Affiliation:
1Servicio de Psiquiatría, Unidad de Hospitalización Psiquiátrica Parcial (UHPP), Hospital Universitario Marqués de Valdecilla, 39008 Santander, Spain
2Área de Neurociencias, Instituto de Investigación Valdecilla (IDIVAL), 39008 Santander, Spain
Email: anaisabelde.santiago@scsalud.es
ORCID: https://orcid.org/0000-0003-0648-9268
Affiliation:
1Servicio de Psiquiatría, Unidad de Hospitalización Psiquiátrica Parcial (UHPP), Hospital Universitario Marqués de Valdecilla, 39008 Santander, Spain
Affiliation:
1Servicio de Psiquiatría, Unidad de Hospitalización Psiquiátrica Parcial (UHPP), Hospital Universitario Marqués de Valdecilla, 39008 Santander, Spain
Affiliation:
1Servicio de Psiquiatría, Unidad de Hospitalización Psiquiátrica Parcial (UHPP), Hospital Universitario Marqués de Valdecilla, 39008 Santander, Spain
Affiliation:
1Servicio de Psiquiatría, Unidad de Hospitalización Psiquiátrica Parcial (UHPP), Hospital Universitario Marqués de Valdecilla, 39008 Santander, Spain
Affiliation:
1Servicio de Psiquiatría, Unidad de Hospitalización Psiquiátrica Parcial (UHPP), Hospital Universitario Marqués de Valdecilla, 39008 Santander, Spain
2Área de Neurociencias, Instituto de Investigación Valdecilla (IDIVAL), 39008 Santander, Spain
ORCID: https://orcid.org/0009-0009-1455-1771
Explor Neuroprot Ther. 2023;3:268–280 DOI: https://doi.org/10.37349/ent.2023.00051
Received: January 14, 2023 Accepted: July 04, 2023 Published: October 26, 2023
Academic Editor: Jorge Manzanares, Miguel Hernandez University, Spain
Aim: The present study aims to analyze the impact on cognitive recovery of an interdisciplinary treatment for acute and severe psychiatric patients.
Methods: The present research is a naturalistic observational study of 130 adults (mean age of 47.68 years, 68% women). Clinical severity was assessed using Brief Psychiatry Rating Scale (BPRS), Montgomery-Asberg Depression Rating Scale (MADRS), and Hamilton Anxiety Rating Scale (HARS). Functional performance was evaluated using the Functioning Assessment Short Test (FAST), and cognitive impairment by applying the Montreal Cognitive Assessment (MoCA). Patients were clustered into four diagnostic groups (non-affective psychosis, bipolar, depressive, and personality disorders) and had individualized psychopharmacological treatment. They receive a transdiagnostic group program including several interventions that have shown evidence of beneficial effects over the different cognitive domains impaired in mental illness (attention, speed of processing, memory, working memory, reasoning, and problem-solving), as well as social cognition domains (emotion processing and social skills), in combination with psychoeducation and some strategies oriented to achieve healthy lifestyle routines (balanced diet, physical exercise, sleep hygiene, and smoking and alcohol cessation).
Results: All clinical scales scores were improved after the end of treatment compared with those achieved at admission (BPRS, MADRS, and HARS scores below the cut-off point for establishing a case diagnosis). MoCA scores improved after the end of treatment concerning admission, both in the total score and in the differentiated cognitive domains, excluding orientation, which remained unchanged in the whole of the sample studied. No statistical significance was found in any comparisons between different diagnostic groups. No correlation between MoCA scores and BPRS, MADRS, or HARS scores at admission or discharge was found.
Conclusions: These results show that the interdisciplinary therapeutic intervention can be effective for recovering cognitive impairment associated with mental disorders, irrespective of the diagnosis.
The National Institute of Mental Health (NIMH) has formulated the most representative definition of severe mental disorder and has achieved the most significant consensus in the literature. This definition considers three dimensions: clinical diagnosis, chronicity of the disorder (time greater than two years), and moderate or severe impairment of the person’s psychosocial functioning [1]. Cognitive functions are essential for normal human functioning, and their impairment significantly negatively impacts everyday life. Cognitive functioning involves multiple mental abilities such as attention, memory, information processing and recall, problem-solving, judgment, and decision-making. Throughout life, cognitive performance varies in response to environmental changes [2].
