Affiliation:
1St. Paul’s Hospital Millennium Medical College, Addis Ababa 1000, Ethiopia
Email: drbiruknucard@gmail.com
ORCID: https://orcid.org/0009-0006-8285-6233
Affiliation:
2Peoples University of Medical and Health Sciences for Women, Nawabshah 67450, Pakistan
ORCID: https://orcid.org/0009-0008-2568-1697
Affiliation:
1St. Paul’s Hospital Millennium Medical College, Addis Ababa 1000, Ethiopia
ORCID: https://orcid.org/0009-0002-7256-8634
Affiliation:
3School of Medicine, College of Health Sciences, Addis Ababa University, Addis Ababa 1165, Ethiopia
ORCID: https://orcid.org/0009-0000-1366-1228
Affiliation:
1St. Paul’s Hospital Millennium Medical College, Addis Ababa 1000, Ethiopia
ORCID: https://orcid.org/0009-0005-4424-7325
Affiliation:
4Fatima Memorial Hospital, Lahore 54000, Pakistan
ORCID: https://orcid.org/0009-0005-5293-5304
Affiliation:
1St. Paul’s Hospital Millennium Medical College, Addis Ababa 1000, Ethiopia
ORCID: https://orcid.org/0009-0000-1404-8484
Affiliation:
5Bacha Khan Medical College, Mardan 23200, Pakistan
ORCID: https://orcid.org/0009-0003-5613-9650
Affiliation:
6D.G. Khan Medical College, Dera Ghazi Khan 32200, Punjab, Pakistan
ORCID: https://orcid.org/0009-0008-0627-2521
Affiliation:
3School of Medicine, College of Health Sciences, Addis Ababa University, Addis Ababa 1165, Ethiopia
ORCID: https://orcid.org/0000-0003-2387-7027
Affiliation:
7FMH College of Medicine and Dentistry, Lahore 54000, Pakistan
ORCID: https://orcid.org/0009-0004-9579-011X
Affiliation:
8Khairpur Medical College, Khairpur Mirs 66040, Pakistan
Email: Umar60560@gmail.com
ORCID: https://orcid.org/0000-0003-0971-3552
Explor Cardiol. 2025;3:101274 DOI: https://doi.org/10.37349/ec.2025.101274
Received: July 02, 2025 Accepted: August 20, 2025 Published: September 28, 2025
Academic Editor: Tasneem Z. Naqvi, Mayo College of Medicine, United States
Tricuspid valve disorders (TVDs) have historically been underrecognized by clinicians. However, recent years have seen increasing awareness of their clinical impact. This mini-review aims to briefly highlight some questions regarding TVDs, such as Review of tricuspid valve disorders, Decoding its trends, The gender and racial divide, Breaking barriers, Where you live matters, Surgery vs. minimally invasive options, Bridging the gap, and the underappreciated significance of TVDs and why they’re becoming a growing concern in the U.S. There is a significant change in perception of the tricuspid valve—from being the “forgotten valve” to being an important area of focus in cardiology as well as clinical medicine in general. With the aid of advanced imaging methods like echocardiography, CT, and MRI that show a clear and three-dimensional view of the tricuspid valve, there is a better understanding of both the prevalence and diagnostic precision of TVDs. Advancements involving more efficient and optimally timed treatment strategies are also occurring. Although medical and surgical approaches are still in use, developments such as transcatheter tricuspid valve interventions (TTVIs) are promising, particularly for high-risk patients with minimal improvement with surgical treatment. TVDs, especially tricuspid regurgitation, have gained widespread attention in the medical and research community, resulting in improved and evolving diagnostic and therapeutic progress to improve patient outcomes.
