Affiliation:
1Cardiology Department, Hospital Santa Casa de Misericórdia de Vitória, Vitória 29025023, Brasil
Email: roberto.cardio@gmail.com
ORCID: https://orcid.org/0000-0002-6359-2678
Affiliation:
1Cardiology Department, Hospital Santa Casa de Misericórdia de Vitória, Vitória 29025023, Brasil
ORCID: https://orcid.org/0009-0004-8445-863X
Affiliation:
2Cardiology Department, Instituto Dante Pazzanese de cardiologia, São Paulo 04012180, Brasil
ORCID: https://orcid.org/0000-0001-9879-7756
Affiliation:
3Faculdade Multivix, Vitória 29056080, Brasil
ORCID: https://orcid.org/0009-0004-8368-6593
Affiliation:
1Cardiology Department, Hospital Santa Casa de Misericórdia de Vitória, Vitória 29025023, Brasil
ORCID: https://orcid.org/0009-0002-8097-4368
Affiliation:
1Cardiology Department, Hospital Santa Casa de Misericórdia de Vitória, Vitória 29025023, Brasil
ORCID: https://orcid.org/0009-0008-3923-8856
Affiliation:
1Cardiology Department, Hospital Santa Casa de Misericórdia de Vitória, Vitória 29025023, Brasil
ORCID: https://orcid.org/0009-0003-1831-1747
Affiliation:
1Cardiology Department, Hospital Santa Casa de Misericórdia de Vitória, Vitória 29025023, Brasil
ORCID: https://orcid.org/0000-0002-0978-3377
Affiliation:
1Cardiology Department, Hospital Santa Casa de Misericórdia de Vitória, Vitória 29025023, Brasil
ORCID: https://orcid.org/0000-0002-1903-4599
Affiliation:
1Cardiology Department, Hospital Santa Casa de Misericórdia de Vitória, Vitória 29025023, Brasil
ORCID: https://orcid.org/0000-0002-1092-8190
Explor Cardiol. 2026;4:101296 DOI: https://doi.org/10.37349/ec.2026.101296
Received: September 08, 2025 Accepted: January 26, 2026 Published: February 12, 2026
Academic Editor: Alex Lee, The Chinese University of Hong Kong, China
The Gerbode defect is characterized by a high ventricular septal defect associated with a defect in the septal leaflet of the tricuspid valve, allowing blood to enter the right atrium from the left ventricle. It accounts for approximately 0.08% of intracardiac shunts and may be congenital or acquired. We describe a rare case of Gerbode defect secondary to tricuspid valve endocarditis. A 58-year-old male patient presented with acute infective endocarditis due to Staphylococcus aureus, related to central venous access. Echocardiography showed a tricuspid valve with thickened leaflets and a small mobile image on the atrial side of the septal leaflet, as well as moderate to severe regurgitation. After completion of the antibiotic regimen with resolution of the infectious condition, the patient was discharged asymptomatic, and a new echocardiogram showed no vegetation on the tricuspid valve. During outpatient follow-up, he presented dyspnea on mild exertion, and consecutive echocardiograms showed moderate tricuspid insufficiency and significant pulmonary hypertension with a pulmonary artery systolic pressure of 83 mmHg (reference: 30 mmHg). He underwent right and left cardiac catheterization, which showed a Gerbode defect, and a transesophageal echocardiogram showed a shunt in the subaortic region measuring 6 to 8 mm, with a maximum gradient of 56 mmHg. He underwent elective surgery to correct the Gerbode defect and tricuspid valve repair, with a good clinical result. The Gerbode defect is rare, and the diagnosis can be challenging because it simulates other conditions. Treatment consists of closing the defect when it generates refractory symptoms or complications. The reported case was surgically corrected, with a good result and favorable evolution.
The Gerbode defect is a rare communication between the left ventricle (LV) and the right atrium (RA). It represents only 0.08% of intracardiac shunts and < 1% of all congenital heart defects [1]. Congenital LV-RA communication was first described in 1838 [2]. In 1958, Gerbode et al. [3] described the clinical features and successful surgical repair of five cases of LV-RA communication, characterized by a high ventricular septal defect associated with a defect in the tricuspid valve septal leaflet allowing blood to enter the RA from the LV. A review by Yuan [4] showed that congenital etiology represents 26.4% of cases and acquired etiology represents 72.7%. Among the acquired causes, the following stand out: postoperative cardiac surgery, infection, ischemic, iatrogenic, and traumatic.