Psychiatric disorders are heterogeneous, with various clinical and biological manifestations. However, there is increasing evidence of common neurobiological mechanisms leading to cognitive impairment in various psychiatric diseases. Therefore, one of the most current areas of research is the search for biomarkers of mental illness based on identified links in the pathogenesis of these diseases [2]. Although, over decades, cognitive impairment has been considered a hallmark feature of schizophrenia, it is nowadays accepted that cognitive impairment is not specific to psychosis. However, it is broadly distributed in psychiatric illnesses in general [3]. Cognitively impaired functioning is a central feature of severe mental disorders such as schizophrenia, bipolar disorders, or major depressive disorder [4, 5] and substantially impacts psychosocial functioning [6, 7]. Despite the extensive literature comparing cognitive dysfunction among these disorders, the relationship between cognitive dysfunction and symptom domains remains unclear. More and more studies have observed similar cognitive impairment patterns and profiles (memory, executive functions, attention, and processing speed) among these three diagnostic entities [4, 8]. There is evidence that the severity of cognitive dysfunction is not so much related to the diagnosis but to the domain of negative/disorganized symptoms shared by all [9]. Data from different and extensive meta-analyses confirm that most patients with bipolar disorder show neurocognitive dysfunction, even during euthymia. Approximately 40% to 60% of patients with bipolar disorders exhibit neurocognitive impairment, with significant heterogeneity among them [10, 11]. These impairments also seem unrelated to drug treatment [12]. Moreover, no differences are found between patients with unipolar and bipolar depression in remission [13].
Cognitive deficits have been reported in affective disorders, most frequently short-term memory impairment, attentional biases, and difficulties in decision-making, however, in extensive meta-analyses, there were no significant differences between the magnitude of impairments between the bipolar depression and major depressive disorder groups [14]. In anxiety disorders, most reported cognitive deficits are related to planning ability and short-term memory deficits [2]. Conversely, in patients with schizophrenia, the cognitive impairments most often reported in the literature are working memory, attention, processing speed, verbal and visual learning, reasoning and planning deficits, and difficulties in problem-solving and abstract thinking [7, 15, 16]. Although the range of cognitive problems might be diverse, several domains, such as executive function, attention, and working memory, seem most frequently impaired in all these mental disorders [6, 8].
Both categorical and dimensional approaches to diagnosis are essential for clinical work and research, and each has benefits and drawbacks. Dimensional methods have advantages for clinical practice, where decision-making determines whether to provide intervention and, if so, what level of intervention is indicated according to the severity of symptoms or symptom clusters [17, 18]. Based on this dimensional approach, there is growing support for a ‘transdiagnostic’ path that crosses the boundaries of traditional diagnosis to offer new perspectives on understanding mental health problems. The proposal to remove distinctions between categories in the classification of psychiatric disorders provides novel ways of classifying mental health problems, proposes alternative concepts to explain processes involved in mental health, and provides new approaches to clinical treatment and functional recovery [19].
In recent years there has been a growing interest in providing rehabilitation treatment for people with severe mental health problems to enable them to function normally and improve their quality of life. Given that impairment in basic cognitive functions is considered the precursor of disturbances in adaptive functioning [16], enhancing cognitive performance could improve the social and functional development of people affected by mental illness. Cognitive remediation has been demonstrated to improve cognition and social functioning, however, the relation between the improvement has yet to be determined [3].
Day hospitals are one of the settings in which patients with severe mental disorders are attended. The model of partial hospitalization or day hospital treatment for acute patients was first described in the 1960s in the United States of America. The Spanish Association of Neuropsychiatry (AEN) [20] defines the day hospital as an intensive, structured, time-limited, and continuous care setting oriented towards continuity of care in the community. It is characterized by treatment through the medium, defined as the use of time and space in a therapeutic way by integrating different therapeutic activities, interdisciplinary teamwork, and different resources. This model of healthcare aims to move patients from heteronomy to autonomy.
By 2012 at the Valdecilla University Hospital (HUMV) in Cantabria, the partial psychiatric in-patient unit (UHPP) was designed and implemented within the psychiatry department, following a model of treatment by the intensity of care, with the mission of providing intensive treatment, on a partial admission regime, to patients with an acute and severe psychiatric pathology requiring admission, but for whom admission with greater containment is not necessary [21]. In this way, the UHPP emerges as a unit that combines characteristics of hospital psychiatric treatment (intensity and containment) with basic elements of community treatment (no uprooting from the environment, strengthening patient autonomy, and less stigma associated with admission). A transdiagnostic approach to mental illness is carried out under the assumption that patients with different diagnoses share underlying biopsychosocial pathways.
The present study aims to test the efficacy of an integrated intervention (including cognitive stimulation, training in social skills, and problem-solving strategies) implemented as the routine treatment of an acute UHPP, to improve cognitive impairment in people with mental illness irrespective of the diagnosis. The hypothesis was that patients who have received this integrated intervention at UHPP would have better cognitive performance in all domains assessed regardless of diagnosis.
