Affiliation:
Department of Psychology, University of Otago, Dunedin 9082, New Zealand
Email: lfranz@psy.otago.ac.nz
ORCID: https://orcid.org/0009-0006-5190-3412
Explor Neuroprot Ther. 2025;5:1004115 DOI: https://doi.org/10.37349/ent.2025.1004115
Received: July 15, 2025 Accepted: August 28, 2025 Published: September 16, 2025
Academic Editor: Manuel Zeitelhofer, Karolinska Institutet, Sweden
Exercise may be one of the most potent tools for protecting the brain—but only through active participation can its benefits be realized. This perspective provides a brief overview of current research avenues and key insights into the role of physical activity and exercise in preventing and mitigating chronic and neurodegenerative diseases and promoting optimal health across the population. The perspective opens with a summary of key findings on how exercise supports brain health and cognitive well-being. It then draws on rodent model studies which shed light on the molecular mechanisms behind these benefits. The paper addresses challenges in translating this research into effective, real-world exercise programs and introduces a new framework aimed at fostering global, inclusive initiatives. This transformative approach is designed to reach individuals across all ages, backgrounds, and health statuses. A central theme throughout is the critical role of psychological factors in exercise adherence—highlighting the need to tackle these barriers if scientific advances are to translate into meaningful benefits for diverse populations.
“Disorders of the central nervous system (CNS), in particular those leading to cognitive deficits, are the main challenge facing medicine in the 21st century. Pathophysiologically based cures of CNS disorders do not yet exist; at best, contemporary medicine is limited to symptomatic treatments.” (the first page of [1]).
With rising rates of chronic diseases—including neurodegenerative conditions such as Parkinson’s, Alzheimer’s, and multiple sclerosis—exercise interventions are increasingly being explored as viable strategies to help mitigate symptom severity and slow the progression of these illnesses. While the term neuroprotection is often used in the context of treatments or interventions aimed at managing neurological disorders and slowing disease progression in neurodegenerative disease [2], it more broadly refers to any processes that protect nerve cells from injury or death. In this context, exercise may prove to be one of the most effective and accessible forms of neuroprotection available.
A wide range of organized sports and physical activities—including table tennis, boxing, fitness classes, dance, golf, cycling, walking, running, and martial arts—has been highlighted in research exploring the role of exercise in supporting individuals affected by neurodegenerative diseases. Initiatives promoting these activities are on the rise, aiming to increase participation among those directly impacted. However, psychological factors must also be carefully considered to maximize the success and reach of such programs. This paper highlights (i) key avenues of research that are deepening our understanding of the neurobiological links between exercise and brain health, and (ii) psychological research addressing the often-overlooked but essential factors influencing long-term exercise adherence. It is imperative that these strands be integrated so the neuroprotective benefits of exercise can effectively reach the people who need them most.
Physical activity involves movement of skeletal muscles, which increases energy expenditure; exercise is a specific form of structured physical activity, usually goal-related and can be further classified into aerobic or other types [3]. In the present context, a distinction between the different forms of physical activity/exercise is not the focus, and the terms are used interchangeably. These activities provide available avenues for optimizing brain health as well as body health in the general population and also offer the potential to mitigate symptom severity and slow rates of cognitive, neurological, mental, and physical decline associated with neurodegenerative diseases [1, 4–6]. While reducing all-cause mortality is a huge benefit of engagement in physical activity in the population at large, so too are neuroprotective effects (particularly studied with onset of the COVID era), such as the role of exercise in directing the immune system to an anti-inflammatory state [7, 8]; yet even that is just the tip of the iceberg of the benefits of exercise.
Physical activity and exercise enhance cognitive function [3] and possibly even provide neuroprotection against declines in cognition, particularly during aging when neurodegenerative diseases such as Alzheimer’s and Parkinson’s tend to occur [4–6, 9–11]. Benefits of exercise on cognition, postural balance, and overall quality of life have also been shown in people with multiple sclerosis [12].
Reducing the risk of coronary heart disease, type 2 diabetes, and forms of cancer are some of the other lauded benefits of exercise more generally [13], but that is also far from a complete list. Considering coronary artery disease alone, which is the leading cause of death worldwide (and is also linked with insulin resistance and type 2 diabetes), research indicates a reduced risk with regular physical activity/exercise [14, 15]. Understanding the precise mechanisms and processes involved, and the levels of exercise that provide optimal benefits, are two exciting areas of research much in need of further investigation. Levels of lipoproteins, mitochondrial biogenesis, changes in the heart and arterial vascular networks, and related changes in inflammation are among the implicated factors underlying the beneficial effects of exercise [15]. However, more research is necessary to understand the precise molecular mechanisms involved.
