Affiliation:
Department of Medicine, Villa Salus Foundation Hospital/IRCCS San Camillo Hospital, 30174 Venice, Italy
Email: faustorigo57@gmail.com
ORCID: https://orcid.org/0000-0001-5919-5306
Affiliation:
Department of Medicine, Villa Salus Foundation Hospital/IRCCS San Camillo Hospital, 30174 Venice, Italy
ORCID: https://orcid.org/0000-0001-8541-9094
Affiliation:
Department of Medicine, Villa Salus Foundation Hospital/IRCCS San Camillo Hospital, 30174 Venice, Italy
Affiliation:
Department of Medicine, Villa Salus Foundation Hospital/IRCCS San Camillo Hospital, 30174 Venice, Italy
ORCID: https://orcid.org/0000-0002-4921-4427
Affiliation:
Department of Medicine, Villa Salus Foundation Hospital/IRCCS San Camillo Hospital, 30174 Venice, Italy
Affiliation:
Department of Medicine, Villa Salus Foundation Hospital/IRCCS San Camillo Hospital, 30174 Venice, Italy
Explor Cardiol. 2023;1:42–48 DOI: https://doi.org/10.37349/ec.2023.00006
Received: March 08, 2023 Accepted: March 29, 2023 Published: August 31, 2023
Academic Editor: Dimitrois Tousoulis, Athens University Medical School, Greece
Aim: Coronary flow velocity (CFV) can be obtained with transthoracic echocardiography (TTE) in the left anterior descending coronary artery (LAD). The physiologic flow velocity gradient across the different segments of LAD has not been established. This study aims to assess the normal values of resting CFV in proximal, mid, and distal LAD.
Methods: In a single center, prospective, observational study design, TTE was attempted on 110 consecutive, asymptomatic middle-aged subjects (age = 55 years, 46% males) with a low likelihood of coronary artery disease (< 5%). Resting CFV in the LAD was assessed with high-end machines, dedicated coronary pre-set, and high-frequency transducers by pulsed-wave Doppler under color-Doppler guidance in the proximal, mid, and distal segments.
Results: The technical success rate for CFV imaging was lowest for the proximal (101/110, 92%), intermediate for mid (106/110, 96%), and highest for the distal segment (108/110, 98%). All 3 segments were interpretable in 101 subjects. CFV was highest in proximal segments (38.6 cm/s ± 3.9 cm/s), intermediate in mid segments (34.3 cm/s ± 6.04 cm/s, P < 0.01 vs. proximal), and lowest in distal segments (28.1 cm/s ± 1.7 cm/s, P < 0.01 vs. proximal and vs. mid).
Conclusions: A resting evaluation of CFV-LAD can be obtained by TTE in the large majority of consecutive subjects referred to the echocardiography laboratory. Feasibility is highest for distal and lowest for proximal-LAD segments. There is a clear physiologic gradient of CFV with decreasing values, of about 10% for each step, going from proximal to mid and distal segments of LAD. When resting CFV is considered, the site of the sampling is important to obtain comparable and physiologically meaningful data.
With last-generation high-end instruments and dedicated coronary pre-sets, coronary flow velocity (CFV) imaging with transthoracic echocardiography (TTE) can be obtained with pulsed-wave Doppler under color-Doppler guidance [1]. TTE is usually combined with vasodilator stress testing to assess coronary flow velocity reserve (CFVR) as the ratio of peak/rest CFV, as recommended by general cardiology guidelines [2, 3]. Recently, emphasis has been placed on absolute values of resting CFV, which may help with phenotyping and risk stratification without need for stress [4]. In presence of angiographically normal coronary arteries, a high resting CFV has been associated with functional coronary microvascular disease, while a low distal with high proximal CFV indicates a proximal significant epicardial coronary artery stenosis, resulting in a pressure drop across the stenosis with a reduction in flow velocity distal to the stenosis [5]. The current study hypothesis was that the different segments of the left anterior descending coronary artery (LAD) have different absolute CFV values. To test this hypothesis, we recruited 110 asymptomatic consecutive healthy subjects with TTE obtained in the 3 segments of proximal, mid, and distal LAD.
