4 results in Exploration of Cardiology
Latest
Sort by :
- Latest
- Most Viewed
- Most Downloaded
- Most Cited
Open Access
Protocol
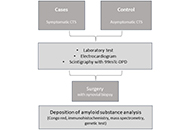
Systemic transthyretin amyloidosis: carpal tunnel syndrome in a Portuguese population (CarPoS)
Sofia Pimenta ... Elisabete Martins
Published: October 24, 2024 Explor Cardiol. 2024;2:217–223
Open Access
Original Article
Echocardiographic findings and subsequent risk of native valve endocarditis
Juan A. Quintero-Martinez ... Larry M. Baddour
Published: September 24, 2024 Explor Cardiol. 2024;2:204–216

Open Access
Case Report
Enhancing patient care: a multimodality strategy for dilated cardiomyopathy in Chagas disease
Luigy Vasquez-Yeng ... Nilda Espinola-Zavaleta
Published: September 22, 2024 Explor Cardiol. 2024;2:196–203

Open Access
Review
Valve-in-valve transcatheter aortic valve replacement: state of art
Marco Fabio Costantino ... Luisiana Stolfi
Published: August 16, 2024 Explor Cardiol. 2024;2:183–195

Journal Information