Affiliation:
1Department of Internal Medicine, East Carolina University/Brody School of Medicine, Greenville, NC 27834, USA
Email: alih20@ecu.edu
ORCID: https://orcid.org/0000-0001-5546-9197
Affiliation:
2Department of Gastroenterology, Mather Hospital/Hofstra University Zucker School of Medicine, Port Jefferson, NY 11777, USA
ORCID: https://orcid.org/0000-0003-1375-8542
Affiliation:
3Department of Gastroenterology, Cleveland Clinic Foundation, Cleveland, OH 44195, USA
ORCID: https://orcid.org/0000-0002-6859-1789
Affiliation:
4Department of Internal Medicine, Quaid-e-Azam Medical College, Bahawalpur 63100, Pakistan
ORCID: https://orcid.org/0000-0002-4660-004X
Affiliation:
5Department of Gastroenterology, East Carolina University/Brody School of Medicine, Greenville, NC 27834, USA
ORCID: https://orcid.org/0000-0002-8447-2149
Affiliation:
6Department of Psychiatry, East Carolina University/Brody School of Medicine, Greenville, NC 27834, USA
ORCID: https://orcid.org/0000-0002-4684-778X
Affiliation:
2Department of Gastroenterology, Mather Hospital/Hofstra University Zucker School of Medicine, Port Jefferson, NY 11777, USA
ORCID: https://orcid.org/0000-0001-8581-1248
Affiliation:
2Department of Gastroenterology, Mather Hospital/Hofstra University Zucker School of Medicine, Port Jefferson, NY 11777, USA
ORCID: https://orcid.org/0000-0002-1187-8404
Explor Med. 2023;4:23–32 DOI: https://doi.org/10.37349/emed.2023.00122
Received: November 27, 2022 Accepted: December 23, 2022 Published: February 24, 2023
Academic Editor: Elizabeth Ann L. Enninga, Mayo Clinic College of Medicine and Science, USA
Aim: Patients with inflammatory bowel disease (IBD) are more likely to develop anxiety or depression. The study aimed to describe the trends and disparities of suicidal ideation (SI) in hospitalized IBD patients.
Methods: A retrospective study was conducted using the National Inpatient Sample (NIS) database, to analyze SI among the IBD hospitalizations from 2009 to 2019. Bivariate analysis was conducted using a chi-square test for categorical variables and an independent t-test for continuous variables. For prevalence, the trend over time was evaluated using the score test.
Results: There were 1,724 IBD hospitalizations with SI for the study period. There was a male (53.8%) and white race (74.2%) predominance. The mean age was 41.47 ± 0.25 years. The hospital stay decreased for IBD hospitalizations with SI from 7.97 days in 2009 to 7.57 days in 2019 (P < 0.001). The mean hospital charge increased from $44,664 in 2009 to $66,639 in 2019 (P < 0.001). The prevalence of SIs increased from 0.17% in 2009 to 0.29% in 2019 (P < 0.001). The mean age of these hospitalizations increased from 38 years in 2009 to 42.3 years in 2019 (P = 0.02). The prevalence of generalized anxiety disorder (GAD) increased from < 1% in 2009 to 12.19% in 2019 (P < 0.001). The prevalence of depression increased from 18.04% in 2009 to 51.21% in 2019 (P < 0.001). Inpatient mortality increased from 0% in 2009 to 2.43% in 2019 (P = 0.024). Among IBD hospitalizations, the male gender had a higher association with SIs than females (odds ratio 1.32 [95% confidence interval (CI) 1.06–1.66], P = 0.014).
Conclusions: There is a rise of SI among the IBD population. Specialized protocols should be in place in clinical settings and communities to identify and assess high-risk patients.