Research on humans into cognitive benefits of physical activity and exercise has increased in recent years across the fields of psychology, neuroscience/neurobiology, sports science and medicine [3, 10, 16]. A range of methods has been employed, using either ‘exercise interventions’ between pre- and post-test comparisons of cognitive measures, or cross-sectional approaches involving exercise-involved versus control groups. Activities such as table tennis, boxing, cycling, walking, swimming, dancing, and martial arts among others have been employed in those investigations; although that is not a complete list [12, 17–21]. Positive effects have been reported on global cognition, executive function, memory processes, and focused attention, particularly in relation to long-term bouts of exercise (i.e., long interventions); for example, when performed 3–4 times per week for 3–6 months [10]. But even a short bout of exercise considered as ‘acute’ can lead to cognitive performance benefits according to a recent meta-analysis of research spanning from 1995 to 2023 [3].
Although the largest benefits seem to be conferred in studies on older individuals (> age 60 years), the age group focused on more than any other [10], benefits to cognition are also demonstrated in younger adults [3]. Physical exercise combined with cognitive training may yield greater benefits for brain health than physical exercise alone [22]. By this reasoning, activities like table tennis—which involve complex cognitive demands such as rapid reactions, strategic planning, inhibition, visual tracking, prediction, memory, and task switching—could hold particular promise as effective exercises for supporting brain health and cognition. However, this potential remains to be rigorously tested.
Recent advances in research highlight links between neurodegenerative diseases and declines in cognition [23] but much is still to be learned about associated brain processes and lifestyle factors that might ward off, or slow, neurodegeneration. The literature points to exercise as an encouraging non-pharmacological method for maintenance and cognitive improvement, and also preventing declines of cognitive function [10, 24]. However, factors such as exercise frequency, intensity, and duration, specific type of exercise, and participant demographics vary considerably across studies, making it difficult to determine what the optimal exercise prescriptions should be [10]. It is also relevant that while novel drugs can treat inflammation and other aspects of chronic neurological diseases, fatigue and physical limitations often lead to a decrease in quality of life which can be mitigated by exercise. This, for example, has been shown in people with multiple sclerosis whose participation in forms of martial arts and other strength training improved quality of life [12].
Evidence-based physical activity guidelines by the World Health Organization (WHO) recommend a minimum of 150–300 minutes of moderate physical aerobic activity for adults per week, and 1 hour per day on average for younger people [25]. The recommended requirements can also be reached through a combination of vigorous cardiovascular activity and moderate activity. Examples of moderate physical activity are everyday tasks such as washing dishes, gardening, ironing, and preparing food.
To put it into perspective, engaging in just 30 minutes of moderate physical activity per day amounts to about 3% of a person’s waking hours over the course of a week (assuming 8 hours of sleep per night); that small amount of time spent on physical activity would already exceed the minimal recommended guidelines. Thus, it is astonishing that at least 27% adults and 80% adolescents world-wide reportedly do not meet minimal physical activity recommendations (as of those 2020 reports).
Given the above, it is essential that education about the benefits of regular exercise—especially its neuroprotective effects as a vital part of maintaining healthy wellbeing—be communicated broadly and effectively. Each of us can help by raising awareness, staying physically active, and encouraging others to do the same. Without widespread understanding and action, these benefits risk being overlooked.
While social media can be a powerful tool for spreading messages, more structured education about the importance of daily physical activity could have universal benefits. Alongside other educational campaigns, a promising approach might build on school programs, where children educate their parents through meaningful homework assignments and activities, creating a ripple effect of awareness from younger to older generations. Ultimately, knowledge about the necessity of regular exercise should be as accessible and emphasized as education on healthy eating and sleep.
A landmark perspective by Hillman and colleagues [26] (2008) identified exercise as a key lifestyle factor that enhances both physical and mental well-being throughout the lifespan. Since then, a substantial and growing body of research has reinforced this view, with emerging evidence pointing to exercise as a powerful form of neuroprotection. The following section provides a snapshot of current findings and highlights promising directions for future investigation.
To support this discussion, Figure 1 presents a proposed framework for optimizing brain health. The approach emphasizes the interplay among four key components: research activities, the development of effective exercise programs, the engagement of participants, and the involvement of trained specialists who guide and interact with those participants. The framework also underscores the critical role of sustained adherence—not only in maintaining these programs but also in achieving long-term health outcomes.
