was limited. Future research should include more women in studies, recruit more participants, and study in other settings than the hospital. Third, participants were asked to stop smoking for at least 1 h before the MRI examination so that they would have withdrawal reactions that would have an effect on brain activity. Lastly, other variables related to smoking behaviors were not controlled in the study. For example, factors that may affect smoking withdrawal behavior and motivations to change of smokers, including participants’ level of physical activity [60, 61], socioeconomic status [62], and stress reduction [16, 63] were not controlled.
The results in this study have highlighted the way to understand motivation to change of smokers and the brain activation of motivation versus non-motivation smokers when watching cigarette cues. The results may be used to develop interventions to help smokers have more motivation to quit smoking regardless of their mental health. Additionally, more research is needed to increase smokers’ internal and external motivation with action mechanisms and strategies based on their brain function related to motivation to change their smoking behaviors.
BMI: body mass index
fMRI: functional magnetic resonance imaging
FTND: Fagerström Test for Nicotine Dependence
MNI: Montreal Neurological Institute
SD: standard deviation
SOCRATES: Stages of Change Readiness and Treatment Eagerness Scale
RK: Conceptualization, Writing—original draft, Writing—review & editing, Supervision. SS: Conceptualization, Investigation, Writing—original draft. AC: Investigation. WS: Investigation, Validation, Supervision. All authors read and approved the submitted version.
The authors declare that they have no conflicts of interest.
The study was approved by the Institutional Review Board of the Chulalongkorn University Faculty of Medicine (No. 273/59). The study was carried out according to the ethical standards laid down in the Declaration of Helsinki of 1964 and its subsequent amendments or comparable ethical standards.
Informed consent to participate in the study was obtained from all participants.
Not applicable.
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
This work was partially supported by the
© The Author(s) 2023.
Copyright: © The Author(s) 2023. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 2862
Download: 19
Times Cited: 0
Jiayi W. Cox ... Lindsay A. Farrer
Elisha M. Wachman ... Huiping Zhang
Richard Sherva ... Lindsay A. Farrer
Rui Fu ... Michael Chaiton
Ketsupar Jirakran ... Rasmon Kalayasiri
Abuelgasim Elrasheed A. Alhassan ... Simon Elliott
