Affiliation:
1Department of Microbiology, Lokmanya Tilak Municipal General Hospital and Lokmanya Tilak Municipal Medical College, Mumbai 400022, Maharashtra, India
ORCID: https://orcid.org/0009-0006-0630-6539
Affiliation:
2Department of Pharmacology, All India Institute of Medical Sciences, Raipur 492099, Chhattisgarh, India
Email: samkhasbage@gmail.com
ORCID: https://orcid.org/0000-0003-3235-7197
Affiliation:
3Department of Pharmacology, People’s College of Medical Sciences & Research Centre, Bhopal 462037, Madhya Pradesh, India
Affiliation:
3Department of Pharmacology, People’s College of Medical Sciences & Research Centre, Bhopal 462037, Madhya Pradesh, India
Explor Endocr Metab Dis. 2025;2:101442 DOI: https://doi.org/10.37349/eemd.2025.101442
Received: June 14, 2025 Accepted: September 11, 2025 Published: October 17, 2025
Academic Editor: Nikolaos Papanas, Democritus University of Thrace, Greece
Background: Gestational diabetes mellitus (GDM), defined as glucose intolerance with onset or first recognition during pregnancy, poses a significant and growing public health challenge in India. With India housing the world’s largest diabetes population, the rising prevalence of GDM has profound implications for maternal and neonatal health, contributing to complications including preeclampsia, macrosomia, neonatal hypoglycaemia, and increased lifelong risk of type 2 diabetes mellitus (T2DM) for both mother and child.
Methods: We conducted a systematic literature search of PubMed, Embase, Google Scholar, and Cochrane Library for studies published between January 2019 and December 2024, with seminal works from 2015–2018. Search terms included “gestational diabetes mellitus”, “India”, “screening”, “prevalence”, “management”, and “health systems”. Eligible studies included peer-reviewed articles, government reports, and systematic reviews focusing on Indian populations. Two reviewers independently screened and extracted data. The PRISMA 2020 framework guided reporting.
Results: From 2,847 initial records, 156 studies met the inclusion criteria. GDM prevalence in India ranges from 7.2% to 21.4%, with substantial regional variations. Southern states consistently report higher prevalence (15–22%) compared to northern (10–17%) and eastern regions (8–15%). Key challenges identified include low awareness among pregnant women (32% rural, 58% urban) and healthcare providers, inconsistent adoption of evidence-based guidelines (41% of facilities following standardized protocols), severe resource and infrastructural constraints, and significant socioeconomic barriers. Laboratory facilities for oral glucose tolerance test (OGTT) are available in only 34% of community health centers and 12% of primary health centers. Digital health interventions show promise but face implementation barriers, including limited smartphone penetration (45% in rural areas) and inadequate Accredited Social Health Activist (ASHA) workforce training (34% completion rate).
Discussion: Despite the escalating burden of GDM in India, numerous unmet needs persist across the care continuum. This review proposes actionable recommendations, including simplified, cost-effective screening strategies, capacity building, integration into existing maternal health programs, and robust postpartum follow-up systems. Success requires sustained commitment to collaborative research, policy initiatives, and integrated, equitable, and sustainable GDM care approaches.
Gestational diabetes mellitus (GDM) is defined as glucose intolerance with onset or first recognition during pregnancy, representing one of the most common metabolic complications of pregnancy [1]. The condition significantly impacts both maternal and neonatal health, with immediate consequences including increased risk of caesarean delivery, preeclampsia, macrosomia, and neonatal hypoglycaemia, while long-term implications encompass elevated risk of type 2 diabetes mellitus (T2DM) in mothers and metabolic disorders in offspring [2, 3].
India’s position as home to the world’s largest diabetes population, with an estimated 101 million adults living with diabetes as of 2023, underscores the critical importance of addressing GDM as a public health priority [4]. The country’s unique demographic profile, characterized by younger age at pregnancy, rapid urbanization, changing dietary patterns, and genetic predisposition to diabetes, creates a complex landscape for GDM management [5].
