Affiliation:
1Department of Internal Medicine, Rheumatology Unit, San Fernando General Hospital, San Fernando, Trinidad and Tobago
Email: dr.esthermd21@gmail.com
ORCID: https://orcid.org/0009-0000-4252-5970
Affiliation:
1Department of Internal Medicine, Rheumatology Unit, San Fernando General Hospital, San Fernando, Trinidad and Tobago
ORCID: https://orcid.org/0000-0001-6994-7014
Affiliation:
2Policy Planning and Research, Southwest Regional Health Authority, San Fernando General Hospital, San Fernando, Trinidad and Tobago
ORCID: https://orcid.org/0000-0002-4518-7337
Explor Digit Health Technol. 2025;3:101152 DOI: https://doi.org/10.37349/edht.2025.101152
Received: January 27, 2025 Accepted: May 12, 2025 Published: June 09, 2025
Academic Editor: Mirko Casu, University of Catania, Italy; Atanas G. Atanasov, Medical University of Vienna, Austria
Aim: To explore patient satisfaction with telemedicine and its associated factors at the Rheumatology Outpatient Clinic, San Fernando Teaching Hospital (SFTH), and to determine patient preference for health-related consultations.
Methods: 305 patients were surveyed via consecutive sampling. Data was obtained via interviewer-administered questionnaires in a clinical setting, capturing demographics, challenges with face-to-face consultations, and patient perspectives on telemedicine. Items from the Telemedicine Satisfaction Questionnaire and Telehealth Usability Questionnaire were modified to capture impact. Data was analyzed using descriptive and inferential statistics (SPSS version 29).
Results: Most respondents were ≥ 40 years old (77.7%), Indo-Caribbean (66.2%), female (89.2%), unemployed (64.9%), and had secondary level education or higher (76.1%). Time off issues (13.0%), timing inconvenience (12.4%), and traveling costs (12.4%) were identified as challenges with face-to-face consultations. Fear of interaction (22.9%) and financial difficulty (22.7%), widely resulting from COVID-19, were additional challenges. Most patients reported satisfaction with telemedicine (71.5%), relating to easier access to health services (65.9%). Combined telemedicine and face-to-face consultations, as appropriate, were the most preferred option (73.4%). Several socio-demographic factors influenced patient satisfaction and preference for telemedicine services, with telemedicine convenience being the most significant factor.
Conclusions: The results conclude that patients at the Rheumatology Outpatient Clinic are satisfied with the current telemedicine service as a method of providing continuity of care (p < 0.001). Challenges encountered with face-to-face consultations and the COVID-19 pandemic can influence patients’ level of satisfaction with and preference for telemedicine. Telemedicine convenience was the most significant factor influencing patient satisfaction and preference (p < 0.001). Most patients’ preference for a combination approach of both telemedicine and face-to-face consultations reflects the current standard of care. The findings of this study suggest that telemedicine is reasonable to incorporate into outpatient care for patients with chronic rheumatological diseases.
The rapid advancement of technology has revolutionized the healthcare industry, with telemedicine emerging as a transformative approach to healthcare delivery [1]. Telemedicine, which can be defined as the utilization of telecommunication technologies to support the delivery of medical, diagnostic, and treatment-related services remotely [2], has the potential to improve patient access to care, enhance the quality of services provided, and increase patient satisfaction [3].
The advent of COVID-19 brought with it several challenges to the healthcare system both locally and internationally. These challenges included reduced access to care, the postponement and cancellation of services deemed less urgent, increased physical barriers to communication, e.g., social distancing and mask-wearing, stay-at-home orders, curfews, and the avoidance of health facilities in fear of contracting the virus, to name a few [4]. The rise of social isolation also led to the rise of technological advancements to overcome these obstacles. Telemedicine has seen a dramatic surge in utilization during the COVID-19 pandemic as outpatient clinics sought to maintain continuity of care while mitigating the risks of in-person visits [5]. According to the Pan American Health Organization (PAHO), “Telemedicine enables many of the key clinical services to continue to operate regularly and without interruption in the course of a public health emergency” [6]. This rapid shift regarding the increased utilization of telemedicine services has highlighted the need to thoroughly examine patient satisfaction with telemedicine, as patient satisfaction is an important and commonly used indicator for measuring the quality of health care and has become an increasingly integral component of modern healthcare delivery [7].
In Trinidad and Tobago, telemedicine/teleconsultations have served as the main method adopted across many public and private healthcare institutions to provide continuity of care in the face of the COVID-19 pandemic. There are many reasons why patients may opt for telemedicine vs regular face-to-face consultations, including convenience, availability, physical illness, fear of contagion, distance, etc. [8]. Some patients may voice a combination of these reasons. It is therefore important to investigate these from a patient perspective to ascertain the potential benefits, quality of life improvements, and suitability of telemedicine in patient care. In Trinidad and Tobago, the scope of telemedicine in patient care is yet to be fully surveyed, and hence, there may exist a need for the adoption of suitable policies to be engraved in health care. A previous study done locally investigating the effectiveness of telemedicine in primary care revealed that telemedicine may not be inferior to usual care [9]. This study, however, will seek to determine the level of patient satisfaction with telemedicine and its associated factors, patient preference for health-related consultations, and the practicality of the adoption of telemedicine in providing continuity of care in a post-pandemic setting.
A cross-sectional, descriptive study comprising 305 patients gathered via consecutive sampling at the Rheumatology Outpatient Clinic was conducted. All patients ≥ 18 years of age, willing to participate, patients with independent cognitive ability, and those who have previously had a teleconsultation were included. On average, there are 50 patients scheduled per week on a Thursday for the Rheumatology Outpatient Clinic. Over a 4-month period, approximately 800 rheumatology patients would be seen at the clinic. Instead of sampling the full 800 patients, a sample size formula was used to generate the sample size as follows:
Where N is the population size = 800 = the total number of patients over a 4-month period; Z = 1.96 = Z-score at 95% confidence interval (CI); e = margin of error = 5% = 0.05 (mostly used margin of error for the given formula, chosen for increased accuracy); p = proportion = 0.5 (commonly used in statistical calculations for survey populations).