Globally, inflammatory bowel disease (IBD) affects over 6.8 million people and has had increasing prevalence in the past decade to substantial economic and social burdens on the healthcare systems [1]. Similarly, the prevalence of mood disorders in the US among adults is high, with an estimated 20% of US adults experiencing any mood disorder in their lifetime [2]. Compared to the general population, patients with IBD are more likely to develop a mood disorder such as anxiety or depression in their lifetime, with rates up to 15% and 20% [3]. One study has suggested a possible common inflammatory pathway between anxiety and depression and the development of immune-mediated inflammatory diseases such as IBD [4]. The study’s findings revealed an increased prevalence of anxiety and depression in IBD patients five years before their IBD diagnosis compared to the general population [4]. Undiagnosed psychiatric disorders (UPDs) have increased the risk of suicidal ideation (SI), suicide, and death [5]. Unfortunately, UPDs are common in patients with IBD [6, 7]. The rates of psychiatric diagnoses and SI in IBD still remain high. Marafini et al. [7] found that among 237 adult patients with IBD, at least 48% of these patients had one psychiatric diagnosis. Additionally, Ludvigsson et al. [8] showed that patients with IBD had an increased risk of suicide attempts with a hazard ratio ranging from 1.2 to 1.4. Furthermore, Xiong et al. [9] revealed that IBD has a higher prevalence of death from suicide with a relative risk of 1.25 [95% confidence interval (CI), 1.09–1.43] compared to those without IBD. Racial disparities have been demonstrated in IBD patients from healthcare utilization, therapy, and surgical outcomes, including complications, readmissions, and length of stay (LOS) [10, 11]. The charge of care for IBD has increased associated with higher healthcare utilization and out-of-pocket expenditures [12]. Although racial disparities have been demonstrated in patients with mental illnesses and suicide [13, 14], there are no studies describing the disparities amongst hospitalized patients with IBD who have SI. The present study aimed to describe the trends and disparities of mental illnesses and SI in hospitalized IBD patients.
The national inpatient sample (NIS) is designed by the Agency for Healthcare Research and Quality (AHRQ). It is the largest inpatient database in the US. The database approximates a 20% stratified sample of hospitals and sampling weights to calculate national estimates [15]. The data in NIS is provided using the International Classification of Diseases (ICD) 9 (before September 2015) and 10 (after October 2015) coding systems. The present study utilizes this database to identify hospitalizations with a primary diagnosis of IBD from 2009 to 2019. All patients below the age of 18 were excluded.
Primary outcomes included the prevalence of SIs in IBD hospitalizations. Secondary outcomes included the prevalence of generalized anxiety disorder (GAD) and major depressive disorder (MDD) in IBD hospitalizations with SI. Additional outcomes of interest included associations of gender and race among IBD hospitalizations with SIs. Trend analysis for respective outcomes was also reported to ascertain any time-based shifts.
Bivariate analysis was conducted using a chi-square test for categorical variables and an independent t-test for continuous variables. Categorical variables were presented as frequency (N) and percentage (%), and continuous variables were reported as mean with standard error (SE) as appropriate. The analysis had 0.05 as the threshold for statistical significance, and all P-values were 2-sided. For outcomes like the LOS and mean hospitalization charges, a hierarchical multivariate linear regression analysis was conducted to adjust the patient or hospital-level factors as in prior studies [16–18]. Multivariate logistic regression was conducted to assess the relationship between gender, race, and SIs among IBD hospitalizations; outcomes were reported as adjusted odds ratios (aORs) with 95% CI and P-value. The adjusted Wald test was utilized to compare slopes of time-based linear regression outcomes and Microsoft Excel (Microsoft Corporation, Redmond, WA, US) to generate figures [19, 20]. For prevalence, the trend over time was evaluated using the score test with the “tab odds” command; for this, 2009 was used as the reference category. The score test compares the odds of cases consecutively every year. It assumes that the trend is linear and can be used, as in prior studies [21, 22]. The present study utilized statistical software for data science (STATA) version 16.0 software (StataCorp LLC, Station, TX, USA).