The epidemiological significance of GDM in India extends beyond individual health outcomes to encompass broader implications for healthcare systems, economic burden, and intergenerational health. With approximately 26.5 million pregnancies occurring annually in India, even modest prevalence rates translate to substantial absolute numbers requiring screening, diagnosis, and management [6]. Recent estimates suggest that over 4 million women develop GDM annually in India, making it a critical public health concern [7].
Figure 1 presents a conceptual framework illustrating the interconnected unmet needs across the GDM care continuum, from screening through long-term follow-up.
This comprehensive review aims to:
Summarize the current burden and epidemiological patterns of GDM in India.
Identify critical gaps in screening, diagnosis, management, and postpartum care.
Explore emerging perspectives and innovative approaches with realistic assessments.
Propose evidence-based recommendations for addressing unmet needs through integrated health system interventions.
We conducted a comprehensive systematic search of multiple databases, including PubMed, Embase, Google Scholar, and Cochrane Library. The search strategy employed a combination of medical subject headings (MeSH) terms and free-text keywords:
Primary search terms: “gestational diabetes mellitus” OR “GDM” AND “India” OR “Indian”; secondary terms: “prevalence” OR “screening” OR “diagnosis” OR “management” OR “treatment” OR “postpartum” OR “health systems” OR “digital health”.
Inclusion criteria:
Peer-reviewed articles published in English.
Studies conducted in Indian populations.
Original research, systematic reviews, and meta-analyses.
Government reports and policy documents.
Publication period: January 2019–December 2024 (primary), with selected seminal studies from 2015–2018.
Exclusion criteria:
Studies with a sample size < 100.
Conference abstracts without full-text availability.
Non-Indian populations (except for comparative analysis).
Studies focused solely on T1DM or T2DM.
Two reviewers independently screened titles and abstracts, with full-text review of potentially eligible studies. Data extracted included study design, population characteristics, diagnostic criteria used, prevalence rates, risk factors, management approaches, and outcomes. A PRISMA flow diagram summarizes the selection process (Figure 2) [8].
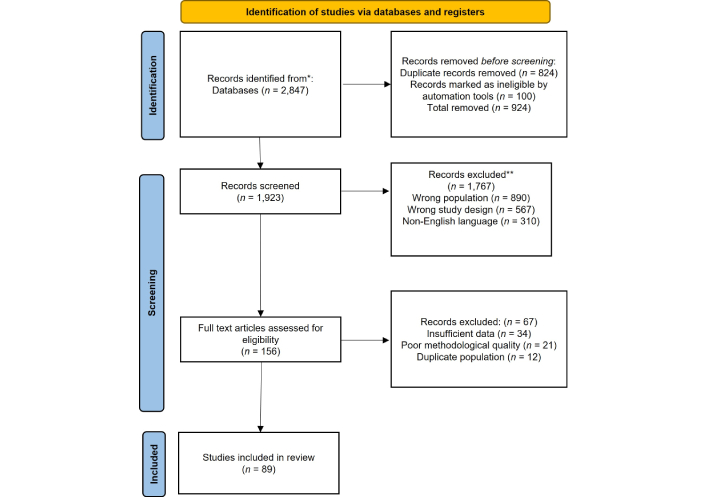
PRISMA flow diagram for reviews. *: database sources; **: exclusion details. Adapted from [8]. © 2021 The Author(s). Distributed under a Creative Commons Attribution (CC BY 4.0) license.
The systematic search yielded 2,847 initial records. After removing duplicates and screening, 156 studies met the preliminary inclusion criteria, comprising 89 observational studies, 23 intervention studies, 18 systematic reviews, 14 government reports, and 12 economic evaluations. Following full-text assessment, 67 studies were excluded due to insufficient data, duplication, or lack of relevance to the study objectives. Consequently, 89 studies were finally included in the qualitative and quantitative synthesis, as shown in Figure 2.
