Affiliation:
1Internal Medicine Residency Program, ECU Health Medical Center/Brody School of Medicine, Greenville, NC 27834, USA
Email: elsharuh22@ecu.edu
ORCID: https://orcid.org/0000-0003-4354-7236
Affiliation:
2School of Medicine, Mutah University, Karak 61710, Jordan
ORCID: https://orcid.org/0000-0002-3689-4566
Affiliation:
3Division of Gastroenterology and Hepatology, Mayo Clinic, Rochester, MN 55905, USA
ORCID: https://orcid.org/0009-0002-5142-7066
Affiliation:
1Internal Medicine Residency Program, ECU Health Medical Center/Brody School of Medicine, Greenville, NC 27834, USA
ORCID: https://orcid.org/0000-0002-7288-6408
Explor Med. 2023;4:421–427 DOI: https://doi.org/10.37349/emed.2023.00152
Received: December 28, 2022 Accepted: February 27, 2023 Published: July 12, 2023
Academic Editor: Lindsay A. Farrer, Boston University School of Medicine, USA
Bochdalek hernia (BH) is a congenital diaphragmatic defect primarily diagnosed in neonates and is usually left-sided. Adult diagnosis, especially of right-sided BH is exceedingly rare and usually presents with symptoms. Till now, only 31 cases have been diagnosed to be right-sided BH along with intrathoracic kidney. This report presents a 26-year-old asymptomatic male who was incidentally diagnosed with a massive right congenital diaphragmatic hernia. Imaging revealed severe abdominal herniation, a right intrathoracic ectopic kidney, and a right liver lobe hypoplasty along with hypertrophied left liver lobe extending down to the pelvic cavity. Several surgeons were consulted, with controversial opinions on whether elective surgery should be performed or withheld. Due to the high risk associated with surgery and the patient’s choice, the surgery was deferred. For almost 18 months, the patient did not report any symptoms or complications. This case highlights the rarity of asymptomatic right-sided BH in adults and the challenges in determining a management approach. Also, it proposes a conservative approach for such patients as a management modality. Most extensive diagrammatic defect reported is estimated to have a neck defect of 10 cm. Most BH cases have been treated surgically and reports on the outcome of a conservative approach are exceedingly rare. In such cases, patient preferences and a thorough risk assessment play vital roles in decision-making regarding conservative versus surgical approaches.
Bochdalek hernia (BH) is a congenital discontinuity of the diaphragm due to improper posterolateral fusion defect, allowing visceral content to herniate to the thorax [1]. The hernia is predominantly left-sided and usually diagnosed in the pediatric population, specifically neonates. If present in adulthood, it presents with pain and hernia-related symptoms [2, 3]. Until March 2016, 31 cases of right-sided BH were reported worldwide, with only 14% being asymptomatic [2, 4]. While a left-sided BH has been reported previously in Jordan, there have been no previous reports on right-sided BH [5]. This report presents potentially the world’s largest BH and the first right-sided BH with intrathoracic kidney with liver hypoplasty diagnosed in Jordan. This report aims to review the presentation of BH, embryological considerations, surgical management, and possible complications. Also, it aims to report the outcome of the conservative approach in BH and to raise awareness of such a method.
A 26-year-old male patient presented to the outpatient department for a pre-employment physical evaluation. His only complaint was chronic constipation with intermittent abdominal pain relieved with defecation and over-the-counter laxatives. The patient had no previous medical history or pertinent symptoms of any disease. He lived a sedentary lifestyle.
Clinical examination revealed normal vitals with a body mass index of 29 kg/m2. Chest auscultation revealed decreased air entry and bowel sounds over the right middle and lower lung. There were no signs of mediastinal shift. The abdomen appeared symmetrical, distended with bulging flanks. Palpation revealed enlarged liver with irregular edges extending to the pelvis. No other masses or tenderness were felt upon superficial and deep palpation. Complete blood count with a differential, comprehensive metabolic panel including renal function, and urinalysis was unremarkable. Upright posteroanterior chest X-ray demonstrated a mass in the right lower zone of the chest (Figure 1). Computerized tomography (CT) scan with oral and intravenous contrast showed herniation of the small bowel loops, ascending colon, transverse colon, majority of the right kidney, remnants of the right liver lobe, and gallbladder into the right hemithorax (Figure 2). The right liver lobe was hypoplastic, while the left liver lobe was hypertrophied and extended down to the pelvis (Figure 3). The right kidney showed an almost horizontal orientation above the edge of the remnants of the right diaphragm. The left adrenal gland was unremarkable, but the right adrenal gland was not identified. Sagittal images demonstrated the presence of posterior diaphragmatic crus. The diaphragmatic defect started 3 cm from the posterior diaphragmatic attachment in the sagittal plane. The maximal anteroposterior and mediolateral dimensions of the defect measured about 11.8 cm and 13 cm, respectively.
