Affiliation:
Department of Internal Medicine, Mission Hospital, Asheville, NC 28801, U.S.
Email: David.Notman@mahec.net
ORCID: https://orcid.org/0000-0001-5097-0986
Affiliation:
Department of Internal Medicine, Mission Hospital, Asheville, NC 28801, U.S.
ORCID: https://orcid.org/0000-0001-9938-6991
Affiliation:
Department of Internal Medicine, Mission Hospital, Asheville, NC 28801, U.S.
ORCID: https://orcid.org/0000-0002-7324-8598
Explor Cardiol. 2025;3:101276 DOI: https://doi.org/10.37349/ec.2025.101276
Received: July 26, 2025 Accepted: September 12, 2025 Published: October 15, 2025
Academic Editor: Undurti Das, UND Life Sciences, USA, Sri Ramachandra Medical University, India
A left ventricular pseudoaneurysm typically occurs as a result of myocardial infarction, blunt chest trauma, or cardiac surgery (typically coronary artery bypass grafting or mitral valve replacement). Pseudoaneurysms form due to left ventricular free wall rupture that is contained by the pericardium, not the myocardial wall, as is the case with a true aneurysm. Pseudoaneurysms have the tendency to expand rapidly as opposed to true aneurysms due to the weakness of the pericardium or fibrous tissue in comparison to myocardial tissue. This case presents a 63-year-old male found to have a very large left ventricular pseudoaneurysm measuring 8 × 7 × 5 cm. The vast majority of left ventricular pseudoaneurysms enlarge with worsening symptomatology and eventual rupture if not surgically repaired. Rarely, large pseudoaneurysms treated conservatively can lead to the gradual resolution of a patient’s symptoms and normalization of right ventricular function. The purpose of this case report is to describe the clinical course and outcomes of a patient with a large left ventricular pseudoaneurysm managed conservatively, thereby contributing to the limited medical data regarding the prognosis and long-term outcomes in this high-risk population.
The rates of expansion of large left ventricular pseudoaneurysms have not been widely publicized due to their rarity, the urgency of surgical intervention, and the clinical insignificance of repeat imaging. Pseudoaneurysms are typically diagnosed by transthoracic echocardiogram, cardiac magnetic resonance imaging (CMR), or arteriography. Common symptoms include dyspnea, chest pain, syncope, or back pain. This case demonstrates a highly unique patient presentation of a large pseudoaneurysm, which was managed nonoperatively, resulting in the resolution of chest pain and dyspnea two years later.
A 63-year-old male with a past medical history of heart failure with reduced ejection fraction (HFrEF), coronary artery disease (CAD), hyperlipidemia (HLD), and tobacco use presented to his primary care physician for a routine checkup. For his HLD, the patient has been on a high-intensity statin medication. His guideline-directed medical therapy for his heart failure includes a beta blocker, angiotensin receptor blocker, and mineralocorticoid receptor antagonist. He also takes an as-needed loop diuretic for increasing edema and weight gain. He underwent a low-dose CT scan of the chest due to his history of tobacco use, and his CT demonstrated concern for a left ventricular aneurysm. He was admitted to the hospital following this due to concern for aneurysm rupture and at the time endorsed increased lower extremity edema, mild dyspnea, and intermittent chest pain, which had been occurring for the past year. He described his chest pain as substernal and worse with exertion, occurring on a weekly basis.
On exam, he was found to have mild lower extremity edema with an audible S1 and S2 heart sound. His point of maximal impulse was laterally displaced. A 1/6 holosystolic murmur indicative of tricuspid regurgitation was present on auscultation. His blood pressure was 185/124 mmHg on admission. An electrocardiogram demonstrated normal sinus rhythm with left axis deviation and left ventricular hypertrophy. He was found to have a troponin I of 0.08 ng/mL, which subsequently downtrended, and a pro-B-type natriuretic peptide (pro-BNP) of 8,524 pg/mL. An echocardiogram demonstrated a left ventricular ejection fraction (LVEF) of 10–15% with a large lateral pseudoaneurysm. It also demonstrated severely reduced right ventricular function with mild to moderate right ventricular dilation.