This, when the above values are input into a statistical calculator, gives an estimated sample size of 260 patients for the 4-month period.
The respective weekly Rheumatology Outpatient Clinic listings were utilized to identify all patients scheduled each week over the 16-week period in question from 1 February to 23 May 2024. Patients were engaged in a routine telemedicine consultation prior to their clinic visit and were not informed of the study until the day of the clinic visit to eliminate bias. The aim was to gather at least 17 patient responses each week over the 16-week period. Patients under 18 years of age, those who declined to participate, and patients who would not have previously had a telemedicine consultation were excluded. Patients with cognitive impairment who were unable to independently give their feedback were also excluded from the study.
At the end of the 4-month period in question, 320 patients were recruited instead of the 260 calculated as the sample size. This was due largely to the eagerness of patients at the clinic to participate in the survey on a weekly basis during the time that the surveys were being administered, i.e., within the first three-hour window, 7 am–10 am. The authors did not wish to refuse patients to right to participate. Additionally, more patients were recruited than the calculated sample size in efforts to increase the generalisability of the findings and to compensate for potential issues that may have arisen, e.g., incomplete surveys.
The telemedicine service for rheumatology outpatients is strictly audio-based and mainly synchronous via dedicated telephones without a visual component. Patients are usually contacted the week prior to their clinic appointment, and the patient-physician interaction is then transcribed into an electronic health record module specifically dedicated to the clinic via the Cellma RioMed platform. Patients are usually contacted a week in advance in order to review lab tests, medication, symptomatology, and concerns, facilitating easier consultations on the day of their scheduled visit. Electronic prescriptions, necessary e-referrals, and additional laboratory test requests are also generated prior to their clinic visit. Patients are usually given the option of attending the clinic visit or collecting the documents generated from the teleconsultation with their next appointment from the clinic clerk. Patients who are identified as having moderate-severe disease flares via teleconsultation are addressed prior to the clinic visit by either instructing patients to adjust medication dosages, adding new medications for collection to the prescriptions, or advising the patient to utilize the accident and emergency services. On the day of the clinic visit, doctors would enter the patient’s hospital registration number into the Cellma RioMed platform, where the prior patient-physician interaction can be seen via the electronic health record. The physician revisits the prior teleconsultation, addresses any new concerns, and the patient is then invited to have their next appointment booked by clerical staff. Prior telemedicine consultations can reduce a clinic visit to less than 5 minutes. First-time patients are not assessed via telemedicine and were excluded from the study. Additionally, rheumatology outpatients who do not have a clinic appointment on said Thursdays usually register their names and contact information via clerical staff for doctors to contact should they have a concern or a new laboratory/radiological result to discuss at a later date.
The sample size was calculated as 260 patients from the preceding formula. A total of 320 patients were recruited whom 7 patients declined to participate who initially agreed, and 8 patients did not complete the survey, causing the remaining number of patients retained to be 305 (Figure 1).
Data was collected via interviewer-administered questionnaires in a clinic setting comprising 38 items capturing socio-demographic information (Questions 1–7), medical history (Question 8), patient support system (Questions 9–11) challenges faced during COVID-19 and in attending face-to-face consultations (Questions 12–13), patient preference (Question 20), and patient perspective on the current telemedicine service at the Rheumatology Outpatient Clinic (Questions 14–38; Questions 21–38 measured responses on a 5-point Likert scale). Questions from two of the most widely used and previously validated questionnaires—The Telemedicine Satisfaction Questionnaire and the Telehealth Usability Questionnaire were utilized and improved upon to capture the impact of telemedicine [10–12].
Data was entered and analyzed using IBM Statistical Package for the Social Sciences (SPSS) version 29.0. Descriptive and inferential methods were used in data analysis. Analyses included tests employed for non-parametric data, which consisted of Kruskal-Wallis tests, Spearman’s rho, Mann-Whitney U tests, Chi-Squared tests of association and independence, and ordinal logistic regression. Both ordinal and numerical data were generated for analysis, and p-values < 0.05 were considered statistically significant.
The average age of participants was 51.36 years. There were several mode ages or the most frequent ages of persons in the study were 53 years and 56 years. Table 1 shows the socio-demographic findings that follow. In terms of clinical data, patients were asked about the length of time they had been members of the clinic. Most patients were in the clinic for more than 2 years (Table 2). Since the clinic has been conducting telemedicine services for over 3 years, this implies that most patients would have had sufficient exposure to the telemedicine service. For patient diagnoses, participants were given 10 response options and a choice option to write the diagnosis if it was not listed. There was a total of 350 responses from 305 participants, which indicated that some participants did identify more than one diagnosis. There was a higher frequency of rheumatoid arthritis (RA) followed by systemic lupus erythematosus (SLE) (Table 2). The term “Connective Tissue Disease” covered patients with Sjogren’s syndrome, scleroderma, mixed connective and undifferentiated connective tissue disease. Questions 10 and 11 enquired of the level of patient support required and the degree of assistance obtained in the form of either public assistance or disability grants (Table 3).