The present study is a naturalistic observational study of the results obtained in a cohort of 130 patients admitted to a UHPP, applying the usual treatments employed in standard clinical practice. This study was approved by the Medical Research Ethics Committee of Cantabria (CEIm) with reference number 2022.241, in accordance with the Declaration of Helsinki. All participants were > 18 years and gave written informed consent after receiving a detailed description of the study.
The present study was conducted in the acute UHPP for adults at the Valdecilla University Hospital (Santander, Spain), a reference hospital of the Cantabria Autonomous Community in the north of Spain. The healthcare area of UHPP has a population of 300,000 inhabitants. The interdisciplinary team comprises psychiatrist, psychologist, nursing staff, and occupational therapist.
UHPP cares for patients with severe mental illness in the sub-acute phase, aiming to achieve functional recovery and encourage the person to acquire the greatest possible autonomy to manage his or her own life. To achieve this goal, psychopharmacological treatment is used, improving cognitive performance, and attenuating clinical symptoms. Secondly, the activities in the different therapeutic groups are based on the model of interaction between thoughts, emotions, and behaviours, which postulates that, by initiating changes in one of these domains, the others will be affected, therefore, work on emotions and behaviours will also have positive effects on cognition. Thirdly, a healthy lifestyle is promoted, including improvements in diet, rest, and physical exercise, which contribute to and are related to cognitive functioning.
Psychotherapeutic interventions are conducted in cross-diagnostic groups encompassing the different domains: psychomotor stimulation, cognitive stimulation, occupational therapy, psychoeducation, solving problems, emotional self-regulation, social skills, healthy behaviours training, play therapy, and day-to-day activities.
All patients aged 18 years or older, admitted to UHPP between May 2020 and November 2022, were included in the study if they met the following criteria: 1) have a principal diagnosis according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-V) of non-affective psychotic disorder, bipolar disorder, affective disorder (depression) or anxiety disorder, or personality disorder; 2) presenting acute symptomatology for which acute intensive in-patient treatment was required for resolution; and 3) agreeing voluntarily be admitted to the acute psychiatric day hospital. Patients were excluded from admission and treatment in this unit for presenting any of the following clinical situations that required complete 24-hour in-patient treatment: aggressive or severely disturbed behaviour, suicidal risk, severe substance addiction, an organic brain disorder, or insufficient socio-family support for partial in-patient treatment in an acute psychiatric day hospital.
Socio-demographic data on admission to the unit collected by using an instrument specifically developed for this purpose. Mental status, cognitive functioning, physical functioning, and perceived quality of life were clinically evaluated. Psychiatric diagnosis was established using DSM-V criteria-length of psychiatric admission.
Assessment scales were used in their Spanish versions: Montgomery-Asberg Depression Rating Scale (MADRS) [22, 23]; Young Mania Rating Scale(YMRS) [24, 25]; Hamilton Anxiety Rating Scale (HARS) [26]; Brief Psychiatry Rating Scale (BPRS) [27]; Montreal Cognitive Assessment (MoCA) [28, 29]; Functioning Assessment Short Test (FAST) [30, 31]; and EuroQol-5 Dimension (EQ-5D) [32, 33]. While the BPRS is generally used to assess schizophrenia and other psychotic disorders, it is a useful measure for psychopathology dimensions across schizophrenia as well as bipolar disorder, and major depressive disorder. It covers a broad range of symptom domains with an efficient and valid assessment of symptom severity [9]. Shafer [34] conducted a meta-analysis of factor analyses of the BPRS, whose results suggested five subscales (with items in parentheses): affect (anxiety, guilt, depression, and somatic); positive symptoms (thought content, conceptual disorganization, hallucinatory behaviour, and grandiosity); negative symptoms (blunted affect, emotional withdrawal, and motor retardation); resistance (hostility, uncooperativeness, and suspiciousness); and activation (excitement, tension, and mannerisms-posturing).
Patients were assessed using the assessment instruments at admission and at discharge from the UHPP.
Outcome was assessed using the following criteria: 1) cognitive improvement; 2) psychopathological and functional improvement; 3) length of time treatment needed to be ongoing to achieve sufficient clinical improvement to discharge the patient; 4) perception of improvement in perceived quality of life; and 5) satisfaction with admission.
For statistical analysis, cases were grouped into four major diagnostic categories: non-affective psychosis; bipolar disorder; depressive disorder; and personality disorder. A descriptive analysis of clinical and socio-demographic variables was carried out. Comparison between groups was accomplished using analysis of variance (ANOVA) for continuous variables and chi-square test (X2) for categorical variables. Kruskal-Wallis tests were performed when needed and Student’s t-test was used to establish comparisons between mean scores on the assessment scales before and after treatment. Post hoc multiple comparisons (pairwise t-test) were corrected by Bonferroni. The significance level of 0.05 was set for all analyses. All secondary analyses were 2-tailed. The Statistical Package for Social Science (SPSS Inc., Chicago, IL, USA) version 22.0 was used for all statistical analyses.