He underwent a right and left heart catheterization, which demonstrated 70% stenosis of his first diagonal vessel, 90% stenosis of his second diagonal vessel, and a second marginal artery, which was fully occluded at its ostium. Finally, a CMR was obtained, which was consistent with a large pseudoaneurysm measuring 8 × 7 × 5 cm containing lateral wall rupture (Figure 1, Figure 2, Figure 3). Within the pseudoaneurysm, a mural thrombus was present, measuring 2 cm in thickness.
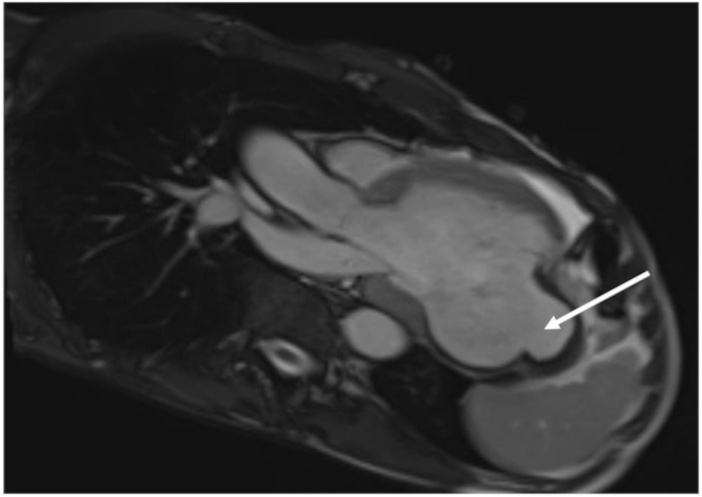
Cardiac MRI three chamber view-vertical long axis. Large left ventricular pseudoaneurysm noted.

Cardiac MRI inversion-recovery sequence-sagittal view. Large left ventricular pseudoaneurysm noted.
Following extensive discussions with the advanced heart failure service and cardiothoracic surgery teams, the patient and family opted for medical management. He was also deemed a very high-risk candidate for any cardiovascular procedure. A left ventricular assist device (LVAD) and percutaneous closure treatment were considered, but the patient and family did not wish to pursue this. Similarly, he deferred consideration for an implantable cardioverter-defibrillator (ICD) secondary to his low ejection fraction. Two years following this patient’s initial echocardiogram, his right ventricle improved in size and function. He had no further chest pain, dyspnea, or leg swelling after about 6 months from his initial diagnosis of his pseudoaneurysm (Table 1). A detail of the timeline events of the patient’s cardiac workup is provided in Figure 4.
Parameter comparison of pseudoaneurysm and ejection fraction over two years.
| Cardiac parameter | Diagnosis | 6 months | 1 year | 2 years |
|---|---|---|---|---|
| LVEF | 10–15% | ~20% | 15–20% | 35–40% |
| RV size/function | Normal size/normal function | Normal size/normal function | Normal size/normal function | Normal size/normal function |
| Pseudoaneurysm dimensions (cm) | 8 × 7 × 5 | - | - | 7 × 7 × 5 |
LVEF: left ventricular ejection fraction; RV: right ventricle.

Timeline of events. CMR: cardiac magnetic resonance imaging; LVAD: left ventricular assist device; LVEF: left ventricular ejection fraction; Pro-BNP: pro-B-type natriuretic peptide.
Left ventricular pseudoaneurysms typically form after a myocardial infarction, trauma, or cardiac surgery, which prompts bleeding into the surrounding pericardium. Symptoms of a left ventricular pseudoaneurysm are variable, with chest pain and dyspnea being most common; however, 12% of patients present with no symptoms [1]. Pseudoaneurysms are distinguished from true aneurysms as they do not have myocardium or endocardium surrounding them, which leads to a higher expansion rate and thus mortality rate. Electrocardiographic changes are seen in most patients but usually consist of nonspecific ST-segment changes, with only 20% of patients showing ST-segment elevation. Physical exam reveals a murmur in about 70% of patients [2]. CMR has been shown to have a sensitivity of 100% in diagnosing left ventricular pseudoaneurysms and is thus widely used after obtaining initial echocardiography [3]. However, cardiac CT and angiography are also routinely used as imaging modalities.