Patient socio-demographic characteristics
| Variable | Value | Total | Percentage* |
|---|---|---|---|
| Sex | Male | 33 | 10.8% |
| Female | 272 | 89.2% | |
| Age | 17–19 | 9 | 3.0% |
| 20–29 | 21 | 6.9% | |
| 30–39 | 38 | 12.5% | |
| 40–49 | 50 | 16.4% | |
| 50–59 | 84 | 27.5% | |
| 60–69 | 78 | 25.6% | |
| 70–79 | 23 | 7.5% | |
| 80–89 | 2 | 0.7% | |
| Ethnicity | African | 52 | 17.0% |
| Chinese | 1 | 0.3% | |
| Hispanic | 3 | 1.0% | |
| Indo-Caribbean | 202 | 66.2% | |
| Mixed | 46 | 15.1% | |
| No response | 1 | 0.3% | |
| Employment status | Unemployed | 198 | 64.9% |
| Employed | 88 | 28.9% | |
| Part-time | 5 | 1.6% | |
| Student | 8 | 2.6% | |
| Retired | 2 | 0.7% | |
| No response | 4 | 1.3% | |
| Education level | Primary | 63 | 20.7% |
| Secondary | 146 | 47.9% | |
| Tertiary | 86 | 28.2% | |
| None | 7 | 2.3% | |
| No response | 3 | 1.0% |
* Percentages rounded off to 1 decimal place
Patient clinical data
| Variable | Value | Total | Percentage* |
|---|---|---|---|
| Longevity in clinic | ≤ 6 months | 19 | 6.2% |
| 7–12 months | 29 | 9.5% | |
| 13–18 months | 14 | 4.6% | |
| 19–24 months | 13 | 4.3% | |
| > 24 months | 228 | 74.8% | |
| No response | 2 | 0.7% | |
| Patient diagnoses | Rheumatoid arthritis | 127 | 36.3% |
| Systemic lupus erythematosus | 76 | 21.7% | |
| Connective tissue disease | 52 | 14.9% | |
| Undifferentiated inflammatory arthritis | 16 | 4.6% | |
| Psoriatic arthritis | 14 | 4.0% | |
| Gout | 11 | 3.1% | |
| Vasculitis | 12 | 3.4% | |
| Myositis | 6 | 1.7% | |
| Polymyalgia rheumatica | 2 | 0.6% | |
| Discoid lupus | 1 | 0.3% | |
| Osteoporosis | 1 | 0.3% | |
| Interstitial lung disease | 1 | 0.3% | |
| Undiagnosed | 27 | 7.7% | |
| No response | 4 | 1.1% |
* Percentages rounded off to 1 decimal place
Patient support
| Variable | Value | Total | Percentage* |
|---|---|---|---|
| Assistance required with daily activities? | Yes | 81 | 26.6% |
| No | 221 | 72.5% | |
| No response | 3 | 1.0% | |
| Grant recipient? | Yes | 60 | 19.7% |
| No | 241 | 79.0% | |
| No response | 4 | 1.3% |
* Percentages rounded off to 1 decimal place
When asked to identify challenges associated with face-to-face visits (Table 4), most participants identified one challenge (n = 192; 63.0%), followed by two challenges (n = 64; 21.0%). In sum, 437 responses were recorded to the question. Some participants identified more than one challenge; hence, the total number of responses does not equal the total number of participants. The highest number of responses reflected having no challenges (n = 72; 16.5%). The most frequently stated challenges were ‘time off issues’ (n = 57; 13.0%), ‘timing inconvenience’ (n = 54; 12.4%), and ‘traveling costs’ (n = 54; 12.4%). Patients were also asked to identify some of the negative effects faced as a result of the COVID-19 pandemic that may have affected their health (Table 4). Participants were given responses from which to select and were asked to select all that applied. A total of 450 responses were recorded from the 305 participants. The most frequent response was ‘fear of interaction’ (n = 103; 22.9%). The second most frequent response was ‘financial difficulty’ (n = 102; 22.7%).
Challenges with face-to-face visits and the effect of COVID-19
| Variable | Value | Total | Percentage* |
|---|---|---|---|
| Challenges with face-to-face visits | None | 72 | 16.5% |
| Time off issues | 57 | 13.0% | |
| Timing inconvenience | 54 | 12.4% | |
| Travelling costs | 54 | 12.4% | |
| Physical illness/disability | 46 | 10.5% | |
| Financial constraints | 42 | 9.6% | |
| Needed company | 34 | 7.8% | |
| Safety concerns | 21 | 4.8% | |
| Fear of contagion | 18 | 4.1% | |
| Weather uncertainty | 18 | 4.1% | |
| Parking | 5 | 1.1% | |
| No response | 16 | 3.7% | |
| Effect of COVID-19 | No effect | 164 | 53.8% |
| Mostly negative | 124 | 40.7% | |
| Benefitted | 12 | 3.9% | |
| No response | 5 | 1.6% | |
| COVID-19 negative effects | Fear of interaction | 103 | 22.9% |
| Financial difficulty | 102 | 22.7% | |
| None | 69 | 15.3% | |
| Illness | 59 | 13.1% | |
| Depression/apathy | 45 | 10.0% | |
| Loss of job | 22 | 4.9% | |
| Breakdown of family structure | 17 | 3.8% | |
| Business closure | 10 | 2.2% | |
| Death of breadwinner | 10 | 2.2% | |
| Eviction | 1 | 0.2% | |
| No response | 12 | 2.7% |
* Percentages rounded off to 1 decimal place
Participants were asked whether telemedicine made it easier for them to access health services. Most of the respondents said ‘yes’ (n = 201; 65.9%). Patients were also asked whether they remembered they had a clinic appointment. Most respondents said ‘yes’ (n = 286; 93.8%). Patients who were reminded of their clinic appointment via telemedicine consisted of the remaining (n = 19; 6.2%).
Participants were then asked a series of Questions, 21 to 38, on a 5-point Likert scale. The percentage for each response follows (Table 5).
