Affiliation:
1Endodontics and Restorative Dentistry Department, Faculty of Dentistry, Latakia University, Latakia P.O. Box 2230, Syrian Arab Republic
Affiliation:
2Department of Oral Medicine, Faculty of Dentistry, Al-Andalus University for Medical Sciences, Qadmus P.O. Box 02400, Syrian Arab Republic
Email: Marwa3600@gmail.com
ORCID: https://orcid.org/0000-0002-4100-7853
Explor Med. 2025;6:1001359 DOI: https://doi.org/10.37349/emed.2025.1001359
Received: June 11, 2025 Accepted: September 03, 2025 Published: September 19, 2025
Academic Editor: Luca Testarelli, Sapienza University of Rome, Italy
This case report documents the successful endodontic retreatment of a mandibular first molar exhibiting four mesial root canals in a 20-year-old male patient—an exceptionally rare anatomical configuration. Following the extraction of the perforated distal root, careful clinical exploration revealed two supplementary canals demonstrating apical convergence with the primary canals. The treatment protocol incorporated ultrasonically activated irrigation, precision rotary instrumentation, and warm vertical compaction obturation with bioceramic sealer. This case underscores the critical importance of thorough anatomical exploration in complex root canal systems.
The primary objective of endodontic therapy is to preserve tooth function while eliminating pain through comprehensive disinfection and three-dimensional obturation of the root canal system [1]. A leading cause of endodontic failure is inadequate debridement of the root canal space [2, 3], as residual pulp tissue and subsequent microbial colonization have been shown to compromise treatment outcomes [4–6]. In some cases, organic tissue remnants persist due to the clinician’s inability to identify additional root canals.
The mandibular first molar, being the first permanent posterior tooth to erupt, is the most commonly treated tooth in endodontics [7]. Given its frequent need for endodontic intervention, clinicians must be prepared to address variations in its internal anatomy. Extensive in vitro and in vivo studies have documented morphological variations in this tooth, including extra roots, additional canals, lateral canals, and anastomoses within the mesial root [3, 8–12].
Despite these well-documented anatomical complexities, few clinical case reports have described the presence of four canals in the mesial root of mandibular first molars [13–18]. Accurate identification and localization of such additional canals are critical for achieving clinical success—a task greatly enhanced by the use of a dental operating microscope.
This case report demonstrates the endodontic management of a mandibular first molar featuring four canals within its mesial root.
The timeline is shown in Table 1.
Timeline.
| Date | Procedures performed |
|---|---|
| December 1, 2024 |
|
| December 15, 2024 |
|
| December 18, 2024 |
|
| January 3, 2025 |
|
| June 1, 2025 |
|
A 20-year-old male patient presented with pain in the right mandibular first molar, exacerbated during mastication. When taking the patient’s medical history, it was found that he had undergone endodontic treatment on the mandibular first molar approximately two years ago following spontaneous pain.
During the clinical examination, pain was observed upon both horizontal and vertical percussion. A radiographic image revealed inadequate endodontic treatment with periapical lesions, as well as a metallic screw in the distal root, causing damage to the mesial wall of the distal root.
Upon removal of the composite restoration and the metallic screw, a perforation was noted approximately 4 mm from the orifice of the distal canal, along with a crack extending from the canal orifice to the perforation site. Therefore, the decision was made to extract the distal root.
The treatment plan included extraction of the distal root (referred to an oral surgeon) and nonsurgical retreatment of the mesial canals.
The decision to preserve the mesial root was made based on several clinical and radiographic criteria.
Clinical criteria:
Root stability: the root is clinically stable, with no pathological mobility exceeding grade 1.
Periodontal health: no deep pockets or chronic gingival inflammation around the root.
Restorability: no significant loss of tooth structure, preventing proper restoration.
Patient’s general condition: the patient is a healthy 20-year-old with no systemic diseases (e.g., uncontrolled diabetes, heavy smoking) that could impair bone or tissue healing.
Radiographic criteria:
Sufficient root length.
Adequate root width: capable of withstanding occlusal forces after crowning.
Good surrounding bone support.
Complete endodontic treatment [13].
Upon reevaluation after 15 days, a new periapical radiograph demonstrated two mesial canals (buccal and lingual) with obturation material located approximately 5 mm short of the apex. The gutta-percha was removed using M3-RT retreatment rotary files (United Dental Group, China), and canal negotiation was initiated with K-files (Tomas, France) sizes #10 and #15.
Further exploration revealed:
A middle canal merging with the lingual canal 3 mm from the apex.
An additional canal between the middle and buccal canals, joining the buccal canal in the apical third (5 mm from the apex).
The canal lengths were initially determined using a Woodpecker v apex locator (Woodpecker, China), followed by radiographic verification to confirm accuracy.
