Affiliation:
1Department of Neurosciences, Institut de Recherche Biomédicale des Armées (IRBA), 91220 Brétigny sur Orge, France
2Deparment of Allergologie, Université Paris Cité, 75006 Paris, France
Email: drphamthi@gmail.com
ORCID: https://orcid.org/0000-0003-1819-2840
Affiliation:
3Department of Pneumology, Allergology and Thoracic Oncology, University Hospital of Montpellier and IDESP, Université Montpellier - Inserm, 34295 Montpellier, France
ORCID: https://orcid.org/0000-0001-7827-7964
Explor Asthma Allergy. 2025;3:100986 DOI: https://doi.org/10.37349/eaa.2025.100986
Received: April 22, 2025 Accepted: June 19, 2025 Published: July 07, 2025
Academic Editor: Umit Murat Sahiner, Hacettepe University Faculty of Medicine, Turkey
The article belongs to the special issue Climate Change, Allergy, and Immunotherapy
Climate change in the form of rising temperatures and pollution can intensify pollen allergies, increasing health burdens and demanding proactive public health policies. Here, we discuss the current perceptions of physicians and patients on the impact of climate change and some of the initiatives to address its impact on global health. Recent surveys suggest growing concern among healthcare professionals and patients over the expanding evidence that climate change is contributing to the onset and exacerbation of respiratory allergies. Limited evidence exists on effective strategies, but some of the proposed public policy solutions include enhanced pollen monitoring networks, promoting climate-health education in medical curricula, development of early warning systems for thunderstorm asthma, and allergen-reducing urban planning. Collaboration among clinicians, researchers, and policymakers is critical for developing targeted measures that build resilience against climate-driven pollen allergy.
Climate change significantly influences the onset and pathogenic aspects of hypersensitivity in pollen allergy [1]. Due to rising temperatures and increased atmospheric carbon dioxide levels, plants prolong the flowering season, and pollen production intensifies, exposing individuals to higher allergenic loads. Atmospheric air pollution also plays a role in increasing pollen allergenicity and human sensitization [2]. These environmental changes can enhance sensitization in susceptible individuals and trigger exacerbated immune responses. Understanding these interactions is essential for developing effective public health strategies and mitigating the increasing burden of pollen allergies. Estimates indicate that pollen allergy already affects 10–30% of the European population. Still, current models estimate that pollen allergy will expand into areas where it is currently uncommon and become a frequent and widespread health problem [3]. The European Respiratory Society stated that climate change could cause significant respiratory morbidity related to increased prevalence and exacerbation of chronic respiratory diseases [4]. Damage caused by climate change could extend to several organs and affect many aspects of healthcare [5].
As climate change alters the landscape of pollen allergy and its impact on human health, healthcare professionals and patients must remain informed and proactive. This perspective article aims to discuss what is known about the current perceptions of primary care physicians (PCPs) and allergists regarding the effects of climate change and how people with pollen-derived allergic rhinitis or allergic asthma can cope. Finally, novel approaches that could help physicians and patients cope with climate change and possible public policy measures to mitigate its effects are discussed.
Surveys conducted by medical societies and other organizations are the primary source of information for evaluating the impact of climate change on the health care practices of professionals. The results of these surveys suggest growing concern over the expanding evidence that climate change is driving respiratory disease onset and exacerbation.
A survey by the American Thoracic Society (ATS) of 915 US members (mainly pulmonary and critical care physicians and pediatricians) considered that climate change is relevant to patient care (65% of respondents) and that its impact could already be observed among their patients and is likely to increase in the future [6]. In this survey, 58% of respondents indicated observing increased allergy symptoms from exposure to plants and molds. Similarly, American Academy of Allergy Asthma and Immunology (AAAAI) members have detected medical problems caused by climate change among their patients [7]. Similar concerns were shown by a national survey among 117 Italian pediatric pulmonologists and Italian Pediatric Respiratory Society members conducted in 2020–2021 [8]. The respondents indicated an increase in the incidence (90.6%) and severity (67.5%) of allergic respiratory diseases among their patients. Significantly, 61% of respondents felt that there had been an increase in the number of children sensitized to pollen. Further, 82% of survey respondents also stated that pollen-induced rhinitis and asthma have worsened, and approximately 77% of respondents believe the pollen production window has changed (starting earlier or being longer). A more recent survey among Italian pediatricians corroborated these results [9]. Similarly, a survey of 408 German pediatricians conducted in 2020 showed that for most respondents, the most significant effects of climate change on children’s health were considered to be longer and stronger pollen seasons [10].