During the period studied, 130 patients completed their treatment in partial psychiatric admission to the UHPP, with a mean age of 47.68 years, 68% women, whose mean age was higher than the mean age among men (50.63 vs. 41.52). However, the differences were not statistically significant. Table 1 shows the description of the sociodemographic and clinical variables for the subjects.
Cohort description: sociodemographic data and clinical features
| Variables | Females (N = 88) | Males (N = 42) | Total (N = 130) |
|---|---|---|---|
| Partner | |||
| Yes | 47 (53.4%) | 14 (33.3%) | 61 (46.9%) |
| No | 41 (46.6%) | 28 (66.7%) | 69 (53.1%) |
| Educational background | |||
| Basic education | 42 (47.7%) | 22 (52.4%) | 64 (49.2%) |
| Intermediate studies | 21 (23.9%) | 14 (33.3%) | 35 (26.9%) |
| Higher education | 25 (28.4%) | 6 (14.3%) | 31 (23.8%) |
| Employment status | |||
| Active job | 8 (9.1%) | 4 (9.5%) | 12 (9.2%) |
| Work sick leave | 30 (34.1%) | 19 (45.2%) | 49 (37.7%) |
| Unemployment | 50 (56.8%) | 19 (45.2%) | 69 (53.1%) |
| Household | |||
| Urban (> 10,000 inhabitants) | 52 (59.1%) | 29 (69.0%) | 81 (62.3%) |
| Intermediate (2,000–10,000 inhabitants) | 14 (15.9%) | 10 (23.8%) | 24 (18.5%) |
| Rural (< 2,000 inhabitants) | 22 (25.0%) | 3 (7.1%) | 25 (19.2%) |
| Available support | |||
| No | 1 (1.1%) | 1 (2.4%) | 2 (1.5%) |
| Familiar support | 58 (65.9%) | 24 (57.1%) | 82 (63.1%) |
| Social support | 6 (6.8%) | 6 (14.3%) | 12 (9.2%) |
| Socio-familiar support | 23 (26.1%) | 11 (26.2%) | 34 (26.2%) |
| Home country | |||
| Spain | 81 (92.0%) | 33 (81.0%) | 114 (87.7%) |
| Other country | 7 (8.0%) | 9 (19.0%) | 16 (12.3%) |
| Time in Spain (years) | 17.43 (SD 20.34) (4–62) | 17.33 (SD 11.12) (1–40) | 16.87 (SD 15.61) (1–62) |
| Median age | 50.63 (SD 13.43) (23–80) | 41.52 (SD 15.08) (19–79) | 47.68 (SD 14.56) (19–80) |
| Psychiatric history | |||
| No | 2 (2.3%) | 4 (9.5%) | 6 (4.6%) |
| Yes, more than one year | 8 (9.1%) | 7 (16.7%) | 15 (11.5%) |
| Yes, less than one year | 78 (88.6%) | 31 (73.8%) | 109 (83.8%) |
| Admission origin | |||
| Hospitalization unit | 44 (50.0%) | 24 (57.1%) | 68 (52.3%) |
| Emergency department | 6 (6.8%) | 4 (9.5%) | 10 (7.7%) |
| Outpatient setting | 38 (43.2%) | 14 (33.3%) | 52 (40.0%) |
| Diagnostic groups | |||
| Personality disorder | 14 (15.9%) | 5 (11.9%) | 19 (14.6%) |
| Psychotic disorder | 17 (19.3%) | 15 (35.7%) | 32 (24.6%) |
| Bipolar disorder | 15 (17.0%) | 11 (26.2%) | 26 (20.0%) |
| Depressive disorder | 42 (47.7%) | 11 (26.2%) | 53 (40.8%) |
| Mean hospital stays (days) | 32.52 (SD 16.78) (range 10–118) | 35.83 (SD 15.55) (range 9–84) | 33.59 (SD 16.40) (range 9–118) |
SD: standard deviation
As can be seen in Table 1, 84% of patients had been mentally ill for more than one year. More than half of the cases came from the full-time psychiatric hospitalization unit. The average length of stay in the UHPP was 34 days, with no notable differences according to gender. Sixty two percent of males were classified in the psychosis or bipolar disorder groups. However, females were admitted more frequently for depressive disorders (48% vs. 36% for psychosis or bipolar disorder). Psychiatric disorders were different with statistical significance between male and female patients (P < 0.05).