We report an unusual case of Gerbode defect secondary to tricuspid valve endocarditis (Figure 1).
A 58-year-old male with systemic arterial hypertension, diabetes, diabetic retinopathy, dyslipidemia, and obesity, a non-user of illicit drugs, had a prolonged hospitalization for treatment of pulmonary tuberculosis in 2018 and, after that, had several hospitalizations for sepsis of pulmonary focus. In one of them, in 2019, he developed acute infective endocarditis due to multi-sensitive Staphylococcus aureus, related to a central venous catheter. At that time, a transthoracic echocardiogram showed a tricuspid valve with thickened leaflets and a small, mobile, hyperechoic, homogeneous mass on the atrial side of the septal leaflet measuring 4.6 cm, and moderate to severe insufficiency. Left ventricular ejection fraction was 46%, and the estimated pulmonary artery systolic pressure was 59 mmHg.
After resolution of the infectious condition with medical treatment, the patient was discharged asymptomatic and with complete resolution of the tricuspid vegetation image. During outpatient follow-up, he presented dyspnea on mild exertion, and consecutive echocardiograms demonstrated moderate tricuspid insufficiency, dilation of the right chambers, moderate dilation of the left atrium (LA), and severe pulmonary hypertension (pulmonary artery systolic pressure 83 mmHg). He was on regular use of losartan, amlodipine, hydrochlorothiazide, furosemide, metoprolol succinate, spironolactone, atorvastatin, metformin, and empagliflozin.
A transesophageal echocardiogram was performed, which demonstrated a 74% LV ejection fraction, enlargement of the right cavities and LA, communication between the LV (subaortic region) and the RA of 6 to 8 mm with a maximum gradient of 56 mmHg, left-to-right shunt (Figure 2), in addition to moderate tricuspid regurgitation and estimated pulmonary artery systolic pressure of 50 mmHg.
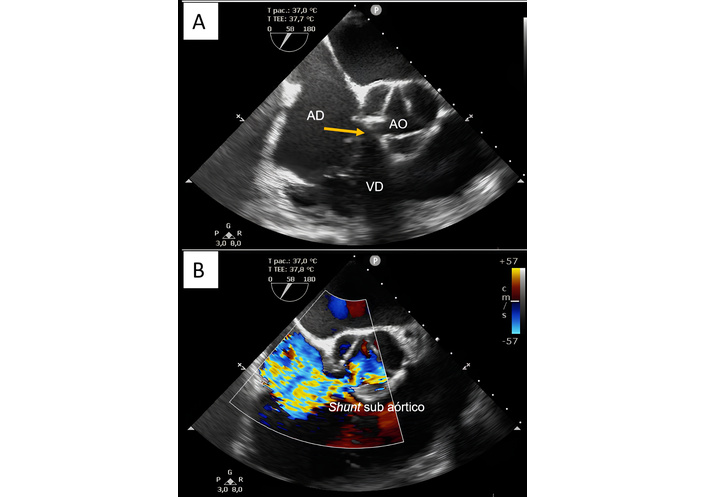
Transesophageal echocardiogram without (A) and with color doppler (B) showing enlargement of the right atrium, communication between the left ventricle (subaortic region) and the right atrium of 6 to 8 mm with a maximum gradient of 56 mmHg. In (A), the yellow arrow indicates the Gerbode defect (AO: aorta; AD: right atrium; VD: right ventricle); in (B), the left-to-right subaortic shunt is observed from the pulsed Doppler.
To evaluate suspected pulmonary arterial hypertension, the patient underwent both right and left heart catheterization. The findings revealed mild pulmonary hypertension, with a pulmonary artery systolic pressure of 42 mmHg (reference: 15–35 mmHg), right ventricular (RV) enlargement, and increased left ventricular end-diastolic volume. Additionally, contrast passage from the LV to the RA was observed, consistent with a Gerbode shunt. No angiographic evidence of pulmonary embolism. The right coronary artery had 30% stenosis.
The defect was surgically repaired by thoracotomy, and a communication orifice of approximately 1.5 cm was visualized intraoperatively, below the septal cusp of the tricuspid valve, with this cusp divided in half (Figure 3). The septal defect was closed with a bovine pericardial patch (Figure 4), and the leaflet was reconstructed, without perioperative complications.