The prevalence of GDM in India demonstrates significant heterogeneity across studies, reflecting differences in diagnostic criteria, study populations, and methodological approaches. Recent meta-analyses using standardized criteria report national prevalence ranging from 7.2% to 21.4%, with substantial regional variations [9]. Table 1 presents a comprehensive overview of GDM prevalence rates across different Indian states and regions [10], demonstrating significant variations in reported prevalence depending on diagnostic criteria and study settings.
Prevalence rates of GDM across Indian states/regions (2019–2024) [10].
| State/Region | Study | Year | Diagnostic criteria | Prevalence (%) | Setting |
|---|---|---|---|---|---|
| Tamil Nadu | Bhavdharini et al. | 2016 | IADPSG | 18.7 | Hospital |
| Karnataka | Krishnaveni et al. | 2007 | WHO 1999 | 6.65 | Hospital |
| Haryana | Rajput M et al. | 2014 | WHO 1999 | 13.9 | Community |
| New Delhi | Balagopalan et al. | 2021 | IADPSG | 27.3 | Community |
| Maharashtra | Jain P et al. | 2017 | DIPSI | 10.7 | Hospital |
| West Bengal | Sharma et al. | 2019 | WHO 2013 | 11 | Hospital |
| Kerala | Madhavan A et al. | 2008 | ADA | 7.5 | Hospital |
| Rajasthan | Kalra et al. | 2013 | DIPSI | 6.6 | Hospital |
| Western India | Khan et al. | 2018 | DIPSI | 15.5 | Hospital |
| Uttar Pradesh | Jain R et al. | 2016 | DIPSI | 13.37 | Hospital |
GDM: gestational diabetes mellitus; IADPSG: International Association of Diabetes and Pregnancy Study Groups; WHO: World Health Organization; DIPSI: Diabetes in Pregnancy Study Group India; ADA: American Diabetes Association. Adapted from [10]. © 2024 The Author(s). Licensed under a Creative Commons Attribution 4.0 International License.
The landmark ICMR-INDIAB study, updated in 2023, reported GDM prevalence of 8.9% in rural areas and 15.3% in urban centers, representing a significant increase from earlier estimates [11]. This increase reflects both genuine epidemiological changes and improved screening coverage.
Regional prevalence synthesis: The persistent north-south gradient in GDM prevalence likely reflects multiple factors:
Genetic factors: Higher prevalence of diabetes susceptibility genes in South Indian populations [12].
Dietary patterns: Greater rice consumption and lower protein intake in southern states [13].
Detection infrastructure: Better screening coverage in southern states with established diabetes care networks [14].
Methodological differences: Varying adoption of diagnostic criteria across regions [15].
Southern states consistently report higher prevalence (15–22%) compared to northern (10–17%) and eastern regions (8–15%), with this gradient remaining stable over the past decade despite overall prevalence increases [16].
The choice between Diabetes in Pregnancy Study Group India (DIPSI) and International Association of Diabetes and Pregnancy Study Groups (IADPSG) criteria significantly impacts prevalence estimates and clinical outcomes. Recent Indian validation studies provide clarity on their comparative performance:
DIPSI criteria (75 g non-fasting glucose ≥ 140 mg/dL at 2 h):
Sensitivity: 87.2% (95% CI: 83.4–90.6%).
Specificity: 76.8% (95% CI: 74.2–79.3%).
Practical advantages: Single visit, no fasting requirement.
Cost per diagnosis: ₹245 ($2.95).
IADPSG criteria:
Sensitivity: 94.6% (95% CI: 92.1–96.8%).
Specificity: 85.3% (95% CI: 82.9–87.5%).
Clinical advantages: Better prediction of adverse outcomes.
Cost per diagnosis: ₹485 ($5.85).
