Affiliation:
Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Tanta University, Tanta 31511, Egypt
Email: marwa.abdallah@dent.tanta.edu.eg
ORCID: https://orcid.org/0009-0003-3760-3622
Affiliation:
Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Tanta University, Tanta 31511, Egypt
ORCID: https://orcid.org/0009-0003-3753-1905
Explor BioMat-X. 2025;2:101350 DOI: https://doi.org/10.37349/ebmx.2025.101350
Received: May 24, 2025 Accepted: October 23, 2025 Published: October 30, 2025
Academic Editor: Rosaire Mongrain, McGill University, Canada
Aim: To evaluate the precision of computer-assisted surgery simulation in mandibular condyle reconstruction using a costochondral graft.
Methods: Ten patients (mean age: 14.5 years) with temporomandibular joint (TMJ) pathology and associated pain were included in the study. All patients underwent TMJ reconstruction using costochondral grafts planned through computer-assisted surgical simulation. Preoperative assessment included mouth opening, facial asymmetry, and the differences between planned and actual mandibular positioning.
Results: Postoperative mouth opening was significantly improved in all patients, and facial profile modifications were enhanced. The site of the costochondral graft relative to the glenoid fossa was found to be satisfactory in postoperative radiographs, computed tomography images, and quantitative analysis.
Conclusions: The results of this study demonstrate that virtual surgical planning combined with 3D-printed guiding templates enhanced treatment planning, provided precise osteotomy guidance, facilitated accurate repositioning of bony segments, and improved the contouring of mandibular anatomy in the management of TMJ deformities (ClinicalTrials.gov identifier: NCT06811415).
Jaw deformities may result from temporomandibular joint (TMJ) disorders. TMJ pathology is often associated with dentofacial abnormalities, malocclusion, TMJ pain, headaches, and myofascial pain [1]. The loss of mandibular continuity caused by osteomyelitis, ablative tumor therapy, or severe trauma may significantly affect a patient’s psychological and physiological well-being. Plastic surgeons find it extremely difficult to restore occlusal function and reconstruct the facial form due to the complexity of mandibular anatomy [2, 3].
Alloplastic grafts, such as acrylic, synthetic fibers, ulnar head prostheses, compressible silicone rubber, and total joint replacements, as well as autogenous bone grafts, such as fibula, metatarsal, clavicle, iliac, and costochondral grafts, have been described as the primary reconstructive approaches [4, 5].
To achieve satisfactory results in accurate mandibular contouring and restoration of masticatory function, the three-dimensional configuration of the graft is the most important factor influencing the facial contour and the occlusal relationship. Proper occlusal relationship and condylar position are also particularly important [6, 7].
Numerous maxillofacial surgical applications, including dentofacial abnormalities, congenital deformities, defects following tumor ablation, post-traumatic defects, reconstruction of cranial defects, and reconstruction of the TMJ, have utilized computer-assisted surgical simulation technologies. Compared with conventional case preparation techniques, these technologies can reduce the amount of time the surgeon spends preparing for surgery, increase surgical precision, and provide both intermediate and final surgical splints [8, 9].
Mandibular condyle reconstruction presents several challenges, including potential nerve injury, infection, bleeding, and long-term complications. The complexity of the surgery increases with case severity, particularly in patients with ankylosis or a history of previous surgeries. Functional restoration, especially in children, and the long-term stability of reconstruction are also key considerations. Computer-assisted surgery simulation offers significant advantages by enabling the design and simulation of the surgical procedure and providing fast and accurate results, which compensate for limitations of conventional methods [10].
Our study aimed to use this technology to guide the selection of the rib and print a template with the precise length, and to guide the osteotomy for the joint pathology. The contouring and fixation of the rib grafts were also addressed in this study.
Ten patients (8 males and 2 females) with a mean age of 14.5 years, who suffered from TMJ pathology and reported pain in the TMJ area, were enrolled in this study. All patients underwent mandibular condyle reconstruction with contralateral costochondral grafts using computer-assisted surgery simulation (Table 1).