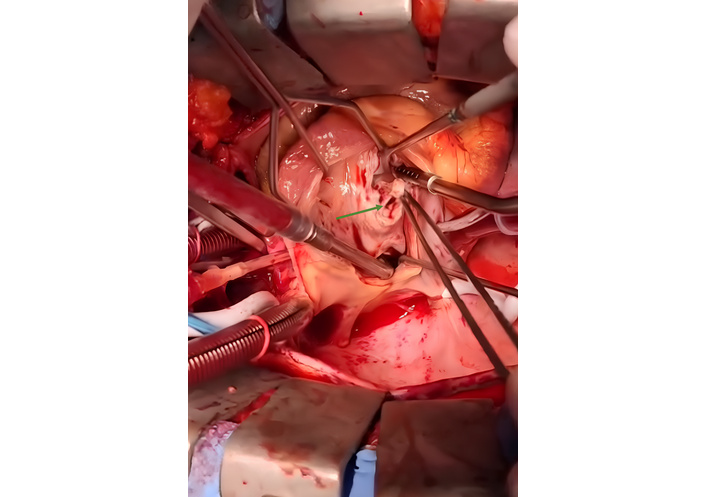
Intraoperative view of the Gerbode defect. A view from the left ventricle showing the communication between this chamber and the right atrium (green arrow).
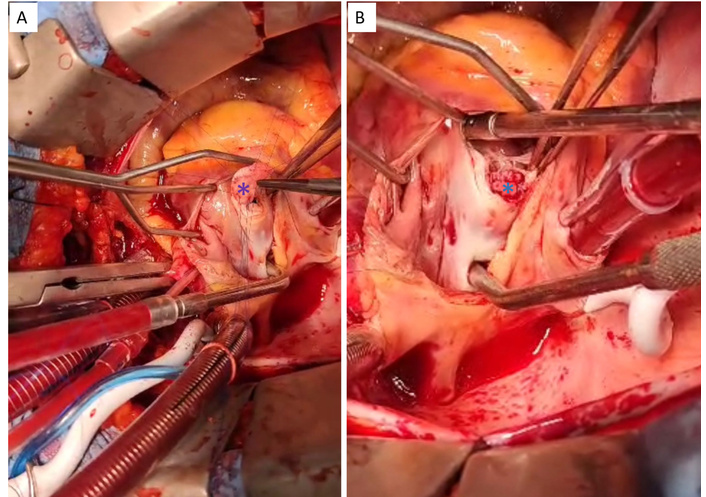
Repair of the septal defect with a bovine pericardial patch. (A) Suture threads passed through the bovine pericardium patch on the Gerbode defect (purple asterisk). (B) Complete surgical occlusion of the Gerbode defect using bovine pericardium patch closure with sutures (blue asterisk).
The patient had a good clinical progress and was discharged from the hospital after 10 days. During outpatient follow-up, he reported improvement in the symptoms of dyspnea.
The Gerbode defect is rare, and its incidence has been increasing with the development of modern cardiac intervention techniques [4]. The classification of the defect depends on its anatomical relationships. In 1967, Riemenschneider and Moss [5] classified the Gerbode defect into two types: direct (or true) and indirect (or false). The direct type is a direct shunt between the LV and RA through the membranous septum, while the indirect type is an intraventricular communication with a left-to-right shunt at the ventricular level associated with tricuspid regurgitation, with the high-speed shunt directed to the RA [2, 4].
A subclassification categorizes indirect defects according to their location. Supravalvular defects involve the atrioventricular membranous septum and occur just above the insertion of the septal leaflet of the tricuspid valve. Infravalvular defects are the most common type and occur in the intraventricular membranous septum. This type is always associated with a malformation in the septal leaflet of the tricuspid valve. These defects include perforation, cleft, or widened commissures. The third and rarest type is the combined supravalvular and infravalvular defect [5]. In our patient, we found an indirect, infravalvular, acquired LV-RA communication due to tricuspid valve involvement in infective endocarditis.
Treatment of the acquired Gerbode defect depends on symptoms, magnitude of shunt, flow volume, concomitant anatomic abnormalities, and co-morbidities. Unlike our patient, asymptomatic, chronic small defects can be managed conservatively.
Percutaneous transcatheter closure techniques have been employed in almost 25% of patients, mostly in high-risk surgical candidates. In most of the cases, surgical correction with a simple direct suture might be enough to close the defect, or pericardial patch closure with sutures may be used, if necessary, such as in our case. If the Gerbode defect is associated with partial or complete destruction of the tricuspid valve, reconstruction or replacement of the tricuspid valve might be required [6].