The initial population comprised 110 asymptomatic consecutive healthy subjects prospectively enrolled by a single center from August 1st to November 30th, 2022, as a part of a screening program funded by a local charity (Ifis Bank, Venice-Italy) for the early detection of heart disease. Indication for TTE was routine screening in asymptomatic subjects with a very low pre-test probability of coronary artery disease (< 5% based on European society of cardiology guidelines in chronic coronary syndromes) [2]. Exclusion criteria were significant valvular or congenital heart disease, and prognostically relevant non-cardiac diseases (cancer, end-stage renal disease, or severe obstructive pulmonary disease). The main clinical, bio-humoral, and resting TTE characteristics of the initial study population are shown in Table 1.
Clinical characteristics of the patients
| Population analysis | All patients (n = 110) | Feasible CFV (n = 101) | Non feasible CFV (n = 9) | P-value |
|---|---|---|---|---|
| Age (years) | 56 ± 8 | 57 ± 7 | 52 ± 19 | NS |
| Male sex, n (%) | 39 (35%) | 33 (33%) | 6 (67%) | NS |
| Diabetes, n (%) | 4 (3.6%) | 2 (2%) | 2 (23%) | NS |
| Hypertension, n (%) | 26 (24%) | 22 (22%) | 4 (45%) | NS |
| High cholesterol, n (%) | 58 (52%) | 53 (53%) | 5 (56%) | NS |
| Smoking, n (%) | 54 (49%) | 49 (49%) | 5 (56%) | NS |
| BMI (kg/m2) | 25.7 ± 3.8 | 25.3 ± 3.7 | 27.1 ± 5.0 | NS |
| SBP (mmHg) | 121 ± 17 | 120 ± 16 | 132 ± 24 | 0.049 |
| DBP (mmHg) | 77 ± 11 | 76 ± 10 | 84 ± 16 | 0.03 |
| HR (bpm) | 72 ± 13 | 71 ± 14 | 81 ± 13 | NS (0.06) |
| LV EF (%) | 61 ± 3 | 62 ± 3 | 58 ± 4 | NS (0.08) |
BMI: body mass index; DBP: diastolic blood pressure; HR: heart rate; LV EF: left ventricular ejection fraction; NS: not significant; SBP: sistolic blood pressure
All subjects underwent TTE including the attempt to image resting CFV with an assessment of CFV of proximal-LAD, mid-LAD, and distal-LAD, without adding ultrasound contrast agent to avoid introducing artifact signals that could give a false increase of CFV (Figure S1, Movie S1).
The study protocol was reviewed and approved by the institutional ethics committee (June 29th, 2021, ULSS3 Serenissima Regione Veneto, prot. 05–08). Written informed consent was obtained from all subjects.
All subjects underwent comprehensive TTE at rest. All measurements were taken by a certified cardiologist according to the recommendations of the American Society of Echocardiography and the European Association of Cardiovascular Imaging [6]. Pulsed-Doppler assessment of rest CFV was defined as the basal peak diastolic CFV in the 3 different LAD segments [7]. For this purpose, we used a commercial Vivid E95 General Electric (GE) echo-machine with a dedicated software: a probe delivery frequency from 3.5–8 MHz with 2nd harmonic, a low color Doppler pulse repetition frequency (PRF, 20–30 cm/s), and high wall filters (frequency about 2.8–3 MHz, power about 0 dB and gain –2 dB), high pulse wave (PW) filters, focus on and a large sample PW volume (5–10 mm), that allows to avoid the potential angle error in resting condition as well as during CFVR assessment.
As previously described in detail [8], proximal-LAD was imaged from a modified parasternal long-axis view or using a modified apical 5-chamber view (traversing anterior wall of the heart) within the area lateral to the sinus of Valsalva, with the left atrial appendage and pulmonary artery representing the key reference points (Figure S2, Movie S1).
Mid-LAD is best imaged by placing the transducer in a low parasternal position. The interventricular groove is located in a short-axis view and then the transducer is either tilted towards the base of the heart or rotated to obtain a modified long-axis view (aligned parallel to the groove and to the pulmonary artery). In case of high acoustic thorax impedance, we imaged it starting from a para-apical approach in a sort of modified 5 chambers in order to focus on proximal-LAD parallel to the aortic root (Figure S3, Movie S1).
Distal-LAD tract can be highlighted from the apical window by investigating the lower part of the interventricular anterior sulcus near the apex under color Doppler guidance and adopting higher emitting frequencies (5–7 MHz in 2nd harmonic) (Figure S4, Movie S1).
All frames and clips were digitally recorded for offline analysis, which was performed by an expert specialist, blind to clinical or echocardiographic data.