The scores obtained for all the clinical scales were improved after the end of treatment in comparison with those achieved at admission, with the BPRS, MADRS, and HARS scores below the cut-off point for establishing a case diagnosis (Table 2). The differences between the means on admission and at discharge, with the cut-off points established for each, were statistically significant, the only exception being the MADRS at the end of treatment, which was very close to the cut-off point. Although the FAST does not contemplate cut-off points, a 15-cut-off point was used for analysis purposes because all patients on admission to the UHPP were on sick leave from work, which implies 15 points on the occupational functioning subscale. When comparing mean scores, the psychosis group shows an increase on the BPRS positive symptoms subscale compared to the rest, although there are no differences in the group comparison, neither in total scores nor in the negative symptom subscale. The post hoc test shows no difference between the different diagnostic groups on admission for the total scores on the BPRS, although the psychosis group has a significantly higher score on the positive symptom subscale than the other three diagnostic groups. Also, patients with psychosis score higher on the negative symptom subscale, but the difference is only significant for the depressive disorder group (Table 2).
Staged clinical assessment: baseline and outcome scores. Multiple comparisons of mean scores before and afterwards treatment in UHPP between specific diagnostic groups with a Bonferroni post hoc test
| Assessment instrument | Depressive disorders (a) | Bipolar disorder (b) | Psychosis (c) | Personality disorders (d) | Total | Statistic | Value | P | pH | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N = 53 | N = 26 | N = 32 | N = 19 | N = 130 | ||||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||||
| BPRS-18 negative symptoms subscale | ||||||||||||||
| On admission | 1.8 | 2.2 | 2.1 | 2.5 | 3.5 | 2.8 | 2.1 | 2.0 | 2.3 | 2.5 | F | 3.422 | 0.019 | a < c* |
| At discharge | 0.9 | 1.9 | 0.5 | 1.1 | 1.6 | 2.1 | 0.7 | 1.0 | 1.0 | 1.7 | X2 | 5.130 | 0.163 | ns |
| BPRS-18 positive symptoms subscale | ||||||||||||||
| On admission | 0.8 | 1.9 | 2.5 | 2.2 | 4.8 | 4.1 | 1.4 | 1.7 | 2.2 | 3.1 | X2 | 35.794 | < 0.001 | a < c***; a < b**; c > d* |
| At discharge | 0.1 | 0.5 | 0.4 | 0.8 | 1.3 | 1.8 | 0.3 | 0.6 | 0.5 | 1.1 | X2 | 18.651 | < 0.001 | a < c*** |
| BPRS-18 total | ||||||||||||||
| On admission | 13.0 | 6.6 | 12.6 | 6.3 | 14.6 | 10.0 | 13.5 | 5.0 | 13.4 | 7.3 | F-w | 0.325 | 0.807 | ns |
| At discharge | 4.1 | 5.2 | 2.6 | 3.6 | 4.4 | 5.5 | 3.5 | 2.6 | 3.8 | 4.7 | X2 | 2.386 | 0.496 | ns |
| MADRS-10 score | ||||||||||||||
| On admission | 24.9 | 10.1 | 11.1 | 10.5 | 11.3 | 10.2 | 21.4 | 11.1 | 18.8 | 12.0 | F | 15.450 | < 0.001 | a > b, a > c***; c < d**; b < d* |
| At discharge | 7.3 | 8.6 | 3.4 | 5.3 | 4.2 | 5.4 | 5.8 | 3.9 | 5.7 | 7.0 | X2 | 8.230 | 0.041 | ns |
| HARS-14 score | ||||||||||||||
| On admission | 16.5 | 9.6 | 8.6 | 5.9 | 8.8 | 7.0 | 15.5 | 8.5 | 12.9 | 9.0 | F | 8.710 | < 0.001 | a > b, a > c***; b < d, c < d* |
| At discharge | 4.7 | 4.9 | 1.9 | 2.5 | 2.8 | 3.4 | 4.2 | 2.9 | 3.7 | 4.1 | X2 | 11.30 | 0.010 | a > b, b < d* |
*** P < 0.001; ** P < 0.01; * P < 0.05; F: ANOVA; F-w: Welch’s ANOVA; X2: chi-square test; ns: not significant
Statistically significant differences were found in the scores obtained on the MADRS scale on admission between the different diagnostic groups. Patients with depressive disorders showed the highest scores (24.94), followed by personality disorders (21.42), in comparison to lower and similar scores for the psychosis and bipolar disorder groups, both having a mean score of about 11 (Table 2). These differences disappeared at discharge, given that the four groups decreased similarly in the severity of depressive symptomatology, remaining below 6 (euthymia), both for the overall sample and for all diagnostic groups, except those with depressive disorders, which remained very slightly above 6 (7.25), as shown in Table 2. A Bonferroni post hoc analysis revealed that significant differences appeared at the time of admission in depressive symptomatology assessed with MADRS between the different diagnostic groups: patients with personality disorders had higher scores than those included in psychosis and bipolar disorders, with similar differences for both groups concerning personality disorders. Similarly, depressive patients have significantly higher scores than bipolar and psychotic disorders. These differences also being similar for both groups (> 13) and more significant than the differences with personality disorders (> 10). The higher MADRS score of the depressive group compared to the personality disorder group was not statistically significant. Differences in depressive symptomatology between the four diagnostic groups have disappeared after treatment.