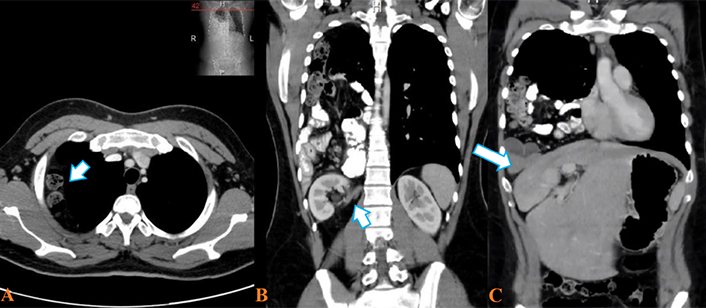
CT of the abdomen and pelvis. (A) Axial section: bowel loops appeared in the upper right hemithorax; (B) coronal view: herniating abdominal organs including right kidney; (C) coronal view: hypoplastic right liver lobe with left liver lobe hypertrophy
In this young adult with an asymptomatic massive diaphragmatic defect in addition to herniation of the bowel and kidney and downward extension of the liver, an elective surgical approach was the only option for correcting the hernia. Surgical approaches may include median laparotomy, laparoscopic reduction, or transabdominal robotic surgery. Due to possible difficult visualization, an additional thoracoscopy may be necessary.
The clinical question was whether an elective repair was indicated or not, given the high risk of recurrence after repair [1]. Surgery carried more risks in this patient as the abdominal cavity was too small to adapt to the reduction of all organs due to the huge liver reaching down to the pelvis (Figure 3). Consequently, the risk of developing abdominal compartment syndrome was highly significant.
Generally, two approaches can be considered to reduce the risk of abdominal compartment syndrome. First, the use of tissue expanders for the abdominal skin over four weeks after completion of the operation, during which the fascia can be closed, followed by the closure of the subcutaneous tissue and skin.
Second, the use of progressive pneumatic peritoneal dilatation, whereby a catheter with laparoscopic guidance is inserted into the peritoneal cavity and inflated until the abdominal cavity expands and is dilated enough to host back the migrating organs. In this method, care must be taken to avoid liver injury [6].
Due to the huge size of the defect, reconstituting the diaphragm was advised to be done using only non-absorbable mesh [7]. Given the risk of abdominal compartment syndrome, even without any post-reduction strangulations, management by leaving the abdomen open would further increase the risk of mesh infection.
While considering any surgical approach, special consideration should be given to lung re-expansion pulmonary edema. Lung re-expansion pulmonary edema is a well-defined complication occurring after the reduction of abdominal organs, typically occurring in highly compressed lungs, such as this patient’s right lung (Figure 4) [8]. Two-thirds of the right kidney is intrathoracic, and the kidney slid partially over the edge of the posterior remnant of the diagram (Figure 2). Thus, it would be most reasonable to leave the kidney in place to avoid any kinking of the ureter due to elongation through caudal repositioning.
After the initial discovery in June 2020 and after continuous discussion, the patient decided to defer surgery. He documented his condition in major hospitals in the country, anticipating the unfavorable scenario of an urgent need for cholecystectomy or appendicectomy. Other than avoiding contact sports, the patient is currently living a normal lifestyle and does not report any other symptoms.
Congenital diaphragmatic hernia affects 1 in 3,000 live births. BH accounts for 70–75% of all congenital diaphragmatic hernias usually diagnosed in neonates, with an 80–90% chance of left-sided involvement [1]. In previous studies, 13,138 CT reports were reviewed and showed that the prevalence of BH was 0.17% and 1 of 2,000 based on autopsy studies [3, 9]. Chest X-rays are sensitive only in detecting large BH, where gas-filled bowel loops or a lung base soft-tissue opacity lesion is seen. Thus, a normal X-ray should not exclude BH [1, 10].