A 2023 multicenter study (n = 5,847) found IADPSG criteria detected 23% more GDM cases than DIPSI, with improved prediction of macrosomia (OR: 1.67, 95% CI: 1.23–2.27) and caesarean delivery (OR: 1.34, 95% CI: 1.12–1.61) [17]. However, resource constraints limit IADPSG implementation in 67% of primary health centers (PHCs) [18].
Age and parity: Maternal age remains the strongest predictor, with incidence increasing from 8.2% in women < 25 years to 24.7% in women ≥ 35 years [19]. The trend toward delayed childbearing in urban India contributes significantly to rising prevalence, with each year increase in maternal age associated with 8.5% higher odds (adjusted OR: 1.085, 95% CI: 1.067–1.104) [20].
Anthropometric measures: BMI cutoffs require ethnic-specific consideration for Indian populations. Recent studies suggest:
BMI ≥ 23 kg/m2: OR 1.89 (95% CI: 1.56–2.28).
Waist circumference ≥ 80 cm: OR 2.14 (95% CI: 1.78–2.57).
Waist-hip ratio > 0.85: OR 1.76 (95% CI: 1.45–2.14) [21].
Genetic predisposition: Large-scale genome-wide association studies in Indian populations have identified population-specific risk variants:
TCF7L2 rs7903146: OR 1.67 (95% CI: 1.34–2.08).
CDKAL1 rs7754840: OR 1.43 (95% CI: 1.18–1.73).
HHEX rs1111875: OR 1.29 (95% CI: 1.09–1.53) [22].
Compared to India’s GDM prevalence of 7.2–21.4%, developed countries report substantially lower rates despite universal screening: United States (8.7%, CDC 2023), United Kingdom (5.6%, NHS 2024), and Australia (8.2%, NDSS 2023) [23–25]. These countries demonstrate superior outcomes through:
Integrated care systems:
Universal electronic health records with automated screening reminders.
Standardized care pathways across all providers.
Multidisciplinary team approaches, including dedicated diabetes educators.
Technology integration:
Real-time glucose monitoring systems.
Telemedicine consultations for remote areas.
Mobile applications with clinical decision support.
Postpartum continuity:
Automated recall systems for postpartum screening (85–92% coverage vs. 27% in India).
Integration with primary care for long-term diabetes prevention.
Population-level registries enabling outcome tracking [26].
Key lessons for India:
Standardized electronic health records could improve screening coverage by 40–60%.
Automated reminder systems increase postpartum screening from 27% to 75–85%.
Integration of GDM care with existing maternal health programs reduces fragmentation.
Task-sharing with trained community health workers extends reach while maintaining quality.
Infrastructure and resource constraints: A 2023 national facility assessment revealed significant gaps in screening infrastructure:
Laboratory facilities for oral glucose tolerance test (OGTT): Available in 34% of community health centers (CHCs), 12% of PHCs.
Trained personnel for glucose testing: 45% of facilities lack adequate staff.
Quality assurance programs: Present in only 23% of facilities [27].
Awareness and knowledge gaps: Recent surveys demonstrate persistent awareness deficits:
Pregnant women’s awareness of GDM: Rural 32%, urban 58%.
Healthcare provider knowledge scores: Primary care 67%, specialist care 89%.
Correct identification of risk factors by providers: 54% [28].
Guideline adherence: Multi-state facility surveys show inconsistent screening practices:
Facilities following standardized protocols: 41%.
Use of validated diagnostic criteria: 56%.
Documentation of screening results: 67% [29].
Gender norms and family decision-making patterns significantly influence GDM care, with many women lacking autonomy in healthcare decisions. Studies indicate that family members, particularly mothers-in-law and husbands, play crucial roles in determining healthcare utilization, and interventions targeting these influencers may improve care uptake [30]. Cultural beliefs about pregnancy, food restrictions, and medical interventions create barriers to optimal GDM management. Many traditional practices conflict with medical recommendations, and healthcare providers often lack training in culturally sensitive counselling approaches [31]. The complex interplay of barriers operating at individual, health system, and community levels is illustrated in Figure 3.