Tricuspid valve disorder (TVD), a critical aspect of valvular heart disease (VHD), significantly impacts cardiovascular health and is increasingly recognized as a significant cause of cardiovascular morbidity. TVD has contributed to a noticeable spike in mortality rate in the U.S. with evolving paradigms in classification. Current epidemiological estimates suggest that abnormalities of the tricuspid valve (TV) consist of various congenital and acquired lesions [1–3], but tricuspid regurgitation (TR) and tricuspid stenosis (TS) are the most prevalent. A schematic overview of the major types of TVD is shown in Figure 1. TR is diagnosed more frequently and impacts approximately 1.6 million Americans, with prevalence rising to 4% in individuals over 75 years of age due to aging and comorbidities. TS, although rare, is responsible for less than 1% of VHD in the U.S. [4, 5]. Once referred to as the “forgotten valve” due to relative disinterest compared to left-sided valves, it is now appreciated for its clinical importance, driven by technical advances in diagnosis and treatment modalities [6, 7], which have focused exclusively on inpatient diagnosis [8, 9]. Despite the poor prognosis for untreated TVD, surgical management is routinely considered only at the time of left-sided valve surgery (LSVS), and patients are typically addressed for isolated tricuspid valve surgery (ITVS) mainly in cases of advanced disease with significant right ventricular dysfunction [10, 11]. The treatment modalities for TVDs include both medical and surgical options. Medical therapy is the cornerstone of treatment and involves the use of diuretics to inhibit volume overload and slow the progression of right heart failure [2, 12]. According to the United States National Registry [13], 5,005 primary TV procedures were performed with an in-hospital mortality of 8.8% over 10 years. Surgical intervention consists of either TV repair or replacement. Valve repair is the most advantageous procedure, while valve replacement is preferred in refractory cases where the valve’s structure is severely compromised, as seen in endocarditis, carcinoid syndrome, and radiation injury [14, 15]. The American Heart Association and American College of Cardiology Guideline for the Management of Patients with Valvular Heart Disease recommends isolated TV repair or replacement as a class of recommendation IIa or IIb, both levels of evidence C [16].
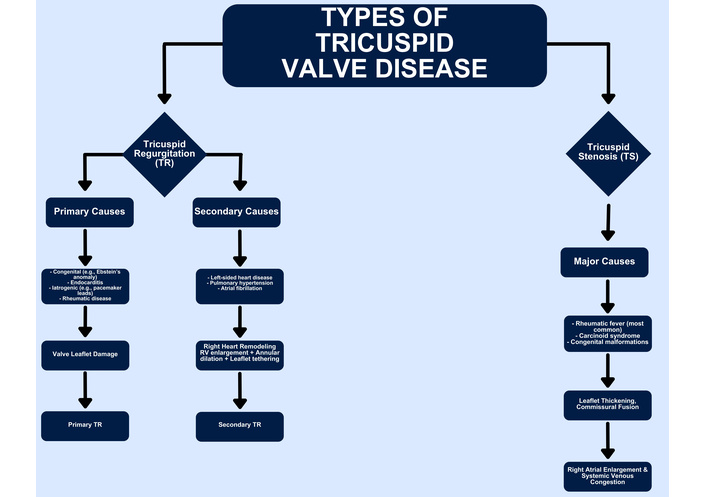
Types of tricuspid valve disorders. TR: tricuspid regurgitation; TS: tricuspid stenosis.
This mini-review aims to synthesize emerging insights into the epidemiology, clinical entities, and recent therapeutic innovations in TVD, with a focus on the U.S. healthcare context. An overview of the classification, pathophysiology, and etiologies of TVD is summarized in Table 1. We highlight disparities in diagnosis and intervention, assess the utility of novel imaging and transcatheter treatments, and examine the evolving guidelines shaping clinical decision-making. In doing so, we underscore why early recognition and personalized treatment of TVD are critical to improving long-term outcomes.
Classification, pathophysiology, and etiology of tricuspid valve disorders.
| Category | Type/Subtype | Description |
|---|---|---|
| Classification | TR | The most common right-sided valvular lesion in adults, physiological trace to mild TR, is often normal [17, 18]. |
| Classification | Primary regurgitation | Caused by intrinsic abnormalities such as congenital defects, infective endocarditis, or rheumatic disease [19]. |
| Classification | Secondary (functional) regurgitation | Due to RV dilation or pulmonary hypertension, which pulls valve leaflets apart, impairing closure [19]. |
| Classification | TS | Thickened or fused leaflets restrict forward blood flow from RA to RV, often caused by rheumatic disease, carcinoid syndrome, or congenital anomalies [2]. |
| Pathophysiology | Annular dilation and leaflet tethering | The TA is more likely to dilate with RV enlargement. Annular dilation and leaflet tethering (from RA/RV dilation) impair coaptation and worsen TR [19–21]. |
| Pathophysiology | Septal annulus dynamics | The septal portion of the TA remains relatively fixed and is less affected by RV dilation, contributing to asymmetric distortion [19–21]. |
| Etiology | Heart failure and left-sided disease | TR usually results from RV dilation caused by pulmonary hypertension, often secondary to left-sided heart disease or lung conditions like emphysema [3]. |
| Etiology | Other causes of TR | Includes trauma, infective endocarditis, rheumatic heart disease, and congenital defects [3]. |
| Etiology | Device-related TR | ICD or pacemaker leads can interfere with leaflet coaptation or cause fibrosis and tethering, leading to TR. Often diagnosed late [22]. |
| Etiology | Role of imaging | Transesophageal echocardiography and 3DE are essential for detection and grading of device-related TR [22]. |
3DE: three-dimensional echocardiography; ICD: implantable cardioverter-defibrillator; RA: right atrium; RV: right ventricle; TA: tricuspid annulus; TR: tricuspid regurgitation; TS: tricuspid stenosis.