The defect size on CT scans does not necessarily correlate with the hernia size, which may be much larger [10]. In a review of 124 articles, the mean size of the right-sided diaphragmatic defect was 37 cm2 [2]. Another systematic review showed that the median age was 53.5 years, 68% of patients were symptomatic, and most intrathoracic kidneys were right-sided [11]. The largest BH reported in the literature was estimated to have a neck of 10 cm [12]. In this report, the right-sided BH with an estimated diaphragmatic neck of 13 cm and a defect size of 153.4 cm2 along with a right intrathoracic kidney, making it potentially the largest documented right-sided BH to date.
Ectopic intrathoracic kidneys were first categorized by Pfister-Goedeke and Brunier’s [13] classification of renal ectopia, and this case fits into the third group (Table 1). Intrathoracic ectopic kidney occurs approximately twice in males, is more common on the left side, and is the rarest form of all renal ectopia (< 5% of cases). The precise etiology of this phenomenon is debatable, with various hypotheses. Some suggested that the incidence of intrathoracic kidney in diaphragmatic hernia is less than 0.25%, thus, it is unlikely to result from the hernia itself [14]. Others suggested that the location could be affected by the adrenal gland or as a result of delayed ingrowth of the ureter into the metanephros. Due to imaging difficulties, information about adrenal gland location in patients with intrathoracic kidneys was scarce, but it was found that the gland could be above or below the kidney. Although questionable, this proposes that the adrenal gland may influence the final location of the ectopic kidney [15, 16]. Unfortunately, the adrenal gland in our case was not localized.
Classification of ectopic intrathoracic kidney
| Group number | Description |
|---|---|
| Group 1 | True ectopic intrathoracic kidney with closed diaphragm |
| Group 2 | Ectopic kidney due to diaphragmatic eventration |
| Group 3 | Ectopic kidney due to diaphragmatic hernia (either congenital or acquired) |
| Group 4 | Ectopic kidney due to traumatic rupture of the diaphragm |
Notably, the right liver lobe of this patient is hypoplastic, likely facilitating abdominal organ herniation. Although the exact etiology of liver hypoplasty in patients with BH remains uncertain, it has been hypothesized that abdominal organs compressing the liver may lead to hepatic hypoplasty. Several anomalies are associated with BH, including intestinal malrotation, cardiac anomalies, and pulmonary hypoplasty, but hepatic hypoplasty has been documented in only nine reports [17, 18].
Most authors recommended the surgical approach regardless of symptoms for treating BH [2]. Despite that, and because of the risks associated with this type of surgery and the variety of symptom severity, surgical decisions should be assessed on a case-by-case basis [19]. The transabdominal approach is preferred in complicated and bilateral hernias to explore the whole of the abdominal cavity if peritonitis is suspected. In contrast, the transthoracic approach provides better visualization of a diaphragmatic foramen in right-sided hernias and obese patients [10, 20, 21].
The conservative approach entails monitoring for the progression of symptoms along with possible complications like pulmonary hypertension or renal function [11, 20]. The decision to pursue such an approach must consider the patient’s request, the symptoms of the patient, and the degree of herniated organ injury. In a previous systematic review that reviewed the management approach for BH, most patients were treated surgically. Nevertheless, three patients were managed conservatively and did not report any symptoms later [22].
This case demonstrates the importance of a multidisciplinary approach and patient education when deciding the need for elective surgery. This report is the first to report the outcome of almost 18 months of conservative management in which the patient had no other symptoms or complications.
In conclusion, BH is more commonly reported on the left side in children but can still be present in the adult population and on the right side. The surgical approach is the most recommended approach up to date. More consideration shall be taken for a conservative approach as more cases are not reporting any complications.
BH: Bochdalek hernia
CT: computerized tomography
HES: Conceptualization, Writing—original draft, Writing—review & editing, Supervision. ZA: Conceptualization, Writing—original draft, Visualization. MA: Validation, Writing—review & editing. AH: Writing—review & editing. All authors read and approved the submitted version.
The authors declare that they have no conflicts of interest.
Ethical approval was waved for this report per Royal Medical Services institutional review boards (IRBs) as per their protocol for case reports. The study adhered to the principles outlined in the Declaration of Helsinki and maintained patient confidentiality.
Informed consent to participate in the study was obtained from all participants.
Informed consent to publication was obtained from relevant participants.
All generated and analyzed data for this study are included in the manuscript.
Not applicable.
© The Author(s) 2023.
Copyright: © The Author(s) 2023. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