There were 1,724 IBD hospitalizations (Crohn’s disease = 36%; ulcerative colitis = 64%) with SI for the study period. There was a male (53.8%) and white race (74.2%) predominance (Table 1). The mean age was lower in patients with SI (41.47 years) compared to those without SI (45.26 years; P < 0.001). There was a higher prevalence of patients in younger age groups of 18–34 years (38.9% vs. 34.6%) and 35–49 years (31.3% vs. 27%) among IBD hospitalizations with SI compared to those without SI (P < 0.001). No significant difference existed based on race for both groups (P = 0.15). IBD hospitalizations with SI had a higher Charlson Comorbidity Index (CCI) score of ≥ 3 than those without SI (8.9% vs. 5.6%, P = 0.006). There was a higher prevalence of GAD (4.9% vs. 0.8%) and depression (42.2% vs. 11.3%) in the SI group compared to the non-SI group (P < 0.001).
Bivariate analysis of primary diagnosis of IBD with and without a secondary diagnosis of SIs in the national inpatient database from 2009 to 2019
| Variables | No SIs | SIs | P-value |
|---|---|---|---|
| Total number of hospitalizations | 829,157 (99.77%) | 1,724 (0.23%) | |
| Mean age, years ± SE | 45.26 ± 0.84 | 41.47 ± 0.25 | P < 0.001 |
| Mean LOS, days ± SE | 5.30 ± 0.09 | 7.78 ± 0.50 | P < 0.001 |
| Mean hospitalization charges, USD ± SE | 41,667 ± 669 | 55,482 ± 256 | P = 0.0011 |
| Age group (years) | |||
| 18–34 | 271,062 (34.6%) | 671 (38.9%) | P < 0.001 |
| 35–49 | 211,178 (27.0%) | 540 (31.3%) | |
| 50–64 | 166,072 (21.2%) | 404 (23.4%) | |
| 65–79 | 99,130 (12.7%) | 69 (4.0%) | |
| ≥ 80 | 35,935 (4.6%) | 40 (2.3%) | |
| Gender | |||
| Male | 384,009 (46.3%) | 928 (53.8%) | P = 0.0057 |
| Female | 444,542 (53.7%) | 796 (46.2%) | |
| Race | |||
| White | 566,635 (73.3%) | 1,183 (74.2%) | P = 0.15 |
| Black | 105,332 (13.6%) | 253 (15.9%) | |
| Hispanic | 63,450 (8.2%) | 105 (6.6%) | |
| Asian | 11,476 (1.5%) | 4 (0.3%) | |
| Native American | 3,122 (0.4%) | 16 (1.0%) | |
| Other | 22,617 (2.9%) | 34 (2.1%) | |
| CCI score | |||
| 0 | 67,327 (8.1%) | 95 (5.6%) | P = 0.006 |
| 1 | 229,013 (27.7%) | 348 (20.3%) | |
| 2 | 530,210 (64.1%) | 1,268 (74.1%) | |
| ≥ 3 | 46,083 (5.6%) | 154 (8.9%) | |
| Hospital region | |||
| Northeast | 195,521 (24.7%) | 463 (28.3%) | P = 0.0001 |
| Midwest | 141,114 (17.8%) | 578 (35.4%) | |
| South | 399,249 (50.5%) | 411 (25.2%) | |
| West | 55,300 (7.0%) | 182 (11.1%) | |
| Hospital location and teaching status | |||
| Rural | 67,327 (8.1%) | 95 (5.6%) | P = 0.0001 |
| Urban nonteaching | 229,013 (27.7%) | 348 (20.3%) | |
| Urban teaching | 530,210 (64.1%) | 1,268 (74.1%) | |