Patient’s data information.
| Patient No. | Gender | Age (years) | Affected side | Diagnosis | Selection of rib | Costochondral length (cm) |
|---|---|---|---|---|---|---|
| 1 | Male | 13 | Left | Ankylosis | 5th | 3.5 |
| 2 | Male | 13 | Right | Infection* | 6th | 3 |
| 3 | Male | 12 | Left | Traumatic bone cyst | 5th | 3.5 |
| 4 | Female | 14 | Left | Osteomyelitis | 5th | 3 |
| 5 | Male | 14 | Right | Ankylosis | 6th | 3 |
| 6 | Female | 15 | Left | Aneurysmal bone cyst | 5th | 4 |
| 7 | Male | 15 | Right | Aneurysmal bone cyst | 5th | 5.5 |
| 8 | Male | 16 | Right | Infection* | 6th | 4.5 |
| 9 | Male | 17 | Left | Aneurysmal bone cyst | 5th | 3 |
| 10 | Male | 20 | Left | Traumatic bone cyst | 6th | 3.5 |
*: Infection refers to condylar resorption resulting from a long-standing infectious process.
The study was approved by the Research Ethics Committee of the Faculty of Dentistry, Tanta University, and was coded R-OS-10-24-3149. All patients and their legal guardians were informed about the purpose of the study, and written informed consent was obtained prior to the initiation of treatment in accordance with the ethical guidelines for human research established by the Research Ethics Committee of the Faculty of Dentistry, Tanta University, which adheres to the 1964 Helsinki Declaration and its later amendments. The approved clinical study number is NCT06811415.
The sample size was determined using the G*Power Version 3.1.9.4 software (Germany). The maximum interincisal opening was the primary outcome of our power investigation. The effect size d = 1.32 was computed [11]. The alpha (α) and beta (β) levels were set at 5% and 20%, respectively, and the study’s power was set at 80%. The estimated sample size was eight patients. To account for a 20% dropout rate, the sample size was expanded to 10 patients.
Patients were chosen in accordance with certain inclusion and exclusion criteria. Ankylosis, functional deformity, cysts, benign neoplasms, resorbed joints, and developmental abnormalities were the primary requirements for inclusion, as well as pain and a mouth opening restriction of less than 20 mm. Active or ongoing infections, patient circumstances where insufficient bone to support the graft, and systemic diseases that increase susceptibility to infection are among the contraindications.
Evaluation incorporated a thorough history and physical examination of occlusion, midline deviation, facial asymmetry and measurement of maximal incisor opening.
Preoperative radiographic analysis incorporated panoramic and chest X-rays. All selected patients had a computed tomography (CT) scan; the preoperative CT should have an interslice thickness of 1 mm, and the CT should not be older than 3 months (Figure 1). Data acquisition and processing: Patients underwent the preoperative cranialmaxillofacial and chest CT scans with 0.625 mm slice increment, 0.3 mm voxel size, 17 × 23 cm extended field of view, 1,120 kV, 5 mA, and “4 ms” exposure time with a stable molar occlusion [12], using ProPlan CMF software [FDA 510 (k) Number: K111641], Materialise Mimics 16.0 (Materialise, Leuven, Belgium) and DePuy Synthes (Johnson & Johnson, Solothurn, Switzerland), for virtual surgical planning.