While a congenital Gerbode defect affects younger patients and is frequently associated with other congenital cardiac anomalies [4, 7], the acquired defect affects older male patients [2] and most commonly occurs after cardiac surgery or percutaneous cardiac intervention (59.1%), and after infective endocarditis (28.4%). Lastly, the most frequent sites of infection are the aortic valve (40%) and the tricuspid valve (20%), and the most frequent microorganism is Staphylococcus (54%), followed by Streptococcus [4].
The pathophysiology of the Gerbode defect is based on the high-pressure gradient generated by the LV-RA shunt, leading to increased RA flow and dilation of the right chambers. Clinical manifestations can range from asymptomatic to severe heart failure (HF), depending on the volume and duration of the shunt [2, 8]. The most common symptom is dyspnea, which occurs due to congestion in the pulmonary circulation. It can present as left HF, and more frequently as right HF (fatigue, weakness, edema of the extremities). Fever and atrioventricular block are more common in the acquired defect [4].
The diagnosis is challenging, since it is a rare pathology, and transthoracic echocardiography has limited accuracy, especially in adults and patients with obesity and chest deformities. It is important to distinguish the high velocity LV to RA jet in Gerbode defect from conditions that increase pulmonary artery pressure and cause high velocity of the tricuspid regurgitation. Differentiation by echocardiography can be difficult, and the examination must be performed cautiously to prevent high systolic flow on Doppler from being falsely interpreted as tricuspid insufficiency and pulmonary arterial hypertension [6]. Transesophageal echocardiography is the most sensitive method for detecting LV-RA shunt, especially in patients with prosthetic valves [2]. Other diagnostic methods include cardiac catheterization, magnetic resonance imaging, and computed tomography angiography. Cardiac catheterization is important to quantify tricuspid regurgitation, clarify pulmonary artery hypertension, and investigate other conditions, such as pulmonary embolism and coronary artery disease [2].
For Gerbode defects with severe clinical manifestations, correct diagnosis and early treatment, especially in acquired cases, result in a better prognosis [1]. In our case, the diagnosis was unclear, and no obvious cause was found for pulmonary hypertension until a transesophageal echocardiogram was performed. At first, we were concerned about the surgical indication due to obesity and associated risks. After intense communication, a shared and patient-centered decision was to perform surgery. Since the tricuspid valve leaflet was affected by endocarditis, it was necessary to reconstruct the leaflet in addition to closing the shunt using a pericardial patch.
In conclusion, the Gerbode defect is rare, and the acquired form accounts for most of the reported cases. Diagnosis can be challenging because it mimics other pathologies such as tricuspid regurgitation and pulmonary artery hypertension. Its differentiation and diagnostic definition are made through imaging tests. Transesophageal echocardiography can add important information, such as the location of the defect and the flow gradient, although sophisticated imaging techniques (magnetic resonance imaging and computed tomography angiography) may be required in challenging cases. Treatment consists of closing the defect when refractory symptoms or complications arise, mainly in acquired shunts, as they are frequently associated with HF. The reported case was surgically corrected, with a good result and favorable evolution.
HF: heart failure
LA: left atrium
LV: left ventricle
RA: right atrium
RRB: Project administration, Resources, Writing—original draft, Writing—review & editing, Investigation, Visualization, Supervision. LPL: Writing—original draft, Investigation, Visualization. LBB: Writing—original draft, Visualization. AJCdPA: Writing—original draft, Investigation, Writing—review & editing, Validation. VEAC and SLSG: Resources, Writing—review & editing. BKS: Writing—original draft, Investigation. LCdB and RCS: Resources, Writing—original draft, Writing—review & editing. LFMB: Project administration, Supervision, Writing—review & editing. All authors read and approved the submitted version.
The authors declare that they have no conflicts of interest.
The study complies with the Declaration of Helsinki. Ethical approval for the case report study is not required according to the local Ethical Committee.
Informed consent to participate in the study was obtained from the participant.
Informed consent to publication was obtained from the relevant participant.
The data is not publicly available due to ethical restrictions and legal constraints, but the data analyzed during the current case report is available from the corresponding author on reasonable request.
Not applicable.
© The Author(s) 2026.
Open Exploration maintains a neutral stance on jurisdictional claims in published institutional affiliations and maps. All opinions expressed in this article are the personal views of the author(s) and do not represent the stance of the editorial team or the publisher.
Copyright: © The Author(s) 2026. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 25
Download: 7
Times Cited: 0