| Expected primary payer | |||
| Medicare | 195,521 (24.7%) | 463 (28.3%) | P < 0.001 |
| Medicaid | 141,114 (17.8%) | 578 (35.4%) | |
| Private | 399,249 (50.5%) | 411 (25.2%) | |
| Other | 55,300 (7.0%) | 182 (11.1%) | |
| Median household income (quartile) | |||
| 1st | 203,291 (25.0%) | 472 (28.1%) | P = 0.097 |
| 2nd | 205,044 (25.2%) | 471 (28.0%) | |
| 3rd | 207,672 (25.5%) | 429 (25.5%) | |
| 4th | 198,512 (24.4%) | 310 (18.4%) | |
| Inpatient mortality | 3,027 (0.4%) | 10 (0.6%) | P = 0.55 |
| GAD | 6,789 (0.8%) | 84 (4.9%) | P < 0.001 |
| Depression | 93,891 (11.3%) | 728 (42.2%) | P < 0.001 |
| Chronic steroid use | 66,332 (8%) | 121 (7%) | P = 0.47 |
| Major abdominal surgeries | 107,790 (13%) | 155 (9%) | P = 0.06 |
The median household income was divided into 4 parts equally, the 1st through the 4th represents the 0–25th, 26th–50th, 51st–75th, and 76th–100th respectively. USD: United States dollar
There was a significantly higher LOS for IBD hospitalizations with SIs compared to those without it (7.78 ± 0.50 days vs. 5.30 ± 0.09 days, P < 0.001) for the study period (Supplementary material). However, the trend in LOS over the study period significantly decreased for IBD hospitalizations with SI from 7.97 days in 2009 to 7.57 days in 2019 (Figure 1; P < 0.001). There was a significantly higher mean hospital charge in IBD hospitalizations with SI compared to those without it ($41,667 vs. $55,482, P < 0.001) for the study period (Supplementary material). The mean hospital charges, however, increased from $44,664 in 2009 to $66,639 in 2019 for IBD hospitalizations with SI (Figure 2; P < 0.001; Supplementary material).
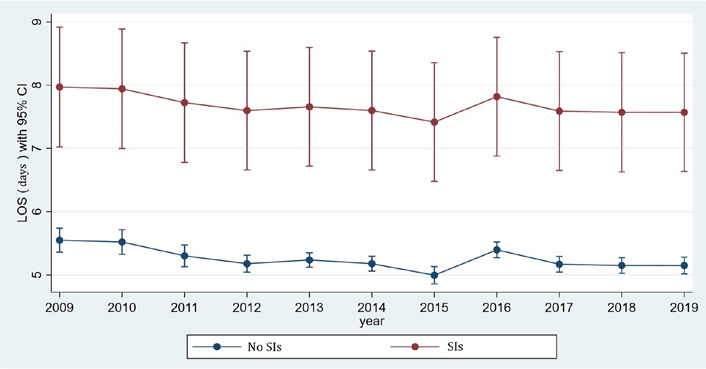
Comparative trend analysis of hospital LOS among IBD hospitalizations with or without SIs
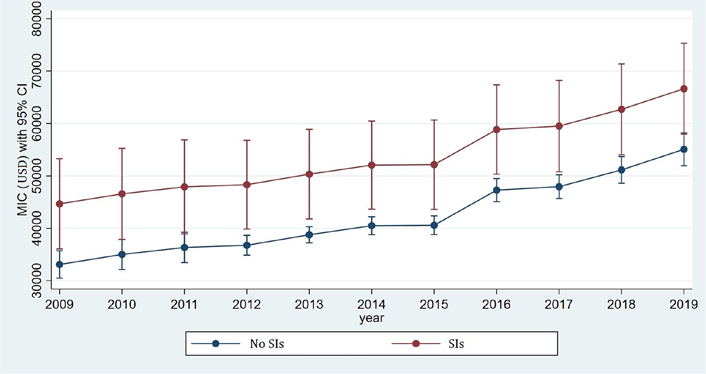
Comparative trend analysis of hospital mean inpatient charges (MIC) among IBD hospitalizations with or without SIs
The total IBD hospitalizations decreased from 75,813 in 2009 to 70,210 in 2019, without any statistical significance (P = 0.30). The prevalence of SIs in primary IBD hospitalizations increased from 0.17% (1.75 per 1,000 total IBD hospitalizations) in 2009 to 0.29% (2.91 per 1,000 total IBD hospitalizations) in 2019 (P < 0.001; Figure 3). Rates of SI peaked in 2015 at 3.20/1,000 total IBD hospitalizations, followed by a dip in 2016 with the rate of 1.43/1,000 total IBD hospitalizations, and continued to rise after that. The mean age of these patients increased from 38 years in 2009 to 42.3 years in 2019 (P = 0.02).