Left ventricular pseudoaneurysms have a risk of rupture of 30 to 45% within one year. It is recommended that medical management be considered in patients who are asymptomatic and who have small-sized pseudoaneurysms under 3 cm [4]. Surgery is the definitive treatment of pseudoaneurysms, however surgical mortality of repair was 20% with a 1-year survival rate following surgery of 73% according to a study done by Atik et al. [5]. When surgical intervention via direct closure or transcatheter closure is not a viable option in pseudoaneurysm repair, medical management follows guidelines similar to those of patients with heart failure (diuretics, angiotensin receptor blockers, SGLT2 inhibitors), arrhythmia control, and anticoagulation if there is superimposed atrial fibrillation/flutter. While the American Heart Association recommends urgent surgical intervention for operative candidates with pseudoaneurysm due to the risk of rupture, observational studies have suggested that in selected patients managed conservatively, the risk of fatal rupture may be low, with most deaths occurring secondary to worsening heart failure or ischemia, rather than hemorrhage [6].
In patients with pseudoaneurysms not amenable to surgical intervention, close monitoring and surveillance are critical. This is often done with echocardiography, CMR, or cardiac CT to assess for changes in the pseudoaneurysm size or morphology. Early identification of pseudoaneurysm rupture is important to reduce the risk of morbidity and mortality. In addition, a multidisciplinary team of cardiothoracic surgeons, electrophysiologists, and advanced heart failure is indispensable to achieving positive results in these nonoperative patients. Treatment approaches are geared towards each patient’s unique physiology and medical history. For example, patients with systemic lupus erythematosus may be at higher risk of wall rupture, such that conservative management may not be appropriate for this group [7].
Left ventricular pseudoaneurysm is a rare phenomenon and requires complex medical decision-making. Patients typically present with dyspnea, chest pain, back pain, syncope, or lower extremity edema. Due to its nature to expand rapidly and prompt worsening symptomatology, urgent surgery is typically indicated. This case reports a patient opting for nonsurgical management of his large left ventricular pseudoaneurysm with full resolution of his clinical symptoms over 2 years following initial diagnosis.
CMR: cardiac magnetic resonance imaging
HLD: hyperlipidemia
LVAD: left ventricular assist device
LVEF: left ventricular ejection fraction
pro-BNP: pro-B-type natriuretic peptide
The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
This research was supported (in whole or in part, non-financial support) by HCA Healthcare and/or an HCA Healthcare affiliated entity.
DN and JV: Conceptualization, Investigation, Writing—original draft. VT: Investigation, Writing—review & editing, Validation, Supervision. All authors read and approved the submitted version.
The authors declare that this research received non-financial support from HCA Healthcare and/or an HCA Healthcare affiliated entity, as acknowledged in the Acknowledgments section. HCA Healthcare is a regulatory organization overseeing Mission Hospital and approximately 200 hospitals across the United States. The authors have no personal, financial, or professional relationships with HCA Healthcare or its affiliated entities beyond the aforementioned non-financial support for this study. No other conflicts of interest are declared.
The study complies with the Declaration of Helsinki (2024 version). Ethical approval for the case report was not required according to the requirements of Mountain Area Health Education Center Ethics and Research Department.
Informed consent to participate in the study was obtained from the participant.
Informed consent to publication was obtained from the participant.
The data for this study could be available from the corresponding author upon reasonable request.
Not applicable.
© The Author(s) 2025.
Open Exploration maintains a neutral stance on jurisdictional claims in published institutional affiliations and maps. All opinions expressed in this article are the personal views of the author(s) and do not represent the stance of the editorial team or the publisher.
Copyright: © The Author(s) 2025. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