An online survey conducted in France in October 2023 also revealed a strong concern among physicians (mostly allergists) for the impact of climate change on health and the increase in pollen allergy [11]. This survey (N = 107) showed that over the previous four pollen seasons (2019 to 2023), 90% of the allergists perceived an increase in the number of patients compared to previous years and the severity of symptoms (Figure 1). Further, they noted that the clinical presentation had changed in 57.4% of cases, with more ocular and bronchial symptoms. In response to these changes, allergists increased allergen immunotherapy (increasing doses in 52.3% of cases or duration of treatment in 90.7% of cases). This survey confirmed in real life the increased incidence of visits for pollen allergies, with changes in their typologies (often more severe, more cases of conjunctivitis and asthma), with a concomitant increase in demand for care [11].
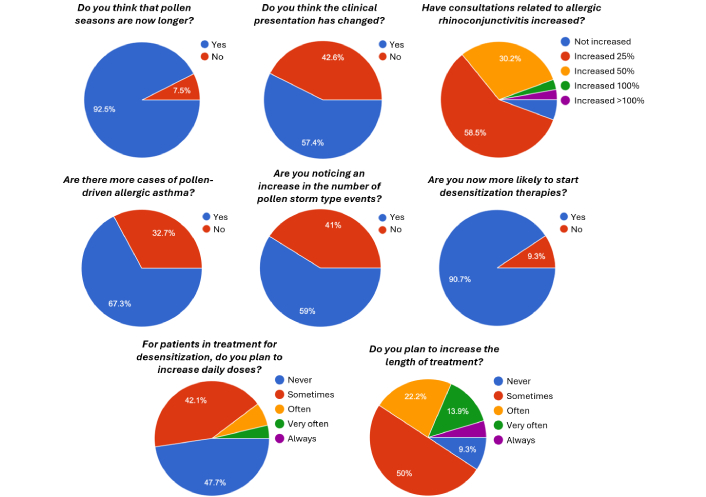
Results of a survey in France on changes in frequency, symptoms, and treatments due to pollen allergy in recent years [11]
PCPs are uniquely positioned to identify people with allergic symptoms because they evaluate many patients daily. Many allergic conditions, like seasonal allergies, food allergies, eczema, and asthma, present with non-specific symptoms that patients report during regular primary care visits. In the Netherlands, a 25-year longitudinal study analyzed trends between increased air temperature due to climate change and the frequency of seasonal allergic rhinitis visits to PCPs [12]. This study observed a longer duration of the period in which seasonal allergy rhinitis appears, with a tendency towards an earlier start of rhinitis symptoms in warmer years. The patients’ contacts with PCPs slightly increased over the 25-year period (from 2.0 to 2.2; P = 0.015), despite the increased patient education and wider availability of allergy medication without the need for PCP consultation, suggesting an increase in severity [12].
In summary, physicians treating people with pollen allergy in many countries have already sensed the need for action in the face of increasing and more severe cases. The ongoing relationship of PCPs with patients allows them to track changes over time, which can be essential for early intervention. In some countries, the changes induced by climate change in pollen allergy patterns have already been translated into changes in therapy.
There is a scarcity of studies evaluating how patients with pollen allergies perceive the effects of climate change and react to them. These perceptions vary widely depending on personal experiences, the severity of their symptoms, cultural background, and knowledge about the condition. Some patients may feel depressed, limiting their outdoor activities and their quality of life. In contrast, other patients perceive pollen allergy as a minor and temporary condition, especially compared to other chronic diseases, and rely on over-the-counter medications without professional guidance. For example, a survey of patients in Germany showed that they did not change their habits of visiting parks despite high pollen concentrations and rather regulated their pollen-related allergy symptoms through the use of medication [13]. Respondents to this survey recommended that urban space planning should consider more non-allergenic trees and improve public pollen information and warning systems. In the case of children with asthma and pollen allergy, a survey in the US showed high levels of concern regarding climate change among parents and caregivers [14]. This study suggested that clinicians should be trained to provide support to these caregivers by discussing with them the impact of climate change on the respiratory health of the patients.
With the objective of empowering patients to better manage their pollen allergy symptoms, numerous mobile applications have been developed and tested [15]. For example, the MASK-air is a mobile phone app that can be used to collect data on overall, nasal, and ocular allergic asthma symptoms, effects on work, and medication use, using visual analog scales [16]. It can be used as an allergy diary and a self-monitoring and medication adherence system to assist with the self-management of allergic rhinitis and asthma symptoms. Husteblume is a mobile phone app specifically designed to help manage pollen allergies through personalized support, allowing users to monitor pollen levels and track their symptoms [17]. It includes a pollen forecast (for ragweed, mugwort, and birch), a regional/national pollen calendar, and a pollen alarm for early warnings. The symptom diary can help better understand individual reactions and provide information on tailored therapies, allergy susceptibility, and treatment methods. AllergyMonitor is a mobile app for recording pollen allergy and asthma symptoms experienced, allowing reporting to the allergist their precise type and severity, as well as keeping track of patient adherence to prescribed therapies [18]. Other pollen-specific applications have been developed and tested [15], generally with very good acceptability and high adherence by patients, suggesting that these tools provide a clear benefit for the patient. Further, allergy diaries can be excellent real-world data sources for research on allergy and for monitoring changes in pollen susceptibility due to climate change. Also, if used in geo-located mobile phones, allergy diaries could potentially be used to detect pollen seasons and monitor patterns of allergy [19].