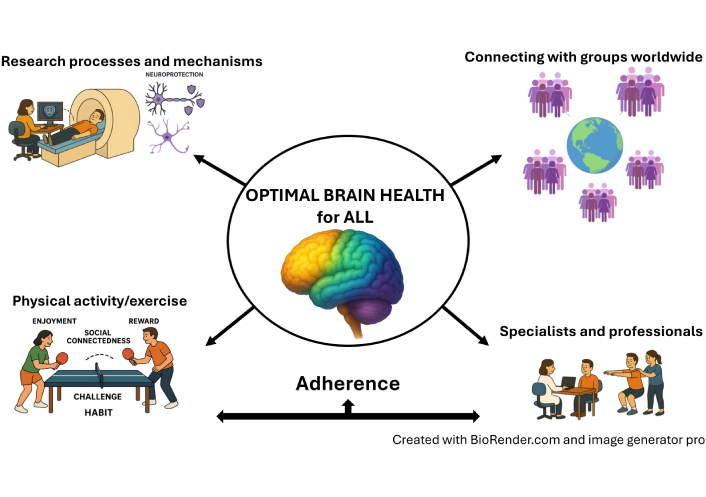
Proposed model for optimal brain health through neuroprotection from physical activity and exercise. The top left highlights the need for strong research at both macro and micro levels: a magnetic resonance imaging (MRI) scanner represents human studies examining whole-brain effects, while the astrocyte symbolizes cellular and mechanistic research (see text for details). The lower left emphasizes the development of inclusive, engaging programs (which also serve as research interventions) that promote participation and foster positive psychological factors like social connection and enjoyment, with table tennis as one example. The top right underscores the importance of reaching broad populations globally to encourage widespread involvement. The lower right illustrates the critical role of professionals—such as medical specialists, coaches, and nurses—in supporting participants, especially those with neurological or neurodegenerative conditions. At the base is adherence, which is critically important to foster in all components of the coordinated efforts. As of 2024, New Zealand’s organized table tennis groups for people with Parkinson’s disease are incorporating this approach. The author has an active license for Biorender through the University of Otago (under Liz Franz: L. Franz). Created in BioRender. Franz, L. (2025) https://BioRender.com/5kfeo7b.
Pre-post comparisons using exercise interventions are commonly employed in human studies to identify changes in brain structure and function, and in cognitive function.
Brain imaging techniques, such as magnetic resonance imaging (MRI) and its functional counterpart, functional MRI (fMRI), are commonly used to measure changes in brain activity through the use of cognitive tasks that rely on executive function, memory, information processing, attention, and a range of other cognitive abilities [10, 16]. These studies typically rely on purpose-designed tasks performed by participants either while in the scanner or in separate assessments outside the scanner (see Figure 1 for illustration).
A key limitation of this research approach is that physically demanding activities—such as table tennis—cannot be performed inside an MRI scanner, where the individual must remain completely still. Movement not only violates scanner constraints but also introduces artifacts that compromise data quality. As a result, measuring brain activity during the execution of complex motor skills is not always straightforward. Nevertheless, alternative methods can offer valuable insights into brain changes associated with such activities. For example, within-subject pre-post comparisons have shown increased functional connectivity between brain regions and greater integrity of the white matter tracts linking them—both of which are thought to reflect benefits of physical activity, particularly aerobic exercise [27].
Predicted areas of brain activity associated with exercise are shown in Figure 2 for illustrative purposes only. Such predictions can lead to the formulation of specific research hypotheses. For instance, one might hypothesize that patterns of brain activation elicited by exercise overlap with brain networks involved in specific cognitive functions. Of particular interest are the striatal-thalamic-frontal circuits associated with cognitive task switching—a key component of executive function—since these networks are known to be affected in Parkinson’s disease [28–30]. Although precise molecular mechanisms are still being elucidated, it stands to reason that if the effects of exercise tap into the same brain areas as those used in cognition, exercise might promote neuroprotection for cognition. Hypotheses stemming from such inferences fuel the scientific landscape with questions for investigations that research scientists are working hard to answer.