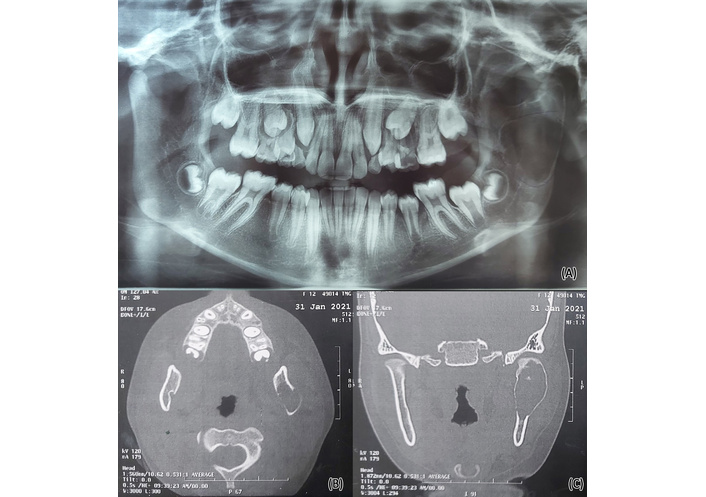
Traumatic bone cyst of the left mandibular ramus and condyle. Panoramic X-ray film shows a left traumatic bone cyst related to the left ramus and condyle (A). Axial and coronal cuts CT shows a left traumatic bone cyst (B, C). Source from case No.3.
All procedures, including general anesthesia and nasoendotracheal intubation, were performed under strict conditions. Preauricular and Risdon incisions were combined. To ensure optimal visualization and facilitate management of any external carotid branch hemorrhage that may arise during the procedure, it was essential to finish the dissections of the superior and inferior incisions prior to performing osteotomies.
The dissection was carried out as far posteriorly as feasible to prevent injury to the branches of the facial nerve, all the way down to the posterior root of the zygomatic arch. Adequate dissection of the soft tissue medial to the neck of the condyle was essential to avoid hemorrhage from the internal maxillary artery and its branches, which are most commonly involved with hemorrhage during TMJ surgery. Ramal exposure was achieved through the posterior mandibular, which provided excellent visualization of the entire ramus for placement of the costochondral graft. Prior to releasing the bone mass in case of TMJ ankylosis, the condyle was excised in accordance with the osteotomy guidance (Figure 2).

Computer-assisted surgery simulation technology used to make a surgical template of costochondral graft. Source from case No.3.
To provide an appropriate bone interface between the rib and ramus, the lateral surface of the ramus was clipped. This was predicated on the preoperative planning and measurements.
The mandible was virtually repositioned based on CT measurements; the height from the glenoid fossa to the mandibular angle was measured, as this corresponded to the required rib length. All the contralateral 5th, 6th, and 7th ribs were exported in STL format to choose the most suitable rib for reconstruction. By making an inframammary incision, typically made in the inframammary crease, which is the natural fold under the breast, beginning about 4 cm from the midline, the incision’s length was 3 to 4 cm. A costochondral graft was removed from the right chest at the 5th, 6th, and 7th rib bones. The rib length ranged from 3 to 5.5 cm, and included no more than 5 mm of cartilage corresponding to the prefabricated template as determined by the cranio-maxillofacial 3D reconstruction.
To ensure proper placement of the cartilage into the middle of the temporomandibular fossa, the cartilage was cut and shaped. A titanium plate with four holes was used to secure the graft to the lateral surface of the ramus with bicortical screws measuring 10 mm in length and 2 mm in diameter. To prevent reankylosis, temporal fascia was interposed in the joint space and secured with 3-0 Vicryl suture. Wound closure was performed in a layer-by-layer manner, where the muscle layer was closed and the skin was sutured with interrupted 3-0 Vicryl sutures. A pressure dressing was applied and changed every 12 hours for 4–5 days postoperatively.
After the seventh surgical day, mouth-opening physiotherapy was started through exercises, manual therapy, and massage. It continued until the patients learned the exercises and performed them independently for six months to restore normal muscle function and avoid hypomobility.
Visual analog scale (VAS), protrusive movements, lateral excursion, and interincisal mouth opening at the first week, one month, and six months of follow-up. Complications at the graft harvest site were also evaluated.
To assess the functional adaptability and appropriate positioning of the graft at the surgical site, postoperative CT scans were obtained.