Another exciting application of mobile phone platforms is the use of social media to track pollen allergy and estimate disease burden. This approach has been demonstrated in studies in several countries [20, 21]. Although mixed results have been found for some countries and specific media, generally social media platforms have been found to enable the collection of real-time data on allergy-related symptoms and behaviors. By analyzing the geotagged information from posts, studies have been able to correlate regional pollen counts with reported symptoms, helping with the mapping and timing of allergy outbreaks and supplementing traditional pollen monitoring systems [22].
Given that climate change can lead to numerous unpredictable and long-lasting impacts on allergic respiratory diseases, it is essential for health professionals to play a proactive role in addressing these challenges (Table 1) [23]. This awareness would not only improve individual patient care but also strengthen public health responses to emerging environmental challenges. However, there is still a lack of supporting literature and few studies evaluate the impact of interventions. Health concerns about climate and environmental change may serve as a powerful catalyst for action among healthcare professionals, but robust evidence is needed to determine what actions should be prioritized [23].
A call to action on climate change
Health professionals should not only raise awareness about these risks but also advocate for the implementation of effective mitigation and adaptation strategies. For example, it has been suggested that pediatricians need to better understand the impact of climate change on children’s respiratory health [24]. In this regard, physicians should learn how to advise patients to stay informed about local updates on weather conditions, heat waves, air quality, and pollen levels so they can take proactive steps and adopt appropriate behaviors to reduce harmful environmental exposures. This advice may include maintaining consistent use of prescribed controller medications to manage symptoms, keeping a rescue inhaler readily available on days with increased risk, minimizing time spent outdoors during high-exposure periods, and avoiding strenuous or prolonged outdoor activities when conditions are unfavorable [24]. In a survey of physicians in France, the majority of allergists mentioned the possibility of extending the allergen immunotherapy treatments to adapt to the observation of the lengthening of pollen seasons because an early start in pre-pollen season would have marked favorable immunological effects for the patient [11].
In the US, the Association of American Medical Colleges, the National League for Nursing, and other organizations have recommended that health professions education incorporate courses on the effects of climate change on health. Some medical schools have started offering courses on climate change and health, and current and future medical students could play in driving the integration of climate topics into the pre-clinical curriculum [25]. Also, in some medical schools new continuing education programs are being established to help healthcare providers and public health professionals understand and mitigate the health consequences of climate change [7]. Understanding how climate change affects their patients should allow new physicians to contribute to preventive strategies at both individual and public health levels, including promoting allergy-related health awareness and patient counseling on risks.
Several initiatives and strategies have emerged in many countries as part of broader public health and climate adaptation efforts to address the increase in pollen allergy resulting from climate change. For example, some countries and regions have established or expanded pollen monitoring networks. Some European countries have comprehensive monitoring programs integrated into environmental and public health policies. For example, the UK Health Security Agency (UKHSA) has published a detailed report on the impact of climate change on allergies highlighting that the continued long-term monitoring of pollen across the UK and the development of taxa-specific forecasts for key aeroallergens to help with allergy management should be key research priorities [26]. Also in Germany, a report has argued for the provision of human and financial resources for the implementation of effective pollen monitoring to guide public health policy [27]. However, a global survey of coordinators of the Worldwide Map of Pollen Monitoring Stations has revealed that aerobiological monitoring is currently sustained by complex, unreliable, and insufficient resourcing in many countries [28]. Even in countries with a low incidence of pollen-driven allergies, such as those in the South of Europe, there is an increased awareness of the need to increase regular pollen monitoring from some tree species, as notable increases in pollen loads and diversity in recent decades have been detected, especially in cities.
A critical aspect of monitoring and early warning of allergy risk happens during thunderstorms occurring during high pollen season, generating a phenomenon known as “thunderstorm asthma” [1, 29]. During these episodes, the extreme weather conditions can disturb and break up pollen grains, disintegrating them into smaller, respirable fragments that can penetrate deeper into the lungs when inhaled, leading to sudden, severe asthma attacks in sensitized individuals. Emergency departments have reported spikes in respiratory-related visits during and after thunderstorms, particularly in regions with high pollen counts, and understanding this relationship is crucial for public health preparedness. Pollution can also break up the pollen as well. A synergy between climate change, air pollution, extreme weather and pollen on allergy has been widely documented [1]. Awareness campaigns and early warning systems can help at-risk individuals take preventive measures. A survey of pediatricians in Italy revealed that only 56% of the participants knew what “thunderstorm asthma” is, but these thought it useful to warn pollen-allergic patients with asthma of the risk associated [8].