Mechanical preparation was performed with K-files (Tomas, France) sizes #10 and #15, followed by a rotary file system (Cicada Dental, China) according to the following sequence: SX, S1, S2, F1, and F2. Upon reaching F1 (size 20, taper 0.06), there was minimal resistance to the file, and the dentinal chips appeared dark yellow, indicating inadequate preparation [14]. Preparation was continued up to F2 (size 25, taper 0.06), at which point the dentinal chips turned white, confirming sufficient debridement.
Possible reasons for larger taper:
The patient’s young age (20 years old) may have contributed to wider canals.
Pulp necrosis and intraradicular infection could have led to weakened canal walls, requiring a more tapered preparation to ensure proper cleaning and shaping.
Irrigation protocol included: 2.5% NaOCl, saline, and 2% chlorhexidine, activated with an Ultra-x ultrasonic device (Eighteenth, China).
Canals were dried with paper points and obturated with gutta-percha and bioceramic sealer (Meta Biomed Co., Ltd., Korea) using the continuous wave technique. After three days, the tooth was restored with a fiber post (Angelus, Brazil) and Filtek Z350 XT composite resin (3M ESPE, USA).
The tooth was subsequently crowned, and the case was followed up for six months. The patient remained asymptomatic, and radiographic examination revealed no radiolucencies, indicating successful healing.
Radiographic documentation of endodontic treatment phases (Figure 1).
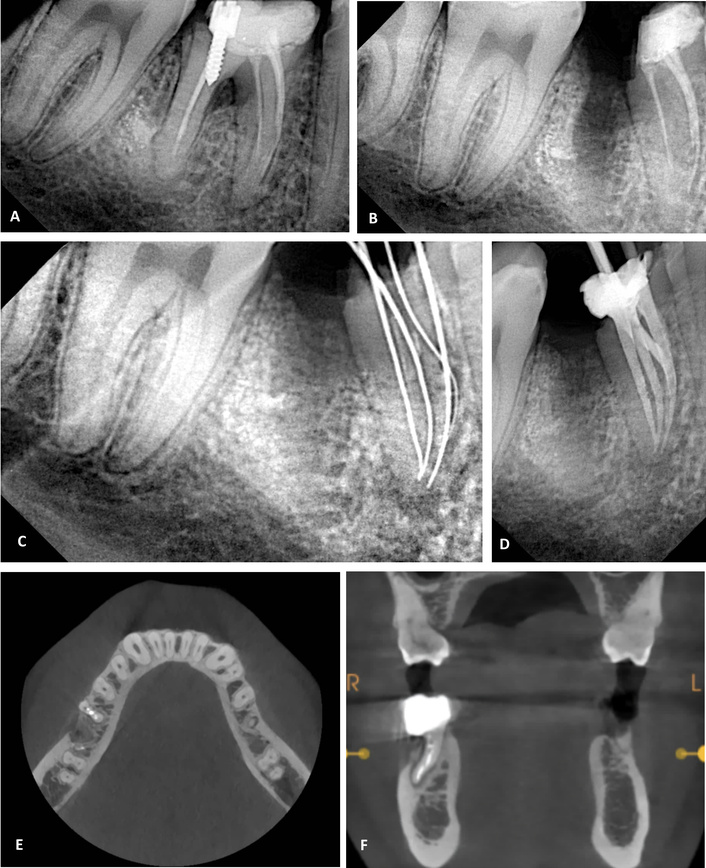
Radiographic documentation of endodontic treatment phases. (A) Diagnostic intraoral periapical radiograph prior to any therapeutic intervention. (B) Post-extraction intraoral periapical radiograph of the distal root. (C) Intraoral periapical radiograph demonstrating the four mesial canals. (D) Post-obturation intraoral periapical radiograph of the four canals. (E) A cone beam computed tomography (CBCT) image revealing the four canals. (F) Six-month follow-up CBCT image.
The patient expressed a strong desire to preserve his remaining teeth, particularly this tooth. Indeed, the outcome was satisfactory for him, as no pain was reported upon mastication after the completion of treatment, and functional efficiency was restored.
Root canal therapy maintains its position as the gold standard for treating irreversible pulpitis and periapical periodontitis. The fundamental objectives of endodontic treatment involve complete debridement, precise canal shaping, and three-dimensional obturation of the root canal system. Failure to identify and properly treat all canal spaces may compromise effective disinfection, ultimately leading to treatment failure [1]. Mandibular first molars emerge as the most frequently treated permanent teeth endodontically, owing to their early eruption and marked susceptibility to dental caries. While these molars typically exhibit two canals in the mesial root and one or two canals in the distal root, anatomical variations present significant diagnostic and therapeutic challenges [19].