Responses on a 5-point Likert scale
| Statement | Strongly agree | Agree | Neither agree nor disagree | Disagree | Strongly disagree | No response |
|---|---|---|---|---|---|---|
| 21. I was surprised to be contacted via telephone for a rheumatology consult. | 20.7% | 41.6% | 16.7% | 14.8% | 5.2% | 1.0% |
| 22. I think telemedicine consults serve the same purpose as face-to-face visits. | 15.1% | 35.7% | 19% | 24.3% | 5.9% | - |
| 23. Telemedicine is more convenient for me. | 21.3% | 39.7% | 23.0% | 12.8% | 3.2% | - |
| 24. I felt that I needed to see my healthcare provider in person. | 23.3% | 46.6% | 19.7% | 7.4% | 3.0% | - |
| 25. My concerns were addressed via telemedicine. | 14.4% | 46.6% | 25.2% | 11.1% | 2.0% | 0.7% |
| 26. The audio quality was sufficient. | 29.2% | 61.3% | 6.2% | 2.3% | 1.0% | - |
| 27. The teleconsult was of sufficient length. | 24.3% | 62.6% | 8.2% | 3.6% | 1.3% | - |
| 28. The staff was courteous and willing to address my concerns. | 32.8% | 57.4% | 7.2% | 1.3% | 1.3% | - |
| 29. I experienced technical difficulties during the teleconsult. | 3.3% | 8.2% | 8.8% | 55.4% | 24.3% | - |
| 30. I am not easily accessible via phone. | 6.2% | 15.4% | 14.8% | 43.3% | 20.3% | - |
| 31. I have no issues with collecting my prescriptions/documents after a telemedicine consult. | 32.1% | 50.5% | 6.9% | 6.9% | 3.3% | 0.3% |
| 32. My doctor uses information from the telemedicine system in my office visits. | 15.0% | 38.7% | 39.0% | 3.3% | 2.6% | 1.4% |
| 33. I follow my doctor’s advice better since working with the telemedicine system. | 12.5% | 27.2% | 50.5% | 8.2% | 1.6% | - |
| 34. I do not know much about technology. | 7.5% | 27.2% | 18.7% | 26.3% | 20.3% | - |
| 35. I am more involved in my care using the telemedicine system. | 9.2% | 21.6% | 48.9% | 15.1% | 4.6% | 0.6% |
| 36. I am satisfied with the current telemedicine service in the rheumatology clinic. | 19.3% | 52.2% | 20.0% | 6.2% | 2.3% | - |
| 37. I would opt for telemedicine for most of my future consults. | 20.3% | 39.3% | 20.7% | 14.1% | 5.6% | - |
| 38. I would recommend an improved telemedicine service as the way going forward. | 14.1% | 32.1% | 18.0% | 14.8% | 21.0% | - |
-: Not applicable
Most questions were structured in such a way that if someone wanted to give a positive response (based on his/her assessment of the statement), strongly agree or 1 was selected. However, some questions were written in reverse, in that positive responses to the statement resulted in the selection of strongly disagree or 5; these questions were reverse-coded. This reverse coding of questions became a limitation of the study as it affected the internal reliability of the scale, i.e., whether the questions in the scale reliably captured concerns relating to telemedicine satisfaction. The questions that were reverse-coded were Questions 24, 29, 30, and 34. The Cronbach’s alpha was 0.441 for the 18 items on the scale. Questions 22, 23, 26, 27, 28, and 37 came from either the telehealth questionnaire or the telehealth usability questionnaire.
Patient satisfaction was assessed with several statements on the questionnaire. Question 30 asked patients whether they were easily accessible by phone. Most patients collectively disagreed (whether disagreed or strongly disagreed) that they were not easily accessible by phone (n = 194; 63.6%), whereas (n = 66; 21.6%) of patients collectively agreed that they were not easily accessible via phone. Forty-five patients, or 14.8%, were neutral to this question. The statements that were determined to have significance in assessing patient satisfaction with the telemedicine service via Kruskal-Wallis tests in relation to phone accessibility were (Table 6):
Questions assessing patient satisfaction with telemedicine in relation to phone accessibility
| Question/Statement | Kruskal-Wallis H test value | p-value | Mean rank | |
|---|---|---|---|---|
| 24 | 10.17 | 0.038 | Strongly agree | 113.89 |
| Agree | 142.55 | |||
| Neither agree nor disagree | 138.62 | |||
| Disagree | 158.36 | |||
| Strongly disagree | 171.93 | |||
| 26 | 21.44 | < 0.001 | Strongly agree | 106.68 |
| Agree | 167.62 | |||
| Neither agree nor disagree | 162.51 | |||
| Disagree | 164.71 | |||
| Strongly disagree | 124.27 | |||
| 27 | 17.32 | 0.002 | Strongly agree | 119.55 |
| Agree | 172.64 | |||
| Neither agree nor disagree | 153.87 | |||
| Disagree | 163.34 | |||
| Strongly disagree | 125.73 | |||
| 28 | 31.99 | < 0.001 | Strongly agree | 107.03 |
| Agree | 175.51 | |||
| Neither agree nor disagree | 162.28 | |||
| Disagree | 167.17 | |||
| Strongly disagree | 113.12 | |||
| 36 | 31.35 | < 0.001 | Strongly agree | 115.42 |
| Agree | 169.38 | |||
| Neither agree nor disagree | 188.71 | |||
| Disagree | 159.55 | |||
| Strongly disagree | 112.24 | |||
Question/Statement 24: I felt that I needed to see my healthcare provider in person.
Question/Statement 26: The audio quality was sufficient.
Question/Statement 27: The teleconsult was of sufficient length.
Question/Statement 28: The staff was courteous and willing to address my concerns.
Question/Statement 36: I am satisfied with the current telemedicine service in the rheumatology clinic.