Another possibility for public policy action is the improvement of urban planning to avoid the introduction of trees with high allergenic potential, and proposals in this regard have already been suggested in many countries [26, 27, 30]. The allergenic potential of urban parks in the future is likely to increase due to a combination of longer pollen seasons, increased pollen allergenicity, and higher sensitization rates among the population [30]. Also, urban planning increasingly emphasizes green infrastructure that not only provides environmental benefits but also contributes to better air quality, as improving air circulation and reducing urban heat islands can indirectly influence pollen distribution and concentration. Another example of state-sponsored actions is the International Ragweed Day. Since 2011, the Health Research Institutes in France have designated the first Saturday of the summer as a day to raise global awareness about the health, environmental, and agricultural issues caused by this invasive plant. On this day, various organizations host events such as educational sessions, training, exhibitions, group weed removal efforts, and youth-focused activities.
Although there is no single universal policy focused solely on pollen allergies, improvements in pollen monitoring and urban planning could help mitigate risks of allergy symptomatology in affected people to adapt to climate change. However, it is generally agreed that much more needs to be done and that most public policies are still in a phase of early planning and implementation before they can be effective guides for healthcare professionals and patients.
Global warming and extreme weather events are expected to worsen in the coming decades and a direct consequence of these changes is the increase in the frequency and intensity of respiratory allergic diseases, such as allergic rhinitis and asthma. This would aggravate the already high burden of health care related to these diseases in Western countries. Allergists are trusted members of the sentinel community and must play a role as informants for social and economic decision-makers and in educating patients on climate change and its harmful effects on human health. In this regard, PCPs can perform initial assessments, ruling out other possible causes for the allergic symptoms, and provide management with recommendations for allergen avoidance (e.g., use of masks, use of air filters), over-the-counter antihistamines, nasal corticosteroids, and patient education. According to surveys, PCPs and allergists are generally aware of the increase of pollen-derived allergies in the population, but additional efforts to mitigate and adapt to the effects of climate change are needed. The use of new technologies could greatly help by, first, increasing the speed and accuracy of pollen information transmitted to patients and physicians so that measures can be taken; second, it could also improve the flow of information between patients and physicians in terms of symptom evaluation and therapy adjustment (Figure 2). The use of telehealth platforms for follow-ups, especially during peak allergy seasons, could ensure that patients can report symptoms and receive timely advice without needing an in-person visit. As empowering patients to monitor and manage their conditions, which can lead to better long-term outcomes, patients should be educated on allergens, symptom recognition, and preventive measures. Both physicians and patients should be aware that the consequences of climate change are largely unpredictable and unknown. For this reason, in addition to longer pollen seasons caused by warmer temperatures, it is possible that plants produce more pollen, that allergenic species colonize areas where they were previously uncommon, or that allergenic pollen proteins change. Therefore, local knowledge and local adaptation are required, and no universal solution can be applied. In this regard, physicians should keep abreast of the latest research on allergens, environmental triggers, and emerging treatments by taking continuing medical education courses and workshops. In cases in which patients with severe or complex allergies require expert intervention, the establishment of strong referral networks between primary care, allergists and immunologists could be essential. In conclusion, by combining continuous professional development, personalized patient care, and technology integration, PCPs and allergists can effectively adapt to the challenges posed by climate change and increased allergy cases. This comprehensive approach will not only improve patient outcomes but also enhance the overall resilience of the healthcare system in coping with climate change.
PCPs: primary care physicians
Medical writing support was provided by Dr. Francisco López de Saro (Trialance SCCL).
NPT: Conceptualization, Writing—original draft, Writing—review & editing. PD: Conceptualization, Writing—original draft, Writing—review & editing. Both authors read and approved the submitted version.
Nhan Pham-Thi reports receiving fees from ALK-Abelló, Chiesi, and Stallergenes Greer for Symposia. Pascal Demoly reports having received fees from ALK-Abelló, Astra Zeneca, Chiesi, GlaxoSmithKline, Menarini, Puressentiel, Stallergenes Greer, ThermoFisher Scientific, Viatris and Zambon.
Not applicable.
Not applicable.
Not applicable.
Not applicable.
Not applicable.
© The Author(s) 2025.
Open Exploration maintains a neutral stance on jurisdictional claims in published institutional affiliations and maps. All opinions expressed in this article are the personal views of the author(s) and do not represent the stance of the editorial team or the publisher.
Copyright: © The Author(s) 2025. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 3997
Download: 55
Times Cited: 0
Alessandro Cinquantasei ... Marcello Albanesi
Jean-Pierre Besancenot, Laurent Mascarell