Similar findings emerged for anxiety levels measured with the 14-item HARS-14. The mean scores decrease after treatment in the aggregate group and in the different diagnostic categories, and the differences between groups are statistically significant at admission and discharge. Personality disorders and depressive disorders were the most highly scored groups both at admission and discharge, compared to the psychosis and bipolar disorders, the latter group having the lowest scores (Table 2). The results of the post hoc analysis for the HARS scale reveal similar differences to those found for the MADRS scale. Both depressive disorders and personality disorders have higher scores on admission than psychosis and bipolar disorders, with no significant differences found between depressive disorders and personality disorders or between psychotic disorders and bipolar disorder. At discharge, there are only significant differences between the depressive disorders group, which has the highest mean score (4.75), and the bipolar disorders, which has the lowest mean score (1.91), with no differences found in the other comparisons.
Likewise, the MoCA scores improved after the end of treatment concerning those obtained on admission to the UHPP, both in the total score and in the differentiated cognitive domains, excluding orientation, which remained unchanged in the whole sample studied (Table 3).
MoCA scores: baseline and outcome of treatment
MoCA scores | Baseline | Outcome | ||||
|---|---|---|---|---|---|---|
| Min-max | Mean | SD | Min-max | Mean | SD | |
| Visuospatial/executive | 0–5 | 3.87 | 1.25 | 1–5 | 4.10 | 1.19 |
| Naming | 1–3 | 2.92 | 0.33 | 1–3 | 2.93 | 0.28 |
| Attention | 0–6 | 4.73 | 1.35 | 0–6 | 4.78 | 1.35 |
| Language | 0–3 | 2.06 | 0.93 | 0–3 | 2.31 | 0.87 |
| Abstraction | 0–2 | 1.33 | 0.82 | 0–2 | 1.48 | 0.74 |
| Delayed recall | 0–5 | 3.15 | 1.62 | 0–5 | 3.75 | 1.40 |
| Orientation | 4–6 | 5.91 | 0.34 | 2–6 | 5.91 | 0.46 |
| Total scores | 10–30 | 24.20 | 4.14 | 11–30 | 25.59 | 4.11 |
When these differences were compared by diagnostic groups using ANOVA with post hoc analysis (Bonferroni correction), no statistical significance was found in any of the comparisons. No correlation was found between MoCA scores and MADRS or HARS scores at admission or discharge. However, when comparing overall cognitive improvement, patients with bipolar disorder and psychosis were found to have improved cognitively more often (65.4% and 59.4% respectively) than patients with depressive disorders and personality disorders (43.4% and 26.3% respectively), resulting in statistically significant differences (P < 0.05) (Figure 1).
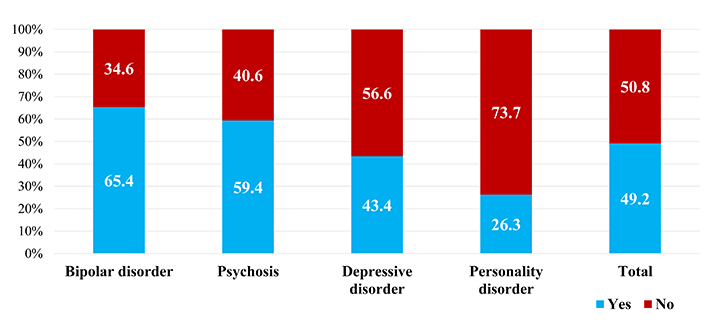
Cognitive recovery after comprehensive treatment at the UHPP, according to different diagnostic groups (N = 130, P = 0.033)
Statistical analysis showed non statistically significant differences while comparing cognitive recovery after treatment with the level of impairment on admission in every diagnostic cluster (Figure 2). Although cases of moderate or severe impairment were rare in personality disorders on admission, complete recovery after treatment was observed in this subgroup, with 67% of cases having no impairment and the remaining 33% showing mild impairment. Patients with severe cognitive impairment declined more frequently after treatment in the psychosis group (6.2 points decline), compared to bipolar (3.1 points) and depressive disorders (5.3 points). Furthermore, starting from a higher overall degree of impairment, patients with psychosis experienced more significant cognitive recovery than those with bipolar and depressive disorders. However, none of the differences found were statistically significant.