Spearman’s rho correlations were done for Questions/Statements 24, 26, 27, 28, and 36 to determine if there was any relationship between them (Table 7). Relationships were found for:
Relationships between questions that assess patient satisfaction with telemedicine
| Correlations | Question/Statement 24 | Question/Statement 26 | Question/Statement 27 | Question/Statement 28 | Question/Statement 36 | ||
|---|---|---|---|---|---|---|---|
| Spearman’s rho | Question/Statement 24 | Correlation coefficient | 1.000 | –0.141* | –0.229** | ||
| Sig. (2-tailed) | 0.013 | < 0.001 | |||||
| N | 305 | 305 | 305 | ||||
| Question/Statement 26 | Correlation coefficient | 1.000 | 0.678** | 0.576** | 0.405** | ||
| Sig. (2-tailed) | < 0.001 | < 0.001 | < 0.001 | ||||
| N | 305 | 305 | 305 | 305 | |||
| Question/Statement 27 | Correlation coefficient | –0.141* | 0.678** | 1.000 | 0.642** | 0.519** | |
| Sig. (2-tailed) | 0.013 | < 0.001 | < 0.001 | < 0.001 | |||
| N | 305 | 305 | 305 | 305 | 305 | ||
| Question/Statement 28 | Correlation coefficient | 0.576** | 0.642** | 1.000 | 0.437** | ||
| Sig. (2-tailed) | < 0.001 | < 0.001 | < 0.001 | ||||
| N | 305 | 305 | 305 | 305 | |||
| Question/Statement 36 | Correlation coefficient | –0.229** | 0.405** | 0.519** | 0.437** | 1.000 | |
| Sig. (2-tailed) | < 0.001 | < 0.001 | < 0.001 | < 0.001 | |||
| N | 305 | 305 | 305 | 305 | 305 | ||
* Correlation is significant at the 0.05 level (2-tailed); ** correlation is significant at the 0.01 level (2-tailed); N: number of patients; Sig: significance
Questions/Statements 24 & 27
Questions/Statements 24 & 36
Questions/Statements 26 & 27
Questions/Statements 26 & 28
Questions/Statements 26 & 36
Questions/Statements 27 & 28
Questions/Statements 27 & 36
Questions/Statements 28 & 36
Kruskal-Wallis tests were done to determine the factors that affected or influenced patient satisfaction with the telemedicine service. The independent variables were ethnicity, marital status, employment status, education level, time at the clinic, the effects of the pandemic, and convenience of telemedicine. There were many responses for age, and as such, the 10-year age groups were used for the analysis. The results for age were not significant. Significant results are reflected in Table 8. The results indicate that Statement 23, “Telemedicine is more convenient for me”, had the greatest influence on patient satisfaction.
Factors associated with patient satisfaction with telemedicine
| IV | DV | Kruskal-Wallis H test | df | p-value | Mean rank | |
|---|---|---|---|---|---|---|
| Marital status | Q/S 28 | 14.65 | 4 | 0.005 | Common law | 161.70 |
| Divorced/separated | 126.95 | |||||
| Married | 144.23 | |||||
| Single | 166.92 | |||||
| Widowed | 146.91 | |||||
| Employment status | Q/S 24 | 10.31 | 4 | 0.036 | Employed | 164.59 |
| Part-time | 221.00 | |||||
| Retired | 219.75 | |||||
| Student | 166.06 | |||||
| Unemployed | 141.89 | |||||
| Education level | Q/S 24 | 8.58 | 3 | 0.035 | None | 80.93 |
| Primary | 139.91 | |||||
| Secondary | 152.40 | |||||
| Tertiary | 164.20 | |||||
| Pandemic effect | Q/S 27 | 8.41 | 2 | 0.015 | Benefitted | 165.00 |
| Mostly negatively | 164.17 | |||||
| No effect | 139.10 | |||||
| Pandemic effect | Q/S 36 | 8.04 | 2 | 0.018 | Benefitted | 145.79 |
| Mostly negatively | 165.97 | |||||
| No effect | 139.15 | |||||
| Q/S 23 | Q/S 28 | 39.70 | 4 | < 0.001 | SA | 178.14 |
| A | 193.45 | |||||
| NAND | 169.40 | |||||
| D | 159.86 | |||||
| SD | 101.27 | |||||
| Q/S 23 | Q/S 36 | 88.62 | 4 | < 0.001 | SA | 269.90 |
| A | 207.85 | |||||
| NAND | 185.14 | |||||
| D | 139.11 | |||||
| SD | 93.35 | |||||
IV: independent variable; DV: dependent variable; df: degrees of freedom; Q/S: Question/Statement; SA: strongly agree; A: agree; NAND: neither agree nor disagree; D: disagree; SD: strongly disagree
The Mann-Whitney U test was used to determine if sex, whether participants had a physical disability or not, whether persons had financial difficulties or not, and whether participants had time off issues or not, affected patient satisfaction. The test also tells if there are differences between the two categories of responses. Sex was significant. Therefore, there were significant differences between both sexes for Question/Statement 36, U = 3,400.000, p = 0.013, with higher observation in females. Additionally, there was a significant result for whether participants got time off or not, U = 5,099.000, p = 0.001, with higher observation in persons who did not get time off.
Chi-Squared tests of Independence were done to determine if there were relationships between Statement 19 (Table 9), “How would you describe your experience with your clinic visit today?” and the statements that assessed patient satisfaction. Significant results were found for the following:
Relationship between clinic experience and patient satisfaction
| Questions/Statements | Chi-Squared, χ2 | p-value |
|---|---|---|
| 19 & 27 | 36.535 | 0.002 |
| 19 & 28 | 46.745 | < 0.001 |
| 19 & 36 | 26.544 | 0.047 |
Statement 27: The teleconsultation was of sufficient length.
Statement 28: The staff was courteous and willing to address my concerns.
Statement 36: I am satisfied with the current telemedicine service in the rheumatology clinic.
To determine the factors that predicted patient satisfaction with telemedicine, an Ordinal Logistic Regression was done. The dependent variable or the criterion variable used was Question/Statement 36 since it directly asked participants about their degree of satisfaction with the overall current telemedicine service, whereas the other Questions/Statements asked participants about aspects or components of the telemedicine service. The independent or predictor variables were age, sex, ethnicity, level of education, marital status, employment status, number of diagnoses, number of challenges, assistance with daily management of illness, the effect of the COVID-19 pandemic, convenience of telemedicine, type of patient and patients’ experiences at the clinic on the day they were asked to participate in the study. The Chi-Squared Goodness-of-Fit test was not significant. Therefore, the overall model was not significant. However, some of the variables were predictors of patient satisfaction. The results showed that being male predicted satisfaction with telemedicine. The odds ratio was 2.760 (95% CI, 1.267 to 6.010), Wald χ2 = 6.536, p = 0.012. Another significant predictor was ethnicity, specifically for Chinese participants. The odds ratio was 213.440 (95% CI, 1.409 to 32,334.462), Wald χ2 = 4.384, p = 0.023. Question/Statement 23: “Telemedicine is more convenient for me” was also found to be a predictor. All the responses, except ‘strongly disagree’, were significant (Table 10).