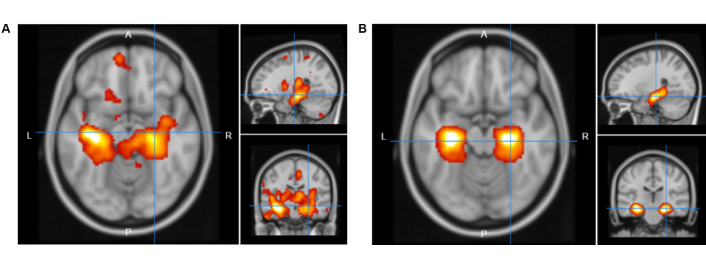
Predicted brain activation from NeuroQuery using the keywords (A) “exercise”, and (B) “hippocampus”; each shown on brain maps in the axial (left large panel), sagittal (top right), and coronal (lower right) planes. NeuroQuery (https://neuroquery.org, accessed 2025 Jul 10) generates predictions through statistical meta-analysis, using a training corpus of approximately 14,000 neuroimaging publications to model associations between keywords and brain activation patterns [31].
At the microscale, most research has relied on rodent models, largely due to the ethical and safety challenges of conducting such studies in humans. For instance, studies in rats have demonstrated that exercise can enhance memory—a core cognitive function—by promoting neurogenesis (the formation of new neurons) in the dentate gyrus of the hippocampus, a key structure within the brain’s memory system [11]. While the hippocampus is illustrated in the human brain in Figure 2B, the majority of supporting evidence currently comes from rodent studies.
In addition to its cognitive and structural benefits, physical activity/exercise promotes angiogenesis, enhancing the brain’s vascular system and improving blood flow [32]. This improved circulation supports overall brain health and facilitates the delivery of essential molecules, including neurotrophic factors. Among these, brain-derived neurotrophic factor (BDNF)—the most extensively studied neurotrophin in the mammalian CNS—has been shown to increase with exercise. BDNF plays a crucial role in enhancing brain function by supporting neuroplasticity, the brain’s ability to adapt and reorganize in response to experience [33].
Building on previous findings, recent research has begun to explore the neuroprotective roles of non-neuronal cell types, particularly astrocytes, which are a major subtype of glial cells. Astrocytes serve as essential support cells in the brain and spinal cord, maintaining the internal environment necessary for healthy neural function. Despite their diversity, astrocytes share key functions such as regulating chemical balance, facilitating communication between neurons, and preserving brain tissue integrity [1].
Much of this research opens a promising frontier of investigation [1, 34]. Astrocytes play crucial roles in transporting nutrients, neurotransmitters, and ions. Notably, they release antioxidants during stress and influence mitochondrial function (the cell’s ability to produce energy) following injury—actions that align with a neuroprotective phenotype [35]. Their involvement extends to regulating cerebral blood flow, neural transmission, metabolism, and the brain’s energy homeostasis, all of which are highly relevant to the effects of exercise [1, 34, 35].
Recent studies suggest that astrocytes may be a key mechanism underlying exercise-related improvements in cognition. However, despite evidence of shared mechanisms conserved across species, further research is needed to translate these findings to human models [36].
Consistent with the research described above, growing evidence shows that physical activity and exercise promote the release of neurotransmitters, neurotrophins, and neuromodulators that enhance neurocognitive function [37]. A recent study using a rodent model of induced cerebral hypoperfusion—a condition linked to cognitive impairments in neurodegenerative diseases such as Alzheimer’s and Parkinson’s (with astrocytes implicated)—demonstrated that two months of exercise (post-hypoperfusion) via running wheel access led to improvements in both spatial and non-spatial memory [35].
An emerging and rapidly developing area of research is the impact of exercise on mental health, in addition to its recognized cognitive benefits. Using measures commonly applied in human studies, recent findings show that even moderate physical activity can reduce symptoms of depression—possibly through mechanisms such as lowering inflammation [38]. Exercise has also been shown to support emotional regulation [27], including reducing the intrusion of negative memories, as demonstrated in a recent study involving table tennis-based interventions [39]. However, our understanding of the precise neurobiological mechanisms underlying these mental health benefits remains limited. This growing field holds considerable promise for future discoveries.
While the translation of research findings to humans is still in its infancy—particularly regarding our understanding of precise mechanisms—the implications for human practice suggest a clear need for long-term lifestyle adoption of exercise by as many people as possible to achieve optimal outcomes. However, one of the biggest challenges is overcoming the so-called “adherence to exercise phenomenon” [40], which refers to the common problem of people discontinuing activity shortly after starting. Only through sustained adherence can exercise activities, programs, and even individual forms of exercise deliver meaningful benefits to the population. Figure 1 displays adherence as a crucial factor for the success of any coordinated efforts toward optimising brain health.