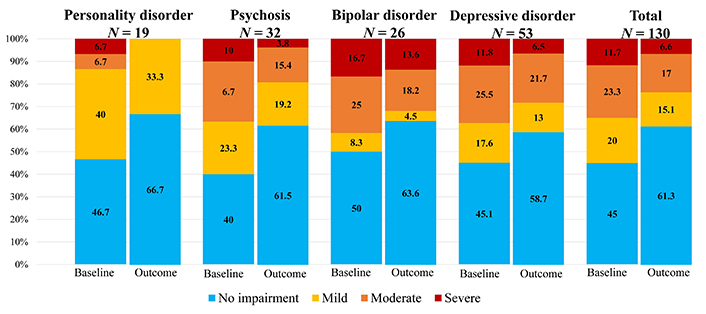
Cognitive impairment by groups according to MoCA scores at admission (baseline) and upon termination of comprehensive treatment (discharge) at the UHPP. MoCA scores: no impairment 26–30; mild 24–25; moderate 19–23; severe 0–18
No association between the existence of negative symptomatology in the BPRS subscale with impairment on admission or cognitive recovery after discharge was found. Similarly, prescription on admission or discontinuing benzodiazepines during treatment was inconsistent with cognitive impairment or cognitive recovery in the group under study.
In this study, clinical improvement (psychotic, depressive, and anxious) and cognitive recovery in all patients during UHPP admission, irrespective of their diagnosis was found. The scores obtained for all the clinical scales were improved after the end of treatment compared with those achieved at admission (BPRS, MADRS, and HARS scores below the cut-off point for establishing a case diagnosis), but no significant differences were found across diagnostic groups. MoCA scores improved after the end of treatment with respect to the admission, both in the total score and in the differentiated cognitive domains, excluding orientation, which remained unchanged in the whole of the sample studied. When these differences were compared by diagnostic groups no statistical significance was found in any of the comparisons. No correlation between MoCA scores and BPRS, MADRS, or HARS scores was found neither at admission nor discharge.
Over the period studied, almost 2/3 of the admissions were women, more frequently for depressive disorders, and the mean age was almost a decade higher than that of men, who were admitted more frequently for psychotic and bipolar disorders. These demographic differences found would seem to be consistent with the epidemiological data on the incidence and prevalence of mental disorders in Spain [35]. All patients have family and social support except for two cases since such support is required for partial admission as an alternative to total hospitalization. Although no statistically significant differences were found, women were more often highly educated (29% women vs. 14% men) and unemployed (57% vs. 45%). However, a higher frequency of retired women and housewives can explain this latter difference.
Half of the cases admitted to the UHPP are patients from the total hospitalization unit, thus contributing to earlier discharge. The remaining half come from outpatient departments or the emergency department, and in these cases, partial hospitalization avoids the need for 24-hour admission. Although all patients are in an acute clinical phase, most have a disease course longer than one year, being the first episode of the disease in only 5% of the cases.
The average length of stay is 33 days, slightly higher in males (35 vs. 32), although without significant differences. Stays differed slightly among the four diagnostic groups, ranging from 29 days (personality disorders) to 35 days (bipolar disorder), with no significant differences. This homogeneity in the need for intervention time is consistent with the transdiagnostic model of clinical approach.
The results obtained concerning the homogeneous decrease in MoCA scores, both in the total score and in the different domains, with no differences found between the diagnostic groups, is also congruent with the hypothesis of common underlying factors to the impairment in the different mental disorders [17, 18] and therefore to the efficacy of a transdiagnostic intervention in cognitive recovery [19].
The study findings of no differences in the BPRS total scores either before or after treatment between the different diagnostic groups reflects that it is a general symptomatology scale useful for measuring clinical severity, as well as changes in response to treatment. Interestingly, the BPRS score decreases homogeneously at the end of treatment in all diagnostic groups, including personality disorders, but not only in psychosis. Thus, the total scores decreased after treatment, falling below the cut-off point at the time of discharge, and the difference with those shown by the patients on admission was statistically significant. As expected, the ANOVA test showed that patients in the psychosis group had significantly higher scores on the positive symptom subscale in the assessment at admission compared to all diagnostic groups. At discharge, the psychosis group maintained a higher mean score on the positive subscale but with no significant differences from the other groups. They also scored higher on the negative symptom subscale, but surprisingly the difference was significant only compared with the depressive disorders. Although a priori, it could be argued that depressive symptomatology might score higher on the negative symptoms scale of the BPRS, the study results do not support this thesis. The findings obtained in this study are consistent with those found by Bora and colleagues [4, 5] in two meta-analyses in patients with schizophrenia, schizoaffective disorders, bipolar disorder, and major depressive disorder, concluding that the neuropsychological data do not provide clear evidence to differentiate schizophrenia from other diagnostic groups categorically.
