Affiliation:
Postgraduate Program in Rehabilitation Sciences, Institute of Health Sciences, Federal University of Bahia (UFBA), Salvador-Bahia 40170-110, Brazil
Email: pitanga@lognet.com.br
ORCID: https://orcid.org/0000-0002-1033-8684
Explor Immunol. 2024;4:211–217 DOI: https://doi.org/10.37349/ei.2024.00137
Received: July 06, 2023 Accepted: March 11, 2024 Published: April 17, 2024
Academic Editor: Hassane Zouhal, University of Rennes 2, France
The article belongs to the special issue Physical Activity and Immune System in Chronic Diseases : Mechanisms and Insights
Coronavirus disease 2019 (Covid-19) was declared a pandemic by the World Health Organization (WHO) in March 2020, a fact that led many countries to close their borders and enact confinement measures with a consequent reduction in physical activity levels in the world population.
The importance of regular practice of physical activity to strengthen the immune system and its repercussions for cardiovascular diseases, including arterial hypertension, was little studied before the Covid-19 pandemic. The main focus of the studies was to demonstrate the importance of regular exercise to improve health and well-being, as well as for the prevention of cardiometabolic events [1–3].
The first points of view and opinion articles on physical activity and Covid-19 began to be published right at the beginning of the pandemic and they drew attention to the importance of continuing the practice of physical activity during the processes of restricting the movement of people in different environments [4–7]. These documents usually commented on the benefits of physical activity for mental, cardiovascular, and metabolic health, with little attention given to the importance of the immune system in this context.
Next, it was observed that there were already publications on the benefits of physical activity to reduce the worsening of the infectious process, hospitalizations, and mortality from influenza, with the strengthening of the immune system having a preponderant role in these results [8, 9]. In this way, it was assumed that these benefits could be extended to Covid-19, since they were infections with similar viral characteristics [10].
It was only at the end of 2021 that original articles on physical activity and Covid-19 began to be published, and, in addition to the benefits of reducing the worsening of the disease, hospitalizations, and mortality [11, 12], it was also observed that physical activity could prevent infectious processes in communities [13], as well as infection with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus, the precursor of Covid-19 [14, 15].
Thus, in this brief comment, some reflections will be made, against the backdrop of the challenges for likely future pandemics, on the importance of physical activity to strengthen the immune system, preventing not only more serious clinical conditions but also infection by the SARS-CoV-2 virus and what are the repercussions of arterial hypertension in this context.
Initially, the importance of physical activity in preventing more severe clinical conditions was seen in relation to influenza [8, 9] and later in relation to community infections [13]. Only at the end of 2021 that original studies on the association between physical activity and reduction in hospitalizations and mortality from Covid-19 began to be published.
One of the first studies on the subject concluded that maximum exercise capacity is independently and inversely associated with the likelihood of hospitalization due to Covid-19 [16]. Subsequently, Spanish researchers carried out a retrospective cohort study that included patients between 18 and 70 years of age, diagnosed with Covid-19 and hospitalized [17]. As a main result, it was observed that patients with a sedentary lifestyle had an increase in mortality from Covid-19 regardless of other previous risk factors. The authors concluded that a sedentary lifestyle increases the mortality of patients hospitalized with Covid-19.
Specifically in Brazil, in 2021, we published a study entitled “Physical activity and mortality due to Covid-19 in the Brazilian capitals: an ecological analysis” [11], when the existence of an inverse correlation between leisure time physical activity and accumulated deaths, cumulative deaths adjusted for every 100,000 inhabitants and also with the lethality of the disease was demonstrated. In this study, the authors also observed that each 1% increase in the prevalence of physical activity could reflect a reduction of 485 deaths in the Brazilian population. It should be noted that these data were analyzed before the start of the immunization process against Covid-19 in Brazil.