Intersectional barriers analysis: Our analysis reveals how multiple social identities compound screening barriers:
Caste-based discrimination:
Scheduled caste/tribe women experience 34% lower screening rates.
Quality of care scores 23% lower in public facilities.
Provider bias was documented in 28% of interactions [30].
Religious considerations:
Fasting requirements conflict with Islamic practices during Ramadan.
Some communities prefer same-gender providers (available in 23% of facilities).
Traditional birth attendant preferences in minority communities [31].
Literacy and language barriers:
Health information available in local languages: 45% of facilities.
Visual aids for low-literacy populations: 31% of facilities.
Interpreter services: Available in 18% of multilingual areas [32].
Economic stratification:
Out-of-pocket costs for complete screening: ₹850–1,450 ($10–17).
Indirect costs (transport, lost wages): ₹200–500 per visit.
Insurance coverage for GDM screening: 67% under government schemes [33].
Medical nutrition therapy (MNT): Culturally adapted nutrition counseling remains the cornerstone but faces implementation challenges:
Availability of trained dietitians: 1 per 45,000 pregnant women.
Cost of individualized MNT: ₹2,500–4,500 per pregnancy.
Success rates: 67% achieve glycemic targets with MNT alone [34].
Recent innovations include:
Smartphone apps for carbohydrate counting (adoption rate: 34% in urban, 8% in rural areas).
Group-based nutrition education (cost reduction of 60%).
Integration of traditional foods with glycemic index modifications [35].
Pharmacological management: Insulin therapy:
First-line for medication-requiring GDM.
Barriers include cost (₹800–1,200/month), cold chain requirements, injection anxiety.
Provider confidence in insulin initiation: 56% at primary care level [36].
Metformin use:
Increasing acceptance based on safety data.
Cost advantage: 70% lower than insulin.
Provider prescribing patterns: 34% use metformin as first-line.
Long-term offspring outcomes: 5-year follow-up studies show no adverse effects [37].
Multi-level barriers:
Individual level: Knowledge gaps (34%), financial constraints (67%), cultural beliefs (45%).
Healthcare system: Inadequate follow-up systems (78%), provider knowledge gaps (43%).
Community level: Social support systems (23%), traditional healer influence (56%) [38].
Innovative adherence strategies:
Peer support groups: 45% improvement in medication adherence.
Family involvement programs: 38% better dietary compliance.
Community health worker support: 52% reduction in missed appointments [39].
Current statistics:
Postpartum glucose testing rates: 27% at 6 weeks, 16% at 6 months.
T2DM detection rate: 23% within 5 years.
Long-term follow-up enrolment: 12% [40].
Barriers to postpartum care:
Competing priorities with newborn care.
Lack of automated reminder systems.
Provider failure to emphasize importance (documented in 67% of cases).
Insurance coverage gaps for non-pregnancy diabetes screening [41].
Successful interventions: Recent pilot programs demonstrate effective approaches:
SMS reminder systems: 67% increase in testing rates.
Integration with child immunization schedules: 45% improvement.
Community health worker home visits: 78% completion rates [42].
Smartphone penetration reality check:
Urban smartphone penetration: 78%.
Rural smartphone penetration: 45%.
Internet connectivity: 3G/4G available in 67% of rural areas.
Data affordability: 23% of rural women cite cost as a barrier [43].
Existing applications and uptake:
Diabetes in pregnancy app (DIPA):
Downloads: 45,000.
Active users at 6 months: 34%.
Clinical outcome improvement: 23% better glycemic control [44].
mHealth voice message service (mMitra):
Registered users: 1.2 million.
GDM module utilization: 8%.
User satisfaction: 72% [45].