TVD has historically been under treatment and has received increasing recognition due to its rising prevalence among all hospitalized patients. A higher incidence of the disease has been observed in women and older age groups. Moreover, the highest AAMR occurred among the Native American populations and residents of states like Oregon, Minnesota, and Vermont, particularly in the west and rural areas. The notable rise in mortality trends between 1999 and 2023 has been associated with the increasing prevalence of diabetes, obesity, and hypertension [1, 2, 5, 8].
There are well-documented differences in gender and race when it comes to the diagnosis, management and results associated with TVDs [23, 24]. TVDs are more frequent in female patients than male patients. Females are often diagnosed at an advanced age and hence are less likely to undergo surgical intervention. Several cross-sectional studies have also indicated that the prevalence of severe TR is more frequent in Black and Hispanic populations. Yet, they undergo far fewer surgical interventions compared to other racial groups [2]. These disparities contribute to worse clinical outcomes, including greater mortality and hospitalization rates in these populations [25]. A recent analysis from the Bronx-Valve Registry by Scotti et al. [25] revealed that Black and Hispanic patients have a higher prevalence of severe TR compared to White patients, yet were significantly less likely to undergo surgical intervention despite similar symptom severity. This under-treatment was associated with increased mortality and hospitalization rates, highlighting persistent healthcare disparities in valvular disease management.
TVDs historically presented challenges due to their diagnostic and therapeutic limitations. TR in older patients, for example, is not often diagnosed promptly, as standard echocardiographic measurements of the TV often downplay TR severity. The advancement of three-dimensional echocardiography (3DE) gives a clearer view of the heart chambers. It can also identify TR severity with better accuracy, without dependence on geometric assumptions [26, 27]. In addition to diagnostics, management of TVD has witnessed an even greater breakthrough, particularly with the development of transcatheter therapies. Surgical TV repair often results in high in-hospital mortality, mostly due to prolonged delay in treatment, but also as a result of post-surgical complications [28, 29]. However, the development of transcatheter TV intervention offers low-risk treatment and is progressively showing favorable outcomes with a marked difference in quality of life [30, 31].
Despite technical advancements and increased clinical use of 3DE, which has significantly enhanced understanding of TV anatomy and regurgitant mechanisms, its practical effectiveness is limited by the need to display volumetric datasets on two-dimensional, flat screens. This can reduce the depth perception required for full spatial appreciation of annular and leaflet geometry. Emerging modalities such as 3D printing of the TV provide promising avenues to overcome this limitation. By enabling tangible exploration of the annular architecture, 3D printed models offer the potential to refine procedural planning and improve patient-specific management strategies [32].
Rheumatic TS is more common in low-income regions, while high-income countries deal more with degenerative TR, demonstrating the significant impact of socioeconomic factors on the etiology of disease [33]. Furthermore, access to novel transcatheter therapies (TriClip and LuX-Valve) is mostly available in specialized centers in high-resource settings, causing disparities in treatment [34, 35].
The evaluation of TVD has evolved significantly with the increasing use of multi-modality imaging, which offers a more comprehensive understanding of anatomical and functional characteristics. Transthoracic and transesophageal echocardiography remain first-line tools, but cardiac CT and cardiac MRI are increasingly employed for annular sizing, leaflet tethering, and right ventricular assessment. This approach enables accurate grading of TR severity, identification of anatomical challenges, and personalization of therapeutic decisions. The EACVI/ESC position paper by Lancellotti et al. [36] highlights that integrated use of 2D/3D echocardiography, CT, and MRI provides additive value in guiding timing and choice of interventions in native valvular disease.