Relationship of telemedicine convenience to patient satisfaction
| Question/Statement 23 | Chi-Squared, χ2 | p-value |
|---|---|---|
| Strongly agree | 72.000 | < 0.001 |
| Agree | 48.155 | < 0.001 |
| Neither agree nor disagree | 23.954 | < 0.001 |
| Disagree | 14.215 | < 0.001 |
To determine patients’ preference for consultations, whether face-to-face or telemedicine, participants were asked Question 20: Please indicate your preference below for health-related consults, with response options of ‘waiting to see a doctor’, ‘telemedicine consults’, and ‘both telemedicine and face-to-face consult as appropriate’. The results are shown in Figure 2.
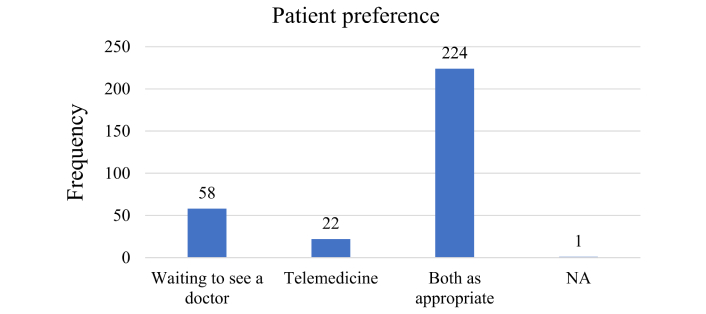
Patient preference for consultations at the Rheumatology Outpatient Clinic. NA: no answer
Kruskal-Wallis tests were done to determine the factors that affected telemedicine preference. The independent variables were ethnicity, marital status, employment status, education level, time at the clinic, the effects of the pandemic, and convenience of telemedicine. Significant results were found for educational level, χ2 = 10.995, p = 0.012 (Table 11). Tertiary-level education was the strongest response that affected preference.
Relationship between education level and patient preference
| Question/Statement | Education level | N | Mean rank |
|---|---|---|---|
| 20 | None | 7 | 130.71 |
| Primary | 63 | 141.49 | |
| Secondary | 146 | 145.02 | |
| Tertiary | 86 | 171.52 | |
| Total | 302 |
3 persons did not answer, accounting for a total of 305 persons surveyed. N: number of patients
Significant results were also found for convenience of telemedicine and preference, χ2 = 33.401, p < 0.001, where persons who were neutral as to whether they thought telemedicine was convenient or not, preferred both telemedicine and face-to-face consultations (Table 12). Due to the many responses for age, the age groups were used for the analysis. The groups were based on 10-year periods. The results were not significant.
Relationship of telemedicine convenience to patient preference
| Question/Statement | Question/Statement 23 | N | Mean rank |
|---|---|---|---|
| 20 | 1 | 65 | 116.96 |
| 2 | 121 | 166.71 | |
| 3 | 70 | 173.96 | |
| 4 | 39 | 141.88 | |
| 5 | 10 | 118.00 | |
| Total | 305 |
1: strongly agree; 2: agree; 3: neutral; 4: disagree; 5: strongly disagree; N: number of patients
To determine the factors that predicted telemedicine preference, an Ordinal Logistic Regression was done. Question/Statement 20: “Please indicate your preference for health-related consults” was the criterion variable and the predictor variables were age, sex, ethnicity, level of education, marital status, employment status, number of diagnoses, number of challenges, assistance with daily management of illness, the effect of the COVID-19 pandemic, type of patient and patients’ experiences at the clinic on the day they were asked to participate in the study. The Chi-Squared Goodness-of-Fit test was significant, χ2 = 2,030.787, p < 0.001. While the Deviance Goodness-of-Fit test (which assesses a lack of fit) was not significant, D = 409.378, p = 1.000. Therefore, the model is significant, and there are predictors of the criterion in the model. The Nagelkerke’s R2 for the model was 0.166. It means that 16.6% of the model predicts the criterion variable, preference for telemedicine, which is significant. The results showed that the response category of ‘both as appropriate’ was significant for the dependent variable. The odds ratio was 9,082 (95% CI, 22.402 to 368,2354.347), Wald χ2 = 8.849, p = 0.023. With regards to the predictors, the effects of the pandemic were the only predictors of preference for telemedicine. The odds of patients who were negatively affected by the pandemic and preferred both face-to-face and telemedicine consults were 21.145 (95% CI, 2.792 to 160.143), Wald χ2 = 8.726, p = 0.011.
Patient compliance was measured with Question/Statement 33: “I follow my doctor’s advice better since working with the telemedicine system”. Chi-Squared tests of Independence were done to determine if the Question/Statement was related to patient satisfaction with telemedicine services (Questions/Statements 24, 26, 27, 28, and 36). It was found that only Question/Statement 36: “I am satisfied with the current telemedicine service in the rheumatology clinic” was related to Question/Statement 33, χ2 = 246.765, p < 0.001 (Table 13). Hence, there was an inter-dependent relationship—the more patients were satisfied with the current telemedicine service, the more they followed their doctor's advice since they began using the telemedicine system.
Relationship between patient compliance and patient satisfaction with telemedicine
| Chi-Square tests | Value | df | Asymptotic significance (2-sided) |
|---|---|---|---|
| Pearson Chi-Square | 246.765 | 16 | < 0.001 |
| Likelihood Ratio | 124.719 | 16 | < 0.001 |
| Linear-by-Linear Association | 70.707 | 1 | < 0.001 |
| Number of valid cases | 305 |
df: degrees of freedom
Finally, there was also a significant effect of patient preference on compliance with doctor’s advice when conducting Kruskal-Wallis tests with Questions 33 and 20, χ2 = 10.245, p = 0.006. When considering mean ranks, the response of ‘both as appropriate’ had the greatest influence on patient compliance (Table 14).