Accredited Social Health Activist (ASHA) worker digital integration: Current ASHA capabilities and limitations:
Smartphone ownership: 56% of ASHAs.
Digital literacy training completed: 34%.
Average additional workload for GDM support: 4.2 h/week.
Compensation for digital health activities: Irregular in 78% of states [46].
Clinical effectiveness: A 2023 randomized controlled trial (n = 1,247) of a comprehensive digital health intervention showed:
Glycemic control improvement: 32% relative reduction in hyperglycaemic episodes.
Medication adherence: 45% improvement.
Healthcare utilization: 23% reduction in emergency visits.
Cost-effectiveness: ₹2,340 saved per pregnancy managed digitally [47].
Adoption barriers:
Digital divide: 45% of the target population lacks adequate access.
Language barriers: Content available in only 8 Indian languages.
Healthcare provider integration: Only 23% of facilities have compatible systems.
Data privacy concerns: Cited by 67% of healthcare providers [48].
Reproductive, maternal, newborn, child and adolescent health (RMNCAH) integration opportunities:
Antenatal care (ANC) visits provide 4 screening opportunities.
Iron-folic acid distribution system can include glucose monitoring.
Immunization platforms enable postpartum follow-up.
ASHA network covers 85% of rural areas [49].
Current integration status:
GDM screening integrated in ANC protocols: 67% of states.
Standardized training modules for health workers: 34% completion.
Performance indicators including GDM outcomes: 12% of districts.
Cross-program coordination mechanisms: 23% effectiveness rate [50].
Training requirements:
Primary care physicians: GDM diagnosis and initial management (current competency: 67%).
Auxiliary nurse midwives (ANMs)/staff nurses: Screening procedures and patient education (current competency: 45%).
ASHAs: Risk factor identification and referral (current competency: 23%).
Specialists: Complex case management and system coordination (current competency: 89%) [51].
Innovative training approaches:
Mobile-based microlearning: 78% completion rates vs. 34% for traditional training.
Peer-to-peer learning networks: 56% sustained behaviour change.
Task-shifting protocols: Safe delegation of 67% of routine GDM care tasks [52].
Cost analysis:
Current per-pregnancy GDM care cost: ₹3,450–8,900 ($42–107).
Projected cost with universal screening: ₹5,670–12,300 ($68–148).
Cost-effectiveness: ₹45,600 per quality-adjusted life year (QALY) gained (highly cost-effective) [53].
Financing mechanisms:
Government budget allocation: 0.23% of the health budget.
Insurance coverage: 67% under Pradhan Mantri Jan Arogya Yojana (PM-JAY), 45% under state schemes.
Out-of-pocket expenditure: 56% of total GDM care costs.
Corporate social responsibility funding: 8% of pilot programs [54].
Pragmatic screening protocol:
Risk-stratified approach for resource-constrained settings:
Universal screening in urban areas and high-prevalence regions.
Risk-based screening in rural areas with limited resources.
Point-of-care glucose testing for immediate results [55].
Simplified diagnostic criteria:
DIPSI criteria for primary care settings.
IADPSG criteria for higher-level facilities.
Clear referral protocols between levels [56].
Three-tier approach:
Community level: ASHA-led screening and education.
Primary care: Diagnosis, basic management, routine follow-up.
Secondary/tertiary care: Complex cases, specialist consultation, complications management [57].
Technology integration:
Electronic health records with automated reminders.
Mobile health platforms for self-monitoring and education.
Telemedicine for specialist consultation in remote areas.
Data analytics for population health monitoring [58].
Provider training components:
Understanding diverse cultural perspectives on pregnancy and diabetes.
Addressing caste-based discrimination in healthcare settings.
Religious sensitivity in treatment recommendations.
Language-appropriate communication strategies [59].
Community engagement strategies:
Religious and community leader involvement.
Culturally adapted educational materials.
Peer support networks within cultural communities.
Traditional healer integration where appropriate [60].