Surgical TV repair or replacement has long been the standard for severe symptomatic TR, but carries high in-hospital mortality—reported as 8.8% in isolated tricuspid procedures over a decade in the U.S. National Registry [13]. Transcatheter tricuspid valve interventions (TTVIs) have emerged as viable alternatives, especially for high-risk surgical candidates. The TRILUMINATE trial demonstrated that edge-to-edge transcatheter repair led to ≥ 1 grade reduction in TR in 87% of patients, with sustained improvements in NYHA functional class and Kansas City Cardiomyopathy Questionnaire scores at 12 months [34]. Similarly, the EVOQUE and LuX-Valve replacement systems have shown favorable early outcomes, though long-term durability data remain limited [35, 37]. Newer minimally invasive surgical techniques have similar outcomes with open surgical techniques while mitigating perioperative morbidity [38]. Direct comparison of transluminal edge-to-edge repair versus beating heart surgery demonstrates nuanced patient-specific factors that are best for individuals [39].
Despite technical advances, ITVS remains high risk. Large registry data show that in-hospital mortality rates for ITVS can approach 8–10%, and major adverse events may occur in approximately 30% of patients with advanced disease [13, 40, 41]. An overview of recent clinical studies comparing surgical and transcatheter tricuspid interventions is provided in Table 2. Importantly, studies indicate that outcomes are more closely related to the severity of TR and the presence of right ventricular dysfunction than to the underlying etiology [42]. These findings highlight the importance of timely referral for intervention before irreversible right heart remodeling occurs [40–42].
Studies showing recent advances in the treatment of tricuspid valve disease.
| Study, year | Study design | Place of study | Sample size (n) | Intervention | outcome | Follow-up duration | |||
|---|---|---|---|---|---|---|---|---|---|
| Sample size (n) | Name of intervention | Previous surgery | Primary | secondary | |||||
| Alnajar et al., 2024 [43] | Retrospective analysis | U.S. | 51 | Replacement(n = 33)Repair(n = 18) | Mini-TVS | Median sternotomy cardiac surgery | In-hospital mortality and overall survival | Complications like stroke, MI, transfusion, and arrhythmias | 17 months |
| Arafat et al., 2024 [44] | Retrospective cohort study | NA | 617 | Isolated TV(n = 63)Concomitant TV(n = 554) | Isolated and concomitant TVS | NA | Overall operative mortality rate, rates of postoperative renal failure, and need for ventilation more than 24 h after surgery | Late outcomes and heart failure rehospitalization | 2009 to 2020 |
| Shimoda et al., 2025 [45] | Medicare fee-for-service 100%, sample inpatient file provided by the Centers for Medicare & Medicaid Services | U.S. | 1,501 | Replacement(n = 610)Repair(n = 891) | Isolated tricuspid replacement versus repair | NA | Early-term (up to 3 years) all-cause mortality | Early-term MACE and heart failure hospitalizations | 18.7 months |
| Altrabsheh et al., 2025 [46] | Retrospective study | U.S. | 298 | 298 | ITVS | Previous surgical intervention Hx | Operative mortality, survival | Late death and 5-year survival | 5.4 years |
| Hahn et al., 2025 [37] | International multicenter randomized controlled trial | 45 centers in the U.S. and Germany | 400 | Transcatheter tricuspid valve replacement(n = 267)Control(n = 133) | Valve replacement | NA | Death from any cause, implantation of a right ventricular assist device or heart transplantation, post-index tricuspid-valve intervention, hospitalization for heart failure, or an improvement of at least 10 points (KCCQ-OS) | NA | 5 years |
ITVS: isolated tricuspid valve surgery; KCCQ-OS: Kansas City Cardiomyopathy Questionnaire-Overall Summary; MACE: major adverse cardiovascular events; MI: myocardial infarction.
Advances in imaging and transcatheter technologies have expanded the therapeutic capabilities of TVDs, but numerous challenges persist. Of special concern, the scarcity of consensual guidelines, anatomical appropriateness heterogeneity criteria, and the lack of well-individualized procedural strategies for morphologically complex valves stand out [47–49].