Statistical analysis: Continuous variables are expressed as mean ± 1 standard deviation. X2 test or fisher exact test was used to compare the distribution of categorical variables among groups. Differences between groups (feasible vs. non-feasible CFV) were tested with a student’s t-test for unpaired values. Multiple group comparisons (proximal-LAD vs. mid-LAD vs. distal-LAD) were assessed by analysis of variance with subgroup analysis by Student-Neumann-Keuls test. All analyses were two-sided. Statistical significance was set at P < 0.05. All statistical calculations were performed using SPSS for windows, release 20.0 (Chicago, Illinois).
The technical success rate for CFV imaging was lowest for the proximal (101/110, 92%), intermediate for mid (104/110, 95%), and highest for the distal-LAD segment (106/110, 96%). All 3 segments were interpretable in 101 subjects (Group 1), while at least 1 segment was uninterpretable in 9 subjects (Group 2). Subjects with uninterpretable CFV in at least 1 segment showed a trend to higher body mass index (Group 1 = 25.4 kg/m2 ± 3.7 kg/m2 vs. Group 2 = 27.1 kg/m2 ± 5.0 kg/m2, P = 0.2) and a faster resting heart rate (Group 1 = 71.7 bpm ± 14.1 bpm vs. Group 2 = 81.1 bpm ± 13.3 bpm, P = 0.06) (Table 1).
The final study population consisted of 101 subjects (age = 56 years ± 11 years, 47 males) with all 3 segments interpretable. CFV was highest in proximal-LAD (39 cm/s ± 4 cm/s), intermediate in mid-LAD (34 cm/s ± 6 cm/s, P < 0.01 vs. proximal-LAD), and lowest in distal-LAD segments (28 cm/s ± 2 cm/s, P < 0.01 vs. proximal-LAD and vs. mid-LAD) (Figure 1).
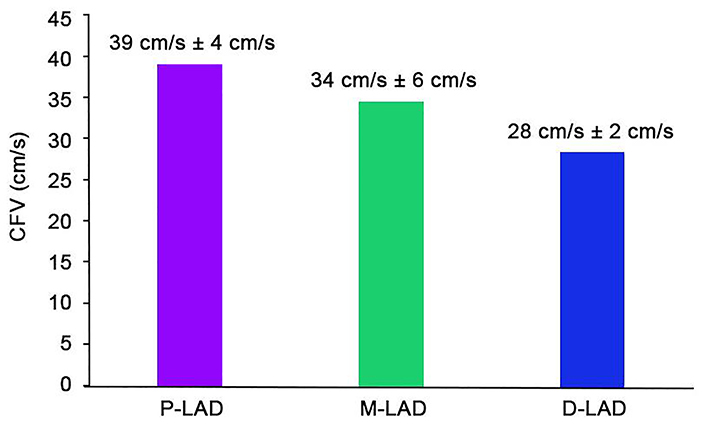
CFV (mean and standard deviation) in distal, mid, and distal segments of LAD. All intergroup differences are significant. P-LAD: proximal-left anterior descending coronary artery; M-LAD: mid-left anterior descending coronary artery; D-LAD: distal-left anterior descending coronary artery
In this study, we used TTE to assess resting CFV in different segments of LAD in asymptomatic, healthy subjects. We demonstrate that: 1. CFV at rest can be assessed in the large majority of subjects consecutively referred to the echocardiography laboratory, with no need for ultrasound-enhancing agents; 2. the success rate is highest for distal-LAD, intermediate for mid-LAD, and lowest although still > 90% for proximal-LAD segments; 3. absolute values of CFV are significantly higher in proximal-LAD compared to mid-LAD and distal-LAD segments. A decrease of about 10% in CFV values occurs at each step. Care should be taken in the harmonization and standardization of sampling sites when absolute resting CFV values are compared in different subjects.
General cardiology guidelines recently endorsed the usefulness of assessing CFVR in patients with CAD or angiographically normal coronary arteries to identify the coronary microvascular disease and refine risk stratification [2, 3]. When CFVR is used, the sampling site is not an issue, and the proximal site with TEE or mid and distal sites with TTE can be used interchangeably. CFVR is a ratio, and the final result averages out the multiple potential sources of error, such as the location of the sampling site or the angle of insonation. However, recently emphasis was placed on the importance of resting CFV in presence of angiographically normal coronary arteries, since a high value may identify a worse prognosis, possibly due to myocardial-coronary mismatch for excessive myocardial oxygen demand, or primary coronary small vessel autoregulatory defect [9]. This situation is different from the pattern of a high proximal- flow with reduced distal-LAD flow, which is a specific sign of proximal-LAD stenosis and requires a mapping of all sites [10, 11]. Another important issue suggests the importance of mapping preliminarily the three different sites of LAD. High-velocity in proximal-LAD (CFV > 50 cm/s) but with a normal decrease up to the distal-LAD highlights high-pressure driving without flow-limiting obstacles in the epicardial coronaries. On the contrary, high-velocity in mid-LAD (CFV > 45 cm/s) or in distal-LAD (CFV > 40 cm/s) with a normal CFV upstream, means a flow-limiting situation is present, such as atherosclerotic plaque or a myocardial bridge over a coronary tract, both situations worthy of further diagnostic investigation such as functional testing or anatomical evaluations with coronary angiography [12].