By using the five subscales suggested by Shafer [34], Zhu et al. [9] found a correlation between the negative/disorganized symptoms of the BPRS-18 scale and the severity of cognitive dysfunction in all the disorders studied in their research (schizophrenia, bipolar depression, and major depression). In contrast, the present study observes no correlation between negative symptoms in BPRS and severity of impairment at admission or cognitive recovery at discharge, neither in the overall sample nor in the different diagnostic groups.
From the meta-analysis carried out on a total sample of 2,876 patients with bipolar disorder, Bourne et al. [12] reported an adverse effect of antipsychotic medication on one measure of memory, but no effects of lithium, antidepressants, or anticonvulsants; significantly better performance was also seen on memory tasks in the small number of patients who were drug-free compared with those who were on any psychotropic medication. The association between psychotropic drugs with cognitive impairment was not analyzed since the comparison involves many confounding factors in the study sample that would be impossible to remove. All psychotic and manic patients take antipsychotics during admission and depressive disorders antidepressants. When the relationship between the use of benzodiazepines and cognitive impairment or improvement in the patients studied was analyzed, no significant differences were found.
As expected, patients with depressive disorders scored significantly higher on the anxiety and depression scales than patients with bipolar disorder and psychosis, and although clinical improvement probably contributed to cognitive improvement, no significant relationship between the two variables was found. Cognitive remediation typically involves training on mental processes and tasks, as those applied in this study. These results are congruent with those found in the meta-analysis of cognitive rehabilitation in patients with various diagnoses, which suggested that cognitive rehabilitation may have a role in patients with mood disorders [6]. As previously reported by Rock and colleagues [14] cognitive impairment may represent a valuable target for therapy for depression because remediation of cognitive impairment, in addition to the remission of depressive symptoms, will be necessary for improving functional outcomes for depressive patients.
At the end of treatment, the entire sample improved on all clinical scales, with no significant differences between the different diagnostic groups. One possible interpretation of these results is the hypothesis proposed in this paper: the efficacy of an integrated intervention in a transdiagnostic model to improve cognitive impairment in people with mental illness. Comprehensive therapeutic interventions aimed at cognitive remediation, including cognitive stimulation and training in its functional application to acquire social skills and problem-solving strategies, should be included in the routine treatment of psychotic and bipolar disorders, depressive disorders, and personality disorders.
This study has substantial limitations, such as the small sample N, the need for a control group, and the MoCA, as an exclusive cognitive assessment instrument. Covariates were not included in the analyses due to the small N in some groups. This constitutes a limitation that could be remedied in further studies with a larger N sample size. Nevertheless, it is an observational study of routine clinical practice at UHPP. In this sense, it shows the health outcomes of psychiatric practice in the real world and may help identify therapeutic targets and areas for improvement.
Despite these limitations, the results obtained in this study show the usefulness of comprehensive transdiagnostic therapeutic interventions for the recovery of cognitive impairment associated with mental disorders, irrespective of the diagnosis.
Further research is needed to investigate cognitive functions in relation to different clusters of psychiatric illness, and studies need to be more carefully matched for confounder variables to identify predictors of treatment response and the factors that promote the generalization of treatment gains. Transdiagnostic models of intervention therapy are exciting and promising new areas of clinical research.
ANOVA: analysis of variance
BPRS: Brief Psychiatry Rating Scale
HARS: Hamilton Anxiety Rating Scale
MADRS: Montgomersy-Asberg Depression Rating Scale
MoCA: Montreal Cognitive Assessment
UHPP: partial psychiatric in-patient unit
AIDSD: Conceptualization, Formal analysis, Writing—original draft, Writing—review & editing. TPP and EGR: Conceptualization, Formal analysis, Writing—review & editing. EPJ: Formal analysis, Writing—review & editing. GCA and AZA: Formal analysis, Writing—review & editing. All authors contributed to the manuscript revision, read, and approved the submitted version.
The authors declare that they have no conflicts of interest.
This study was approved by the Medical Research Ethics Committee of Cantabria (CEIm) with reference number 2022.241. This study was conducted in accordance with the Declaration of Helsinki principles.
Informed consent to participate in the study was obtained from all participants.
Not applicable.
Not applicable.
Not applicable.
© The Author(s) 2023.
Copyright: © The Author(s) 2023. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 3674
Download: 31
Times Cited: 0