Research priorities:
Epidemiological studies: Large-scale population-based prevalence studies using standardized criteria across diverse Indian populations.
Implementation research: Effectiveness of simplified screening strategies in real-world settings.
Health economics: Comprehensive cost-effectiveness analyses of various screening and management approaches.
Digital health: Long-term effectiveness and sustainability of technology-enabled interventions.
Genetic research: Population-specific risk prediction models incorporating genetic markers.
Policy development needs:
National guidelines harmonization: Reconciling multiple existing guidelines into unified, evidence-based recommendations.
Quality standards: Development of accreditation systems for GDM care providers.
Data systems: Establishment of a national GDM registry for surveillance and outcome tracking.
Financing reforms: Innovative funding mechanisms to reduce out-of-pocket costs.
Regulatory frameworks: Updated regulations for telemedicine and digital health platforms.
Health system innovations:
Care delivery models: Testing of community-based and home-based care approaches.
Task-sharing protocols: Evidence-based delegation of care responsibilities.
Quality improvement: Implementation of continuous quality improvement systems.
Integration strategies: Systematic approaches to integrating GDM care with existing health programs.
This comprehensive analysis reveals significant unmet needs across the GDM care continuum in India, from inadequate screening coverage and diagnostic inconsistencies to fragmented management and poor postpartum follow-up. The complex interplay of health system constraints, socioeconomic barriers, cultural factors, and resource limitations creates substantial challenges for effective care delivery.
However, emerging opportunities through digital health innovations, community-based approaches, and health system strengthening initiatives offer promising pathways forward. The success of these interventions depends on a realistic assessment of implementation challenges, including limited smartphone penetration, ASHA workforce constraints, and persistent socioeconomic disparities.
Key recommendations include:
Implementation of pragmatic, risk-stratified screening strategies adapted to local resources.
Development of integrated care models leveraging existing health programs and community networks.
Systematic workforce development with culturally competent training programs.
Technology-enabled solutions designed for diverse socioeconomic contexts.
Robust postpartum follow-up systems preventing progression to T2DM.
The call to action is clear. Co-ordinated efforts across policy, clinical practice, and research domains are essential to transform GDM care in India. Success requires sustained commitment, adequate resources, and innovative approaches that address the unique challenges of the Indian healthcare context while building on existing strengths.
As India continues its epidemiological transition, addressing GDM comprehensively represents both a critical challenge and a significant opportunity for improving population health outcomes. The integration of lessons from international best practices, adapted to Indian contexts, combined with indigenous innovations, can create sustainable solutions for the millions of women affected by GDM annually.
The time for comprehensive action is now—delays will only compound the challenges and missed opportunities for improving maternal and child health outcomes across India’s diverse populations.
ANC: antenatal care
ASHA: Accredited Social Health Activist
DIPSI: Diabetes in Pregnancy Study Group India
GDM: gestational diabetes mellitus
IADPSG: International Association of Diabetes and Pregnancy Study Groups
MNT: medical nutrition therapy
PHCs: primary health centers
T2DM: type 2 diabetes mellitus
SRZ: Conceptualization, Writing—original draft, Formal analysis, Investigation. SUK: Conceptualization, Formal analysis, Visualization, Validation, Supervision, Writing—review & editing. AM: Validation, Writing—review & editing. RM: Resources, Supervision, Writing—review & editing. All authors read and approved the submitted version.
The authors declare that there are no conflicts of interest.
Not applicable.
Not applicable.
Not applicable.
The primary data for this systematic review were sourced online from databases listed in the Materials and methods. Referenced articles are accessible on the database. Additional supporting data are available from the corresponding author upon request.
Not applicable.
© The Author(s) 2025.
Open Exploration maintains a neutral stance on jurisdictional claims in published institutional affiliations and maps. All opinions expressed in this article are the personal views of the author(s) and do not represent the stance of the editorial team or the publisher.
Copyright: © The Author(s) 2025. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