Relationship between patient preference and compliance
| Question/Statement | Question/Statement 20 | N | Mean rank |
|---|---|---|---|
| 33 | Telemedicine | 22 | 100.07 |
| Waiting to see a doctor | 58 | 151.47 | |
| Both as appropriate | 224 | 157.92 | |
| Total | 304 |
1 person gave no response, bringing the total to 305. N: number of patients
Questions/Statements 29, 30, 31, and 38 were examined to determine if they could provide insight into possible limitations of telemedicine within the Rheumatology Service at San Fernando Teaching Hospital (SFTH).
Statement 29: I experienced technical difficulties during the teleconsultation.
Statement 30: I am not easily accessible via phone.
Statement 31: I have no issues with collecting my prescriptions/documents after a telemedicine consult.
Statement 38: I would recommend an improved telemedicine service as the way going forward.
Several Chi-Squared tests of Independence were done to determine if there were relationships between the aforementioned Questions/Statements and preferences. The results and the frequencies were used to determine if any limitations existed for the use of telemedicine for the Rheumatology Service at the SFTH. A Chi-Squared test of Independence was done to determine if there was a relationship between Question/Statement 29 and Question/Statement 20. The results were significant, χ2 = 40.877, p < 0.001. For the frequency of Question/Statement 29, most respondents ‘disagreed’ (169 persons or 55.4% of respondents). A Chi-Squared test of Independence was also done to determine if there was a relationship between Question/Statement 30 and Question/Statement 20. The results were also significant, χ2 = 30.105, p = 0.003. For the frequency, most collectively disagreed (whether disagreed or strongly disagreed) with Question/Statement 30 (n = 194 persons or 63.6% of respondents). With regards to Question/Statement 31, most respondents collectively agreed (whether agreed or strongly agreed) that they would willingly collect their prescriptions/documents after a telemedicine consult (n = 252 persons or 82.6% of respondents). The results for the Chi-Squared test of Independence with Question/Statement 20 were significant, χ2 = 31.788, p = 0.007. Finally, Question/Statement 38 ascertained whether participants would recommend an ‘improved’ telemedicine service. Most respondents collectively agreed (n = 141 persons or 46.2% of respondents). In terms of the results for the Chi-Squared test of Independence, the results were significant, χ2 = 44.376, p < 0.001.
This study explored the various challenges experienced by patients in attending face-to-face consultations, their perception of the current telemedicine service at the outpatient clinic, and the factors that may have affected patients’ level of satisfaction with and preference for telemedicine services. The most frequent challenges described by patients regarding physical consultations reflected difficulties with receiving time off, costs of traveling, and inconvenience in timing. The COVID-19 pandemic also added insult to injury by contributing to patient reluctance for face-to-face consultations, either due to fear of contracting COVID-19 or increased financial difficulty, which was reflected in this study. Previous studies highlighting the increasing role of telemedicine in rheumatology as a method of providing continuity of care in the post-pandemic period cited an increased preference for telemedicine for patients who had a long commute or those who were reluctant to attend in-person consultations due to the fear of contracting COVID-19 [13–15]. In terms of variables that predicted patients’ preference for telemedicine vs. face-to-face consultation, the effect of the pandemic in terms of patients who stated the pandemic had negative consequences for them was more likely to prefer both telemedicine and physical consultations as deemed appropriate.
Patient’s perception of telemedicine in this study was mostly positive, as reflected by the percentage of patients directly stating they were satisfied with the current telemedicine service, opining that it granted them easier access to health services. It is interesting, however, that although most patients felt the need to see their healthcare provider in person, most also acknowledged that their concerns could have been addressed by telemedicine. Socio-demographic factors affecting patient satisfaction and preference for telemedicine included marital status, sex, employment status, educational level, the effect of the pandemic, convenience of telemedicine, whether patients felt their concerns were addressed, the length of a teleconsultation, and whether patients got time off or not. In terms of demographics, existing literature reveals a recurrent theme of the elderly population being very resistant to telemedicine, which may be due to a lack of literacy or increased morbidity [13, 16]. This study, however, did not find any significant impact of age differences influencing patient satisfaction with telemedicine. Patient satisfaction was predicted by sex, specifically males, which meant that males were more satisfied with the service than females. This finding may not be generalizable, seeing that 89% of participants were females. Ethnicity was also found to predict patient satisfaction, specifically, the Chinese ethnic group. This, however, may be subject to gender bias due to the small sample size, which may not have been representative. Existing studies agree that patients with higher educational literacy levels were more likely to prefer and utilize telemedicine services [13, 16, 17]. It is worth mentioning a previous study conducted in 2021 that highlighted the technological divide created by the implementation of telemedicine/telehealth services, augmenting ethnic/racial and socioeconomic disparities amongst patients needing care, where reduced access to telemedicine was rampant amongst minority groups [14]. Disparities among patients with accessing telemedicine services, however, were not explored in this study.
A significant finding was the factor of telemedicine convenience having the greatest effect on whether patients were satisfied or not with telemedicine, in that the more convenient the service was for patients, the more satisfied they were with it. The convenience of the service was also a predictor of patient satisfaction with telemedicine. For patient preference, it was found that education level, in this case, tertiary level education, and the convenience of telemedicine positively affected patients’ preference for telemedicine. For patients who opted to utilize telemedicine in the future, the main predictor was the convenience of telemedicine.