Statistical analyses were performed using Statistical Package for the Social Sciences (SPSS version 26); the chi-squared test was used to compare categorical variables and repeated measures. ANOVA was used to compare numerical variables (the level of significance was set as p < 0.05).
A physical examination was performed on all patients as part of the routine assessment of overall health status, and all patients were found to be fit for surgery with no complications regarding general examination and assessment. Ten patients (eight male and two female), with a mean age of 14.5 years (range: 12–20 years), including two cases of unilateral ankylosis (20%), six cases of TMJ pathology (60%), including three cases of aneurysmal cyst (30%), two cases of traumatic bone cyst (20%), and one case of osteomyelitis (10%), and two cases of condylar resorption due to long-standing infection (20%). All patients underwent costochondral graft reconstruction guided with computer-assisted surgery simulation. The 5th rib was selected in six joint reconstructions, while the 6th rib was used in four reconstructions (Figure 3).
Before surgery, all patients had moderate discomfort, with a mean VAS score of 4.8 (range: 1–7 points). Six patients reported excellent pain relief, while four reported moderate relief. At one month postoperatively, the mean VAS score was 2.2 points (range: 1–4 points). By six months after surgery, all patients were satisfied with the reduction in their degree of pain.
After six months, the mean postoperative maximum interincisal opening was 30 mm (range: 26 to 33 mm) and standard deviation 1.75 mm, while the mean preoperative maximum interincisal opening was 18.1 mm (range: 15–29 mm) and standard deviation 2.5 mm. The difference in maximal interincisal opening between the preoperative measures showed notable improvements (p < 0.001).
A successful postoperative occlusion was achieved in every patient. No patients had complaints regarding weakening of the facial muscles on the repaired side or numbness of the lower lip. Every patient was pleased with the appearance of the wound scar, and every patient’s range of motion in the mandible had significantly improved after surgery.
All patients’ mandibular condyle reconstructions using the costochondral graft were effective, according to postoperative CT scans, and every rib suited the lateral surface of the ramus perfectly. The titanium plate and screws were precisely secured, and the postoperative position of the bone grafts was comparable to the normal position of the mandible in relation to the glenoid fossa (Figure 4).
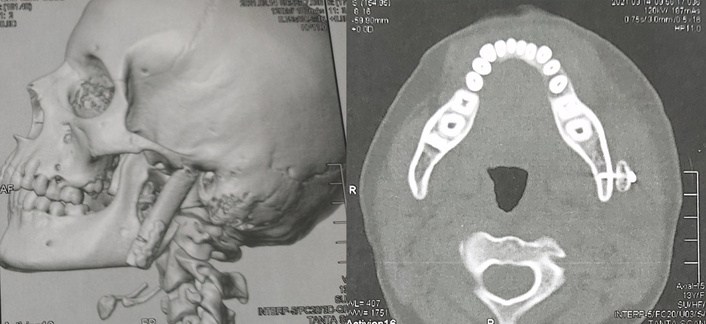
Postoperative 3D and axial computed tomography show costochondral graft with accurate position in relation to the lateral surface of ramus. Source from case No.3.
Computer-assisted surgery simulation technology eliminates the traditional steps in which the surgeon manually positions the costochondral graft into its new final position on the mandible, thus saving time and improving surgical accuracy. We have documented the accuracy of the computer-assisted surgery simulation in this study compared to the traditional planning methods, as the actual surgical outcomes were consistent with the planned outcomes. These findings are in agreement with a recently published study demonstrating that the computer-assisted surgery simulation protocol results in improved outcomes [13–16].