Although something motivates people to begin training—whether it’s the appeal of a game, casual play, or interval training—that motivation likely varies widely among individuals. As with any sport or exercise activity, individual differences abound in relation to the complex mix of components involved, including participants’ fitness, agility, age, and health status. Some people are highly competitive, which alone drives them to participate. Others are less competitive but seek social interaction with like-minded individuals. Still others may be more timid, yet eager to push their own boundaries. Of course, some reach the highest ranks, benefiting from a combination of competitiveness, fitness, and the time and energy to train and compete.
Psychological factors such as connectedness, relatedness, social support, and the exchange of helpful information by specialists (e.g., researchers and medical professionals who can be part of organized programs where possible) are all key to better adherence [40]. Nurturing enjoyment whenever possible, encouraging social support (such as bringing a partner or friend), and tailoring specific skills to targeted groups (e.g., aging populations, individuals with neurodegenerative diseases, and/or those with physical or mental impairments) all contribute to making exercise a rewarding experience. This positive reinforcement, fostered through a socially supportive environment, enhances adherence. One thing is certain: to reap the benefits for brain health, physical health, and cognitive-mental wellbeing, it is imperative that people participate in regular physical activity or exercise—and continue to do so. Only then will exercise become an accessible and effective means of optimizing health and well-being across the population at large.
This piece highlights the potential of organized exercise programs to engage individuals in healthy activities that can become lifelong habits. Equally important is ensuring access to inclusive, adaptable options—such as community gyms, parks, trails, or home-based alternatives—that support independent physical activity. While some prefer to exercise alone, it is important to note that group activities offer social connections that can further motivate and sustain long-term participation.
Although high-income countries generally have developed infrastructure like bike paths and urban parks, recent data reveal these regions still face high levels of sedentary behavior, particularly among females [41]. This underscores that despite resources, promoting widespread participation remains a challenge globally.
International organizations have established a strong foundation for global physical activity policy, beginning with UNESCO’s 1976 International Conference and the 1978 International Charter of Physical Education and Sport, which officially recognized physical education and sport as fundamental human rights (affirmed in Chapter 1), and emphasized lifelong learning (Chapter 3), health (Chapter 5), and inclusion of children and persons with disabilities (Chapter 6) [42]. While early policies focused broadly on health and inclusion, more recent UNESCO initiatives—including the Quality Physical Education (QPE) Guidelines of 2015 and the Kazan Action Plan in 2017—have aligned physical activity policies with the UN Sustainable Development Goals [43]. Complementing this, WHO’s Global Action Plan on Physical Activity (GAPPA) in 2018 provides guidance and tools to help countries increase activity levels [44]. More recently, UNESCO’s QPE policy briefs and toolkits in 2021, followed by the 2024 Global State of Play report [45], have highlighted the cognitive and brain health benefits of physical activity.
Despite these extensive policy efforts, the 2024 report [45] notes that physical education remains under-prioritized. Recognizing the significant efforts invested globally, it remains essential to ensure that these initiatives translate effectively into practice so people of all ages and backgrounds can benefit.
Just as translating research into effective physical activity programs is vital for community health, ensuring that policies are fully implemented through practical, accessible means remains an ongoing priority. Although detailed implementation lies beyond this perspective’s scope, continued collaboration and innovation will be key to bridging policy and practice for maximum public health impact.
Even as global strategies continue to evolve, lasting change ultimately depends on what happens in our neighborhoods, communities, and daily lives. Bridging the gap between policy and practice requires not only institutional commitment but also grassroots action and individual initiative.
Encouraging people to become more active can be supported through welcoming messages and slogans such as “Join us!”, “Come along!”, or “Welcome all!”. This creates an inclusive atmosphere that invites participation and strengthens the sense of belonging that comes from shared activity. Encouraging team leaders, coaches, and group members to refer to each other by name during interactions can help personalize the experience, strengthen social bonds, and foster a more supportive and inclusive environment. Social connection goes a long way—and each of us can foster it, whether in the activities we join or those we help lead.
Keeping a digital or handwritten activity log can also boost motivation by helping individuals track progress and experience a sense of accomplishment. Digital devices offer one way to support this, though their effectiveness across settings remains mixed [46]. Still, the broader message is clear: some physical activity is far better than none (and most likely, the more, the better).