The finding that convenience largely affects patient satisfaction and preference for telemedicine is in keeping with previous studies. A recent systematic review and narrative analysis on telemedicine and patient satisfaction in 2017 highlighted high levels of patient satisfaction with telemedicine, citing factors for continued use, including improved outcomes, increased access to care, decreased traveling time, lower personal cost, improved communication, and patient empowerment [16]. On the contrary, additional studies showed that whilst patient satisfaction may be high regarding telemedicine services, no significant differences were reported for patient outcomes, including reduction in disease activity and quality of life, leading to the argument that telemedicine is both non-superior yet non-inferior to physical consultations [18, 19]. Regionally, a study conducted in Trinidad regarding telemedicine effectiveness for the management of chronic diseases at primary care facilities also highlighted non-inferiority [9]. Studies that may have deemed telemedicine services as inferior to in-person consultations, however, still acknowledge the convenience of telemedicine but opined that telemedicine is more suitable for patients with chronic diseases in a state of remission and not suitable for 1st visits [19–21]. This study largely investigated patients with chronic rheumatological diseases in an outpatient setting and did not include patients who were scheduled for an appointment at the clinic for their first visit. The level of disease activity was also not assessed in this study.
In terms of patient compliance, the main finding was that the more patients were satisfied with the current telemedicine service, the more they followed their doctor’s advice since they began using the telemedicine system. This finding is similar to previous studies where patient compliance was increased by a positive telemedicine experience [15, 16]. It was also found that patients who preferred both telemedicine and face-to-face visits as deemed appropriate were more likely to be compliant with their doctor’s advice.
Several limitations associated with observational studies also stand for this study conducted to evaluate patient satisfaction with telemedicine. Firstly, the study utilized convenience or consecutive sampling, which would have been easier to conduct but consisted of a non-randomized approach. This would have contributed to bias. Efforts were made to reduce sampling, survivorship, and volunteer bias by administering the survey to all patients present at the clinic who met the inclusion criteria during the 3-hour window period. Patients who refused to participate, those who did not attend the clinic on their appointment days (which may have included patients with severe disease activity who may have been warded or utilizing accident and emergency services), and patients attending the clinic after the 3-hour period when the surveys were conducted, contributed to non-response and under-coverage bias which served as limitations of the study. The sample size was also relatively small, and the study was conducted alongside usual face-to-face care, which may have influenced the results. Additionally, this study was conducted at a single site. This can affect the generalizability of the study as patient characteristics can differ based on the study site, affecting the results. For example, demographic data of patients may differ amongst locations in the southern territory as compared to centers located in central or northern areas. To date, few studies have been published reflecting the demographic data of patients with rheumatological diseases in the Caribbean however, studies conducted from Trinidad showed a similar demographic profile regarding a higher proportion of patients being female, with most patients being of East Indian, African, and Mixed ethnicities in the exact order of decreasing prevalence [22–24]. Currently, there exists global consensus regarding a higher prevalence of autoimmune diseases in females as compared to males [25, 26], which is reflected in this study.
With regards to possible limitations of telemedicine itself, patients may have given responses based on whether they experienced technical difficulties during the teleconsultation, whether they were easily accessible via phone, and whether they were digitally literate. Based on the percentages obtained, most patients did not encounter technical difficulties during their telemedicine consultations and were accessible via telephone. The digital literacy level of patients was not assessed. This study was also limited to telephone consultations and did not include video conferencing.
This study is the first in the Caribbean region that seeks to foster a higher level of insight into patient satisfaction with telemedicine services for outpatients. The findings are useful in analyzing the appropriateness of telemedicine for providing continuity of care should a future pandemic arise and for increased convenience in the post-pandemic period. The authors recommend that a multicentre study be conducted with a larger sample size to allow for generalizability. Further studies should also focus on both physician and patient interactions with telemedicine via various methods, including videoconferencing. Areas for future research also can include study designs to assess the potential of telemedicine in improving healthcare delivery in underserved communities, which may lead to improved healthcare outcomes for vulnerable populations. Finally, larger multicentre studies may allow for a set of criteria to be defined regarding the suitability of patients for telemedicine consultations vs physical face-to-face encounters for the region.
The results conclude that patients at the Rheumatology Outpatient Clinic are satisfied with the current telemedicine service as a method of providing continuity of care (p < 0.001). Several challenges associated with face-to-face consultations may influence patients’ preferred method of consultation. Amongst the socio-demographic factors affecting patient satisfaction and preference for telemedicine consultations, telemedicine convenience was the most significant influencer (p < 0.001), which agrees with the existing literature. The COVID-19 pandemic also significantly affected patients’ satisfaction and preference for telemedicine. Most patients’ preference for a combination approach of both telemedicine and face-to-face consultations reflects the current standard of care, which may need to be refined based on established criteria. The findings of this study suggest that telemedicine is reasonable to incorporate into outpatient care for patients with chronic rheumatological diseases.
CI: confidence interval
SFTH: San Fernando Teaching Hospital
The supplementary material for this article is available at: https://www.explorationpub.com/uploads/Article/file/101152_sup_1.pdf.
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
We would like to thank Mr. Daniel Cornwall for his assistance with data collection and data entry as a medical On-The-Job-Trainee.
ER: Conceptualization, Investigation, Methodology, Resources, Writing—original draft, Formal analysis, Project administration, Visualization, Writing—review & editing. HD: Conceptualization, Investigation, Methodology, Resources, Supervision. GR: Conceptualization, Methodology, Project administration, Validation, Supervision. All authors read and approved the submitted version.
The authors declare that they have no conflicts of interest.
This study was approved by the Bioethics Committee of the South West Regional Health Authority with reference/approval number 2023-09-18-14-17.
Informed consent to participate in the study was obtained from all participants.
Not applicable.
The dataset for this study will not be shared on an open access forum in compliance with ethical regulations associated with the South West Regional Health Authority. Data can be accessed via contacting the corresponding author.
Not applicable.
© The Author(s) 2025.
Open Exploration maintains a neutral stance on jurisdictional claims in published institutional affiliations and maps. All opinions expressed in this article are the personal views of the author(s) and do not represent the stance of the editorial team or the publisher.
Copyright: © The Author(s) 2025. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