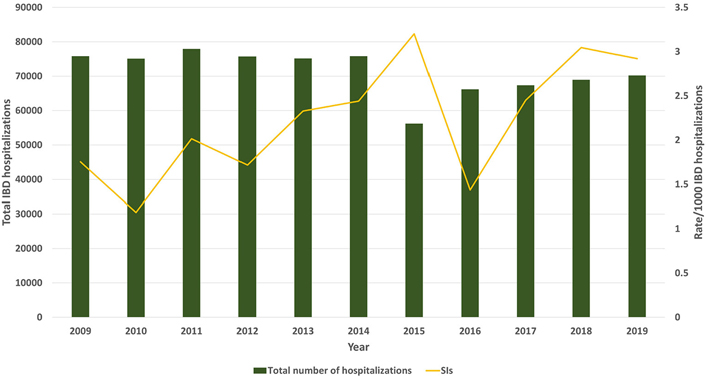
Rate of SIs in IBD hospitalizations. Bars show the total number of IBD hospitalizations per year; the yellow line shows the rate per 1,000 IBD hospitalizations with SIs
The total number of IBD hospitalizations with SIs decreased from 133 in 2009 to 205 in 2019 without any statistical significance (P = 0.27; Supplementary material). Among hospitalizations with IBD and SIs, the prevalence of GAD increased from < 1% in 2009 to 12.19% (121.9/1,000 IBD hospitalizations with SI; P < 0.001). The prevalence of depression increased from 18.04% (180.4/1,000 IBD hospitalizations with SI) in 2009 to 51.21% (512.1/1,000 IBD hospitalizations with SI) in 2019 as shown in Figure 4 (P < 0.001). Inpatient mortality among these patients increased from 0% in 2009 to 2.43% in 2019 (P = 0.024). The total frequency of steroid use was 7% in IBD hospitalizations with SI. The rate of steroid use increased from 6.7% in 2009 to 7.5% in 2019 (P = 0.62). Chronic steroid use was not associated with SIs in IBD hospitalizations (aOR 0.86, 95% CI 0.57–1.29, P = 0.45). The major abdominal surgeries (defined as rectal surgery, laparoscopic or open colectomies, total colectomies, or small bowel surgeries) decreased from 10% in 2009 to 2% in 2019 in IBD hospitalizations with SI (P < 0.001).
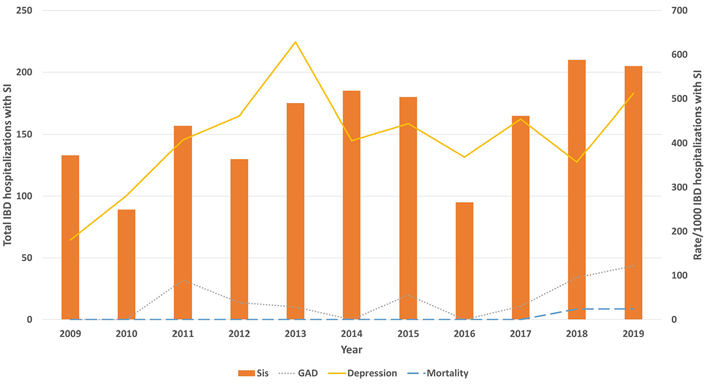
Rate of GAD, depression, and inpatient mortality in IBD hospitalizations with a secondary diagnosis of SI. Bars show the total IBD hospitalizations with a secondary diagnosis of SI per year; the yellow line shows the depression rate per 1,000 IBD hospitalizations with SI; the grey line shows the GAD rate per 1,000 IBD hospitalizations with SI; the blue line shows the inpatient mortality rate per 1,000 IBD hospitalizations with SI
Among IBD hospitalizations, there was a higher association of SIs in ulcerative colitis compared to Crohn’s disease (aOR 1.24, 95% CI 1.01–1.53, P = 0.04). The male gender had a higher association with SIs than females (aOR 1.32, 95% CI 1.06–1.66, P = 0.014). There was no difference in association with SIs in Blacks (aOR 1.09, 95% CI 0.81–1.48, P = 0.54), Hispanics (aOR 0.77, 95% CI 0.49–1.20, P = 0.25) or Asians/native Americans (aOR 0.17, 95% CI 0.02–1.27, P = 0.086) when compared to the white race.