More recently, a retrospective longitudinal study was published, in which approximately 44,000 people were classified as consistently active and consistently physically inactive [12]. The main result found in this study was that patients with Covid-19 classified as consistently inactive had a higher risk of hospitalization, intensive care unit admission, and deaths due to Covid-19, when compared with patients who consistently met physical activity guidelines.
All this information was compiled in a recent systematic review with meta-analysis where all the benefits of regular physical activity to reduce the deleterious effects of the infectious process were demonstrated [15].
It is extremely important to emphasize that physical activity can also reduce the risk of infectious processes. One of the first systematic review studies with meta-analysis that examined the association between habitual physical activity and the risk of infectious diseases demonstrated that a higher level of habitual physical activity is associated with a 31% reduction in the risk of infectious disease acquired in the community, however, in this work, infection by SARS-CoV-2 was not evaluated [13].
Regarding physical activity as a protective factor for SARS-CoV-2 infection, it was also seen in two recent publications [18]. In the first, with data from 125,000 people, randomly selected from the Korean National Health Insurance Service database, the authors observed that higher levels of regular physical activity were associated with a lower risk of infection and mortality from Covid-19, highlighting the importance of maintaining adequate levels of physical activity alongside social distancing amid the Covid-19 pandemic.
Later, another recent study, also retrospective longitudinal, published by Lee et al. [14] (2022), in which approximately 212,000 adults from South Korea participated, demonstrated that adults who engaged in aerobic and muscle-strengthening activities, according to physical activity guidelines, had a lower risk of serious illness and death related to Covid-19, but the most important finding of this study is that those who engaged in aerobic and muscle-strengthening activities had a lower risk of SARS-CoV-2 infection than those engaged in aerobic and muscle-strengthening activities insufficient [14].
In Brazil, in 2022, we published a study with participants from the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil), where we demonstrated that those who remained physically active during follow-up and, in addition, used individual protective measures against Covid-19 had a 43% reduction in risk of SARS-CoV-2 virus infection [19]. Furthermore, it is important to emphasize that coping behavior is a healthy adaptation to protect against the adverse health effects of Covid-19 [20].
Since the beginning of the pandemic, attention has been drawn to the importance of the immune system to prevent the worsening of clinical conditions, hospital admissions, and death from Covid-19, in addition to reducing the possibility of infection with the SARS-CoV-2 virus. The immune system is formed by the innate defense system and the adaptive defense system. The innate defense system is composed of epithelial barriers, phagocytic cells, and natural killer (NK) cells, while the adaptive defense system is mainly composed of “B” lymphocytes, which produce antibodies, and “T” lymphocytes that try to destroy infected cells.
In this way, different researchers have reported that during the conflict between the virus and the immune cells of our body, during the infectious process caused by the new coronavirus, there would be a release of pro-inflammatory cytokines, which, when directed to the lungs, could cause a greater severity of the clinical condition with, many times, the need for more drastic interventions, such as mechanical ventilation [11, 21].
Thus, more physically active individuals could have more adequate defense mechanisms to reduce the inflammatory process caused by the conflict between the virus and the immune cells of our body, through a higher concentration of anti-inflammatory substances, mainly interleukin 10 (IL-10), observed in greater amounts, chronically, in more physically active individuals. Thus, the reduction of the inflammatory process in the lungs could decrease the severity of the patient’s clinical condition, avoiding the use of more drastic interventions. In addition, it was also observed, in physically active individuals, a higher concentration of phagocytic cells, as well as lymphocyte proliferation, that is, a positive immunomodulation [22].
Furthermore, regarding the fact that physical activity also prevents SARS-CoV-2 infection, the mechanisms can be partially attributed to the higher concentration of immune cells, such as T lymphocytes, in addition to the increased strength of the mucosal immune barrier [salivary immunoglobulin A (IgA)] seen in higher concentrations in more physically active individuals [13, 23, 24], as it has the potential to provide greater immunity against different types of viruses and bacteria that enter the human body through the oral cavity and upper airways (Figure 1) [25].