The costochondral transplant is the autogenous approach that is most commonly used. Compared to other autogenous transplants, costochondral transplantation offers numerous benefits. Harvesting is simple and causes minimal morbidity for patients. The costal cartilaginous cap is composed of hyaline cartilage, which allows the transplant to withstand functional loading effectively and exhibit outstanding biocompatibility. Children who receive a costochondral graft may grow. Notwithstanding these benefits, several potential complications exist, including donor-site morbidity, poor rib bone quality, the potential for cartilage and rib bone to separate, graft fracture, recurrence of ankylosis, and inconsistent development behavior. Despite being rare, donor site morbidity, including emphysema, atelectasis, pleural effusion, pneumothorax, and pleural rupture, can nonetheless cause discomfort for patients. The graft was harvested from the right side to differentiate postoperative pain from cardiac pain and the cartilaginous part, which has an important role as a growth center [17, 18].
Costochondral grafts have been reported in several publications for condylar reconstruction in patients with merely a preauricular incision [19] or an intraoral incision along with a preauricular incision [20], which offer the advantage of minimizing the risk of injury to the facial nerve’s marginal mandibular branch. To provide wide exposure and good access without causing affection to the marginal mandibular nerve, our procedure only required a preauricular incision in conjunction with a Risdon incision.
Based on the clinical findings, 100% of the joints were reconstructed using the fifth or sixth ribs. According to earlier research, several surgeons removed the fifth and seventh ribs for joint reconstruction [19]. Another study reported that the sixth rib has the optimal depth and width, this study precisely answered that the fifth and sixth ribs may be harvested for the majority of joint reconstructions [20].
In terms of surgical guide accuracy, the findings demonstrated that all guides were stable with sufficient retention on the bone surfaces, guided all osteotomies safely, and were simple to insert in their designated locations. Other writers, who discovered that computer-aided surgery simulation greatly increased the safety of TMJ ankylosis procedures and decreased the frequency of complications, corroborated these results. These results run counter to those of another study that found certain limitations, including the likelihood that the surgical guides would be difficult to put on [21, 22].
The limitations of this study include the following: First, the statistical strength of the results is limited by the small sample size (10 patients). To confirm the observed trends and support the findings, a larger sample size would be required. Second, the absence of a control group makes it difficult to assess how much of the observed benefits can be attributed to 3D-printed templates and virtual surgical planning alone, rather than to conventional surgical techniques. Third, the six-month follow-up period was relatively short, which might not have sufficiently captured the stability of results over the long term or the possibility of late complications. To validate and build on these findings, more research with randomized controlled designs, larger populations, and longer follow-up periods is crucial.
This study demonstrates that using 3D-printed guides in conjunction with virtual surgical planning improves the precision and effectiveness of TMJ reconstruction procedures, resulting in better functional and clinical outcomes. By facilitating accurate graft placement and anatomical restoration, these technologies contribute to greater mandibular mobility and minimize postoperative discomfort. The level of care in TMJ reconstruction has the potential to be significantly improved by incorporating computerized planning into conventional surgical practice.
CT: computed tomography
TMJ: temporomandibular joint
VAS: visual analog scale
MTI: Conceptualization, Methodology, Investigation, Writing—original draft, Writing—review & editing. MNB: Data curation, Visualization, Supervision. Both authors read and approved the submitted version.
The authors declare that they have no conflicts of interest.
This study was approved by the Research Ethics Committee of the Faculty of Dentistry, Tanta University, code R-OS-10-24-3149 and the clinical trial number was NCT06811415.
Informed consent to participate in the study and to receive treatment was obtained from all patients or their legal guardians prior to starting treatment.
Informed consent to publication was obtained from the legal guardians of relevant participants.
The data of the submitted paper are available upon request to the corresponding author, marwa.abdallah@dent.tanta.edu.eg.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
© The Author(s) 2025.
Open Exploration maintains a neutral stance on jurisdictional claims in published institutional affiliations and maps. All opinions expressed in this article are the personal views of the author(s) and do not represent the stance of the editorial team or the publisher.
Copyright: © The Author(s) 2025. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 1480
Download: 28
Times Cited: 0