The topic of suicidal behavior amongst patients with IBD has not been extensively explored in literature. Our study investigated the trends in SI within IBD hospitalization over an eleven-year period. Our results revealed that from 2009 to 2019, the prevalence of SI in IBD hospitalization increased from 0.17% to 0.29%, respectively. Even with the advancements in medical therapy for IBD over time, an increased trend in SI was still observed. However, a portion of these IBD hospitalizations might be those who also have a terminal illness, and hence, suicidal behavior may be observed amongst these patients contributing to the overall SI rate. Understanding the importance of considering regular psychiatric screening among IBD patients is crucial.
Our observations showed a higher prevalence of SI among IBD hospitalization in the age groups of 18–34 years (39%) and 35–49 years (31%). These statistics are consistent with a national study conducted in the United States involving 184,300 individuals, where SI was most prevalent among participants aged between 25–34 years and 35–44 years [23]. Another observation made in our analysis was that most CCI scores were less than one among IBD patients with SI. In our data, only 8.9% of the patients had a CCI score of more than 3. These patients might fall in the older age group where multiple comorbidities and no improvement in health status might contribute to SI.
Since IBD is often diagnosed in the second or third decade of life, it can often interfere with one’s ability to navigate the education system and obtain a job. The impact of uncontrolled IBD on the quality of life can significantly impair the psychological well-being of a patient. In our data, we observed an increase in the prevalence of GAD from < 1% in 2009 to 12.19% in 2019 among IBD hospitalized with SI. Along with GAD, we also noticed an increase in the prevalence of depression from 18% in 2009 to 51.21% in 2019. A study examining the US population’s GAD from 2008 to 2018 also noticed a 15% increase [24]. Despite abundant treatment options available since 2008 for GAD, it persists owing to the many factors that influence anxiety in an individual. Some of these factors include education, income, age, and race. Fuller-Thomson and Sulman [25] analyzed the link between IBD and clinical depression and found that approximately one in three patients diagnosed with IBD reported depression, and one in six patients had suicidal thoughts within a one-year study period. The findings from our data are also consistent with a national survey conducted in Canada which revealed that IBD patients had a two-fold increase in anxiety [26]. The American College of Gastroenterology (ACG) has now recommended psychiatric evaluation in the clinical guidelines for the management of Crohn’s disease [27].
In our study, there was a longer LOS among IBD hospitalizations with SI compared to those without it. A large clinical study was conducted on approximately 2,000 adults where depression was associated with a risk of exacerbation in IBD patients [28]. Given the possible link between depression and disease flare activity, it might explain why IBD hospitalizations with SI have a longer LOS due to potential complications that could delay the expected recovery time. A two-year study conducted on IBD patients with and without depression revealed that IBD patients with depression had a greater number of clinical visits [29]. This same study also noted a lack of compliance in treatment protocol among IBD patients with depression. This could further delay recovery time and increase mortality among these patients. We observed this trend in our data, where inpatient mortality among IBD hospitalizations with SI increased from 0% in 2009 to 2.43% in 2019. In the present study, there was a significantly higher mean hospital charge in IBD hospitalizations with SI than those without it. Due to increased LOS, the relapsing nature of IBD, and potential complications, all these factors could contribute towards an overall increase in mean hospital charge and mortality.