Differences between U.S. and European recommendations, such as transcatheter approval criteria, timing of intervention, and quantification of TR severity, emphasize the need for consistent, evidence-based recommendations. As a means to further tailor patients and inform future guidelines, additional long-term outcome studies of these novel therapies are necessary [49, 50].
In patients with secondary TR, medical therapy remains the first-line approach aimed at reducing volume overload and alleviating right heart failure symptoms. Diuretics are commonly used to manage congestion, though they do not modify the underlying disease progression. Advanced heart failure therapies, including neurohormonal blockade (ACE inhibitors, ARBs, beta-blockers, aldosterone antagonists), may be beneficial in selected patients with left-sided heart failure contributing to TR. However, no randomized trials have evaluated pharmacologic therapies specifically for TR.
Notably, discrepancies exist between U.S. and European guidelines regarding timing and indications for surgical or transcatheter interventions in TR. The 2020 ACC/AHA guidelines recommend surgical treatment primarily in patients undergoing LSVS with severe TR (Class I) or in selected symptomatic patients with isolated severe TR and right-sided dysfunction (Class IIa). Conversely, the 2021 ESC/EACTS guidelines offer earlier consideration for intervention in patients with progressive TR, even in the absence of left-sided pathology, especially when right ventricular dilation is evident. This divergence reflects regional differences in interpreting evidence and risk thresholds, and underscores the need for individualized treatment planning based on anatomy, etiology, and comorbid burden [49, 50].
TTVIs represent a significant advancement in the management of TVDs, particularly for high-risk surgical candidates. These minimally invasive procedures offer safer alternatives to traditional surgical approaches by reducing perioperative morbidity and mortality while enabling functional improvement and effective reduction of TR. However, several challenges persist. Anatomical and hemodynamic heterogeneity necessitate individualized treatment planning and thorough pre-procedural evaluation. Complications such as valve migration, leaflet tethering, and conduction disturbances highlight the importance of multidisciplinary procedural planning. Furthermore, the long-term durability of TTVIs remains inadequately studied. Integration of TTVIs into comprehensive structural heart programs, along with future randomized controlled trials, is essential to validate their efficacy and inform standardized clinical guidelines [51]. These evolving trends and treatment innovations are summarized in (Figure 2).

Central illustration—Emerging trends and interventions in tricuspid valve disorders.
TVD has emerged from clinical obscurity and has become a significant focus of cardiovascular medicine. Once underappreciated, TR is now recognized as an essential contributor to heart failure and systemic complications. Advances in imaging and transcatheter therapies have opened new avenues for treatment, making TR a more manageable and treatable entity. However, continued research is essential to identify optimal patient selection criteria, address the lack of standardized grading and therapeutic algorithms, and generate high-quality evidence on long-term outcomes of both surgical and transcatheter approaches. Addressing these gaps will support earlier referral, reduce operative risks, and ultimately improve clinical outcomes in patients with TVD. In the upcoming years, a renewed focus on early detection and personalized therapy will be key to improving the prognosis of patients with TVDs.
3DE: three-dimensional echocardiography
ITVS: isolated tricuspid valve surgery
LSVS: left-sided valve surgery
TR: tricuspid regurgitation
TS: tricuspid stenosis
TTVIs: transcatheter tricuspid valve interventions
TV: tricuspid valve
TVDs: tricuspid valve disorders
VHD: valvular heart disease
BDA, FB, HSG, HWN, HTA, WT, YTT, AK, MUA, EHH, IK, and MU: Conceptualization, Writing—original draft, Investigation. All authors critically revised the manuscript for important intellectual content, approved the final version, and agreed to be accountable for all aspects of the work.
The authors declare that they have no competing interests.
Not applicable. This article does not involve any studies with human participants or animals performed by any of the authors.
Not applicable.
Not applicable.
Not applicable. No new datasets were generated or analysed for this review.
The authors received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors for the preparation of this manuscript.
© The Author(s) 2025.
Open Exploration maintains a neutral stance on jurisdictional claims in published institutional affiliations and maps. All opinions expressed in this article are the personal views of the author(s) and do not represent the stance of the editorial team or the publisher.
Copyright: © The Author(s) 2025. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 2104
Download: 103
Times Cited: 0