Activity logs can also help individuals monitor perceived changes in physical, cognitive, or mental health—such as mood improvements or regressions. These records may guide decisions about when to consult health professionals and help streamline clinical conversations, especially in regions facing shortages of medical providers. In addition, digital tools may reinforce goal-setting and deliberate practice, both of which support habit formation. Encouraging these strategies early in life may be one of the most effective ways to establish habits that foster sustained lifelong engagement in physical activity [47].
Collaboration among diverse groups—including scientific researchers, medical specialists, program facilitators, and participants—is essential for translating research findings into effective, accessible programs for the public (see Figure 1). Sustaining long-term participation in organized physical activity also benefits from teamwork among professionals. For example, a coach with expertise in neurodegenerative disease, a physiotherapist experienced in movement disorders, or a nurse familiar with neurological care can significantly enhance exercise programs tailored to individuals with specific clinical needs.
While not all programs involve such specialists, the design of inclusive, supportive environments remains key. Table tennis organizations have been leaders in promoting brain health through movement. They have launched global initiatives targeting people with Parkinson’s, Alzheimer’s, and multiple sclerosis—building on a robust foundation of programs designed for individuals of all ages, ranging from very young children to para-athletes with diverse abilities. These efforts extend to specialized forums that connect participants directly with researchers and practitioners who shape the programs. For instance, the World Table Tennis for Health Congress features sessions on neuroscience, physical activity, and community support, highlighting the sport’s growing role as a platform for well-being and evidence-based intervention (hyperlink: ITTF Foundation, 2024) [48].
Promoting physical activity and exercise as a priority for all requires coordinated efforts across education, infrastructure, communication, and resource allocation. This includes expanding access to safe, welcoming spaces for movement; investing in public education campaigns; and sharing accurate, up-to-date research in ways that are both understandable and actionable. While global frameworks have laid important foundations, continued effort is needed to ensure that strategies are effectively implemented and reach the populations that need them most.
Education is especially critical. Lifelong physical activity habits can be encouraged as early as possible, beginning in the home and also in school-based programs that not only engage children but further influence their families—creating a ripple effect that extends to parents and even grandparents when delivered with deliberate intent. Bottom-up approaches like these, combined with top-down support from public institutions, can help integrate physical activity more seamlessly into everyday life.
Awareness campaigns—including media advertisements and local programs—can continue to expand, as they show promise for shifting cultural norms around movement. Universities can (and often do) play a leading role by translating research into public engagement through community presentations, participatory research, and partnerships with local organizations. Ultimately, the need for physical activity and exercise affects us all—and promoting it must become a shared societal responsibility.
Exercise is neuroprotection—but participation is the imperative. People must engage in regular movement, whether through structured exercise or daily physical activity, and continue to do so. This is not to suggest that these behaviors should replace medical treatments or medications, which remain essential for many. Rather, physical activity and exercise represent fundamental needs and vital contributors to brain health. Integrating these into daily life is crucial for overall well-being.
In summary, there is a clear need for:
More research into the mechanisms underlying the neuroprotective effects of exercise;
More research into identifying optimal “doses” of physical activity tailored to different age groups, fitness levels, and types of neurodegenerative disease;
Acknowledging and fostering psychological factors that promote sustained adherence to physical activity and exercise routines and programs, which is critical for maximizing the benefits across the population;
Collaborative approaches to program development, involving researchers, clinicians, and participants, to ensure that exercise strategies are effective, inclusive, and widely adopted;
Providing accessible resources that reach people across countries, cultures, and socioeconomic levels.
BDNF: brain-derived neurotrophic factor
CNS: central nervous system
fMRI: functional magnetic resonance imaging
GAPPA: Global Action Plan on Physical Activity
MRI: magnetic resonance imaging
QPE: Quality Physical Education
WHO: World Health Organization
The author acknowledges individuals around the world living with neurodegenerative and other diseases who actively strive to improve their lives through daily exercise and healthy lifestyle choices. The author is also deeply grateful for the insights and contributions of colleagues and research participants over the years.
EAF: Conceptualization, Writing—original draft, Writing—review & editing.
The author has no conflicts of interest to report.
Not applicable.
Not applicable.
Not applicable.
Not applicable.
There were no specific grant sources for this Perspective.
© The Author(s) 2025.
Open Exploration maintains a neutral stance on jurisdictional claims in published institutional affiliations and maps. All opinions expressed in this article are the personal views of the author(s) and do not represent the stance of the editorial team or the publisher.
Copyright: © The Author(s) 2025. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 2703
Download: 30
Times Cited: 0