Our data are in agreement with previous studies showing the high success rate of LAD flow imaging with state-of-the-art technology, with a success rate consistently above 90%, especially when distal-LAD is the target [1–5]. In fact, distal-LAD is closer to the transducer, with less intervening soft and lung tissues, and higher ultrasound frequencies with better spatial resolution can be used. Our data are also consistent with higher values reported for proximal-LAD compared to mid- and distal-LAD in several previous studies. Hozumi et al. [13], in their pioneering study with TTE found a mean value of 22.9 cm/s in distal-LAD of 24 patients without coronary artery stenosis. With TEE, Iliceto et al. [14], reported a mean value of peak diastolic velocity of 35 cm/s in proximal-LAD in normal. Subsequent experiences with TTE and TEE have fully confirmed these initial experiences [15]. Large body mass index and faster heart rate do not preclude technically satisfactory imaging, although image quality is higher with relatively lower heart rates [16].
Studies on resting CFV should always standardize and harmonize the sampling site. In subjects with normal coronary arteries, the distal-LAD is the recommended sampling site since it is the most feasible. CFV in distal-LAD shows the lowest absolute values. The heterogeneity of sampling sites is acceptable for measuring CFVR, but attention to location can make a difference when the absolute values of CFV are considered.
This study has the inherent limitation of a single-site, observational study design. However, all exams were performed by the same experienced observer, with the same machine, with a specific dedicated echo-setting machine, minimizing the known sources of variability due to operator dependence and machine quality. Different coronary segments are imaged by different projections, and this may affect the angle of insonation and therefore absolute values of CFV, which are highest when sample volume is parallel (zero degrees angle) with the flow direction. However, by using a large sample volume for pulsed Doppler assessment, the potential angle error is really minimized and only in a rare case, only in 2 subjects with the highest acoustic impedance, the angle correction was used, and in those cases the difference, in terms of maximum early diastolic peak CFV, was very low about 2–3 cm/s, and therefore scarcely relevant.
Resting CFV can be obtained in almost all subjects referred for TTE. Resting CFV can help in phenotyping and risk stratification for patients in chronic coronary syndromes and possibly other conditions beyond coronary artery disease [17], but the methodology needs standardization and harmonization since absolute values are highest for proximal-LAD and lowest for distal-LAD in healthy subjects. For future studies, the site of sampling should be standardized, studies pooling proximal-LAD, mid-LAD, and distal-LAD values are not advised, and distal sampling is recommended.
CFV: coronary flow velocity
CFVR: coronary flow velocity reserve
LAD: left anterior descending coronary artery
TTE: transthoracic echocardiography
The supplementary Figures for this article are available at: https://www.explorationpub.com/uploads/Article/file/10126_sup_1.pdf. The supplementary movie for this article is available at: https://www.explorationpub.com/uploads/Article/file/10126_sup_2.mp4.
FR: Conceptualization, Investigation, Writing—original draft, Writing—review & editing, Supervision. VS, RSF, PR, CC, and MA: Conceptualization, Investigation, Writing—original draft, Writing—review & editing. All authors read and approved the submitted version.
The authors declare that they have no conflicts of interest.
The study has been approved on June 29, 2021, by Ethical Committee ULSS3 Serenissima Regione Veneto, prot. 05–08.
Informed consent to participate in the study was obtained from all participants.
Informed consent to publication was obtained from relevant participants.
The raw data supporting the conclusions of this manuscript will be made available by the authors, without undue reservation, to any qualified researcher.
The study was funded by un unrestricted grant of Banca Ifis Venezia-Mestre [01-2023]. The funders had no role in study design, data collection, analysis, the decision to publish, or preparation of the manuscript.
© The Authors 2023.
Copyright: © The Author(s) 2023. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