Current data indicate that the middle mesial canal, situated between the mesiobuccal and mesiolingual canals, demonstrates a prevalence ranging from 1 to 15% [3]. In contrast, the presence of a fourth mesial canal is exceptionally rare, with only isolated cases reported in the endodontic literature (Table 2).
Literature review of four-canal variants in mandibular first molar mesial roots.
| Root configuration | Age | Gender | Ethnicity | Country | Reference |
|---|---|---|---|---|---|
| N/A | 23 | Male | N/A | USA | Reeh, 1998 [15] |
| Mesial root with a Gulavibala Type 11 (4-2) | 30 | Female | N/A | Iran | Aminsobhani et al., 2010 [16] |
| Mesial root with a Gulavibala Type 11 (4-2) | 37 | Female | Caucasian | USA | Martins and Anderson, 2015 [17] |
| N/A | 37 | Male | N/A | N/A | Vineet et al., 2018 [18] |
| N/A | 30 | Male | N/A | N/A | Kontakiotis and Tzanetakis, 2007 [20] |
| 4-2-1 pattern | 37 | Male | N/A | N/A | Subbiya et al., 2013 [21] |
N/A: not available.
The anatomical configuration of root canal systems exhibits significant ethnic variations, a critical consideration for effective endodontic diagnosis and treatment. This diversity is evidenced by disparate prevalence rates reported across different populations. For instance, Goel et al. [12] documented a 3.3% incidence of a four-canal morphology in the mesial root of mandibular first molars within an Indian population, while Wasti et al. [9] identified a classic Vertucci Type VIII configuration in a single specimen out of 30 teeth studied in Pakistan.
Further underscoring these population-specific variations, large-scale analyses reveal both the variety and frequency of these anatomical complexities. Sert and Bayirli’s [22] examination of 2,800 teeth in a Turkish cohort identified 36 specimens with configurations that deviated entirely from the established Vertucci classification, noting a pronounced propensity for such anomalies in mandibular teeth. In a Burmese population, Gulabivala et al. [11] reported a unique four-canal morphology (designated Type XI), distinguished by the canals merging to exit through two distinct apical foramina. This case report contributes a pivotal data point to this global tapestry of dental morphology by presenting, to our knowledge, the first documented instance and successful management of a mandibular first molar with four mesial canals in a Syrian patient.
Notably, the presentation of these anatomical complexities can also be influenced by factors beyond ethnicity, such as age. Significantly, while existing literature indicates a higher probability of additional canals in patients over 30 years of age, we observed this rare anatomical variation in a much younger patient (20 years old) [20].
The evolution of diagnostic imaging in endodontics, particularly the advent of cone beam computed tomography (CBCT), has fundamentally enhanced our ability to decipher complex root canal anatomies. CBCT offers unparalleled three-dimensional visualization, proving diagnostically superior to conventional radiography in identifying multi-canal systems, developmental anomalies, and pathological conditions [23, 24]. Its judicious application is, however, tempered by considerations of increased radiation exposure and availability. Notably, the successful management of the present case, which involved a rare four-canal mesial configuration, was achieved relying solely on meticulous clinical evaluation—including careful tactile exploration with fine files under high magnification and conventional radiography with multiple angulations. This outcome invites a critical discussion on the role of technology in clinical decision-making. It serves as a crucial reminder that advanced imaging, while powerful, is an adjunct to, rather than a replacement for, fundamental diagnostic acumen. This case demonstrates that when CBCT is unavailable, contraindicated due to radiation concerns (particularly in a young patient), or simply not deemed essential based on initial assessment, exceptional outcomes are still achievable. The cornerstone of success remains a rigorous, pre-operative clinical protocol: a deep understanding of anatomical possibilities, dedicated access cavity refinement, and the strategic use of ultrasonic troughing to uncover occult orifices. Therefore, this report does not diminish the value of CBCT but rather clarifies its role. It underscores that CBCT is best reserved for cases where conventional methods yield ambiguous or conflicting findings, thereby reinforcing the principle of As Low As Reasonably Achievable (ALARA) in radiation exposure while celebrating the enduring efficacy of masterful clinical skill.