A large-scale study by Marchioni Beery et al. [30] among adult IBD patients with SI noticed a higher prevalence of SI among the male population. This trend is consistent with our data, where the male gender had a higher association with SIs than females. According to the Centers for Disease Control and Prevention (CDC), males are four times as more successful at executing suicide as compared to females. However, females report more suicidal thoughts than males in the United States [30]. Another two-year study involving IBD patients revealed that the female gender was linked with higher odds of anxiety and depression [31]. Additionally, Williet et al. [32] found that approximately 50% of IBD patients experience fatigue and poor quality of life. The production of inflammatory cytokines from uncontrolled IBD potentially contributes to this population’s increased prevalence of mental illness. Increased risk of suicide has been reported in several other chronic inflammatory diseases such as rheumatoid arthritis and systemic lupus erythematous compared to the general population [33].
Our retrospective study is one of the largest to evaluate the trends in SI amongst hospitalized IBD patients. We have highlighted that patients with IBD require a multidisciplinary approach to the medical and psychiatric illness to increase the chances of achieving disease remission. One of the limitations of our study is that NIS data does not reflect the actual occurrence of suicidal behavior or attempt since the NIS data lacks the coding concerning this differentiation. We identified risk factors for SI, such as the young to the mid-age group and low CCI scores. Some studies have shown genetic and immunological factors to be related to the mechanism of anxiety and depression among IBD patients [31]. However, given the complexity of this disease, further research is required to understand the mechanics involved. Since ACG guidelines recommend psychiatric assessment, only 12% of adult medical centers have been reported to possess the resources for a thorough evaluation [34]. A study by Davis et al. [35] showed an improvement in IBD patients when non-pharmacological management, such as cognitive behavioral therapy, was used to lower anxiety, and depression and improve quality of life. The results of our study might be limited to interpretation since we did not factor in blinding and randomization in this study.
In conclusion, as physicians, we should consider psychiatric evaluation in IBD patients who might be vulnerable to suicidal behavior. If these patients are provided with psychiatric help at an early stage, it can prove to be more beneficial. For these patients, the concept of a medical home can be applied, proving effective, and more equitable care can be provided. As discussed above, improvement in mental health might also improve the overall health condition of these patients. Through our study, we address the rise of SI among the IBD population, which should alert healthcare providers to develop guidelines for effective clinical management. Specialized interventional protocols should be in place in clinical settings and communities to identify and assess high-risk patients. Through effective screening, early identification, and treatment could improve the quality of life in the IBD population, lowering the prevalence of depression and anxiety associated with SI.
aOR: adjusted odds ratio
CCI: Charlson Comorbidity Index
CI: confidence interval
GAD: generalized anxiety disorder
IBD: inflammatory bowel disease
LOS: length of stay
NIS: National Inpatient Sample
SE: standard error
SI: suicidal ideation
The supplementary material for this article is available at: http://www.explorationpub.com/uploads/Article/file/1001122_sup_1.pdf.
HA: Conceptualization, Investigation, Writing—original draft, Writing—review & editing. RD: Conceptualization, Investigation, Writing—original draft, Writing—review & editing. SP: Investigation, Writing—original draft, Writing—review & editing. LSM: Writing—original draft, Writing—review & editing. PP: Validation, Writing— review & editing, Supervision. SS: Validation, Writing—review & editing, Supervision. KF: Writing—review & editing, Supervision. RR: Conceptualization, Validation, Supervision. All authors read and approved the submitted version.
The authors declare that they have no conflicts of interest.
Not applicable.
Not applicable
Not applicable.
The datasets analyzed for this study can be found in the Healthcare Cost and Utilization Project (HCUP) registry at https://www.hcup-us.ahrq.gov.
Not applicable.
© The Author(s) 2023.
Copyright: © The Author(s) 2023. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