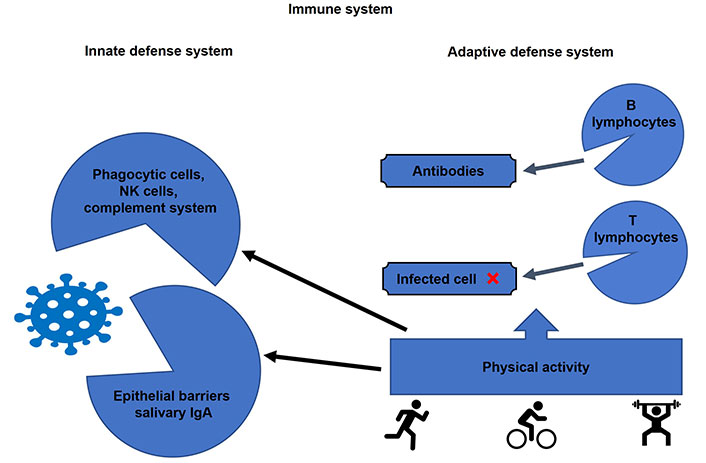
Effect of physical activity on the immune system in preventing the worsening of clinical conditions of Covid-19 and infection by the SARS-CoV-2 virus. The red cross mark indicates that T lymphocytes try to destroy the infected cells
Evidence from the beginning of the pandemic [26], as well as more recent evidence relating to the Omicron variant [27] pointed to angiotensin converting enzyme 2 (ACE2) as an entry receptor for SARS-CoV-2, as well as the main regulator in the balance of the renin angiotensin aldosterone system (RAAS) which regulates blood pressure levels [28].
A recent review article draws attention to many studies, which have already pointed out the importance of host genetic polymorphisms (especially in the RAAS), as well as other related factors such as age, sex, lifestyle, habits, and pathologies or comorbidities (diabetes and cardiovascular diseases) that may provide a greater risk of infection and pathogenicity of Covid-19 [29].
Thus, it can be assumed that in normotensive individuals with adequate functioning of these systems, infection by SARS-CoV-2 could be minimized, even because physical activity can lead to lower circulating levels of ACE2, as seen in a study carried out with 21 young and healthy men submitted to a supervised physical exercise program for 4 weeks, which demonstrated that physical exercise induces the highest expression of ACE2 in skeletal muscle, but leads to lower circulating levels that can potentially reduce the infectious process, such as the pathogenicity of SARS-CoV-2 [30].
It’s very important to mention that in the context of physical activity, not only ACE2 can be associated with infection and hypertension. Physical activity is also associated with levels of histamine, nitric oxide, and general inflammation, which affect blood pressure. Could this be related to SARS-CoV-2 infection too.
The main reflections that remain, based on what we learned from the Covid-19 pandemic, is that the regular practice of physical activity with the respective strengthening of the immune system can be an important strategy to minimize the deleterious effects of future infectious processes that may come to affect humanity. In addition, physical activity has a very positive impact on the prevention of different cardiovascular and metabolic events, such as high blood pressure. The main challenge would be to try to reduce physical inactivity in the world’s population, as we also live with a global pandemic of physical inactivity.
Public policies to promote physical activities more aggressively, with the aim of increasing physical activity levels in the world population, can have a very positive impact so that we are better prepared for future new viral infections with characteristics similar to those of Covid-19.
ACE2: angiotensin converting enzyme 2
Covid-19: coronavirus disease 2019
SARS-CoV-2: severe acute respiratory syndrome coronavirus 2
FP: Conceptualization, Investigation, Writing—original draft, Writing—review & editing.
The author declares that he has no conflicts of interest.
Not applicable.
Not applicable.
Not applicable.
Not applicable.
Not applicable.
© The Author(s) 2024.
Copyright: © The Author(s) 2024. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 2145
Download: 19
Times Cited: 0
Marios Hadjicharalambous ... Nikolaos Zaras