Effective chemomechanical preparation constitutes the cornerstone of endodontic success, necessitating a tailored approach that reconciles the principle of optimal shaping with the imperative for complete debridement and disinfection according to specific clinical findings. Although conservative canal preparation remains a well-established tenet in contemporary endodontics [25], clinical judgment is paramount and may dictate modifications based on individualized anatomical and pathological presentations. In the present case, the patient’s youth was associated with relatively wide canals, and the presence of infection accompanied by changes in the canal walls warranted judicious yet sufficient enlargement to ensure thorough debridement and disinfection. This approach is consistent with established literature underscoring that customizing the extent of canal preparation to the specific clinical scenario is a critical determinant of long-term success [14, 26, 27]. However, even with optimal shaping, the complex anatomy of the root canal system, with its intricate web of canals, isthmi, and recesses, presents a significant challenge. Conventional syringe irrigation is often insufficient against these untouched areas. Therefore, passive ultrasonic irrigation (PUI) was employed, as its acoustic microstreaming significantly enhances biofilm disruption and debris removal, thereby complementing the mechanical preparation [28]. Furthermore, the selection of an obturation technique must account for the complexity of the prepared canal system. Bioceramic sealers are capable of flowing into irregularities and accessory canals, facilitating a consistent, homogeneous three-dimensional seal that ensures the complete obturation of intricate anatomical structures. These sealers also exhibit unique bioactive properties, most notably a demonstrated capacity to induce biomineralization. This process is characterized by the formation of mineral tags within the dentinal tubules and at the sealer-dentin interface, which significantly enhances the long-term seal. This approach underscores the importance of selecting materials and techniques that are specifically tailored to the unique anatomical challenges of each clinical case [29].
The long-term prognosis of posterior teeth that have undergone root resection and endodontic retreatment remains a topic of clinical debate, particularly given their exposure to higher occlusal forces compared to anterior teeth. The absence of occlusal force assessment in such cases further limits the accurate estimation of functional load. However, several factors positively contribute to tooth survival, including the preservation of adequate root length and width, the absence of supporting periodontal complications, and full coronal coverage to distribute occlusal forces. Available literature indicates that these teeth can achieve long-term survival when carefully selected. A study by Carnevale et al. [30] reported a 93% ten-year survival rate for molars treated with supportive therapy following root resection, while Falabella et al. [31] documented a 97.6% ten-year survival rate, with no significant influence of restoration type. Although Bühler’s [32] analysis demonstrated a failure rate of approximately 32% after ten years in some hemisection cases, case reports such as that by Ajlan have shown the potential for successful root resection in maxillary molars, with maintained function and structure for up to 14 years [33]. Therefore, ensuring sufficient root dimensions, the absence of periodontal disease, and full coronal coverage to distribute occlusal forces are critical factors in achieving high long-term survival rates for posterior teeth even after hemisection.
The presence of four mesial canals introduces unique challenges for long-term endodontic success. While complete debridement and obturation of complex anatomies reduce microbial load, the long-term prognosis may be influenced by factors such as isthmus cleanliness, accessory canal communication, and the biomechanical impact of multiple preparations on root strength. Recent studies suggest that teeth with intricate canal systems exhibit higher survival rates when adjunctive technologies like CBCT and ultrasonics are employed, though our case demonstrates that conventional methods can achieve comparable outcomes with meticulous execution.
Managing multiple canals within a confined root space demands exceptional technical precision. Key challenges include maintaining adequate dentin thickness to prevent fracture (particularly in younger patients with less sclerotic dentin), avoiding transportation of canals with divergent apices, and ensuring three-dimensional disinfection of interconnected anatomy.
This case underscores the viability of conventional techniques in resource-limited settings. The successful outcome supports the prioritization of clinician skill and anatomical knowledge over technological dependency. However, we acknowledge that CBCT remains invaluable for preoperative planning in high-risk anatomies, as it may reveal hidden complexities not detectable radiographically. Future studies should compare outcomes between conventional and CBCT-guided approaches for multi-canal systems to establish evidence-based protocols.
This case report adds to the growing yet limited evidence on four-canal mesial roots by presenting a successful short-term outcome. It underscores the importance of meticulous examination and customized treatment planning in endodontic retreatments. Although the six-month follow-up showed favorable results, longer-term observations are necessary to assess the prognosis more comprehensively. The use of magnification, ultrasonic activation, and bioceramic sealers played a key role in addressing this complex anatomical configuration.
CBCT: cone beam computed tomography
AH: Conceptualization, Investigation, Writing—original draft, Writing—review & editing. MK: Conceptualization, Investigation, Writing—original draft, Writing—review & editing. Both authors read and approved the submitted version.
Both authors declare that they have no conflicts of interest.
This study was conducted in accordance with the ethical principles of the Declaration of Helsinki (2013). Ethical approval was granted by the Scientific Research Council at Tishreen University, Latakia, Syrian Arab Republic (Approval #2027; December 1, 2024).
Informed consent to participate in the study was obtained from the participant.
Informed consent to publication was obtained from the relevant participant.
The dataset used during the study is available from the corresponding author upon request.
Not applicable.
© The Author(s) 2025.
Open Exploration maintains a neutral stance on jurisdictional claims in published institutional affiliations and maps. All opinions expressed in this article are the personal views of the author(s) and do not represent the stance of the editorial team or the publisher.
Copyright: © The Author(s) 2025. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 1948
Download: 22
Times Cited: 0
