Affiliation:
1Rheumatology Department, Ramón y Cajal University Hospital, 28034 Madrid, Spain
2Rheumatology Department, HLA Moncloa University Hospital, 28008 Madrid, Spain
3Rheumatology Department, HM Sanchinarro University Hospital, 28050 Madrid, Spain
Email: carlosantonio.guillen@salud.madrid.org
ORCID: https://orcid.org/0000-0002-6480-2294
Affiliation:
1Rheumatology Department, Ramón y Cajal University Hospital, 28034 Madrid, Spain
ORCID: https://orcid.org/0000-0002-9438-6375
Affiliation:
1Rheumatology Department, Ramón y Cajal University Hospital, 28034 Madrid, Spain
ORCID: https://orcid.org/0009-0004-6658-5731
Affiliation:
4Emergency Medicine, Ramón y Cajal University Hospital, 28034 Madrid, Spain
ORCID: https://orcid.org/0009-0001-1115-9602
Affiliation:
2Rheumatology Department, HLA Moncloa University Hospital, 28008 Madrid, Spain
ORCID: https://orcid.org/0009-0002-8718-8618
Affiliation:
3Rheumatology Department, HM Sanchinarro University Hospital, 28050 Madrid, Spain
ORCID: https://orcid.org/0000-0002-3169-0206
Affiliation:
1Rheumatology Department, Ramón y Cajal University Hospital, 28034 Madrid, Spain
ORCID: https://orcid.org/0000-0002-4548-6089
Explor Musculoskeletal Dis. 2023;1:207–215 DOI: https://doi.org/10.37349/emd.2023.00023
Received: August 25, 2023 Accepted: October 16, 2023 Published: November 20, 2023
Academic Editor: Rubén Queiro, Hospital Universitario Central de Asturias & Oviedo University School of Medicine, Spain
Aim: To determine the existence of a correlation between the elastographic study of the patellar and Achilles tendons and the enthesis evaluation in patients with psoriasis with or without psoriatic arthritis.
Methods: Observational, cross-sectional study. Patients with psoriasis, psoriatic arthritis and healthy controls were included. The elastography results of the patellar and Achilles tendons of the non-dominant leg of the three groups were compared and tested for correlation with the Madrid Sonographic Enthesis Index (MASEI) score, as well as an entheses clinical evaluation score [Spondyloarthritis Research Consortium of Canada (SPARCC)].
Results: Forty-eight patients were included, 24 with psoriasis and 24 with psoriatic arthritis, as well as 48 healthy controls. Patients with psoriatic arthritis had a higher clinical enthesitis score than patients with psoriasis (8.0 vs. 1.0, P < 0.001). The mean (standard deviation) or median (25–75 percentile) of control subjects patellar and Achilles’ tendon stiffness, 127.8 kPa (18.5 kPa) and 198.0 kPa (183.2–212.0 kPa) were significantly higher than observed in patients with psoriatic arthritis, 119.2 kPa (19.7 kPa) and 184.8 kPa (175.5–193.9 kPa; P < 0.001 and P = 0.018, respectively). A strong inverse correlation between MASEI score and the patellar and Achilles’ tendon stiffness was also detected (Spearman’s Rho coefficient of –0.813 and –0.941, respectively).
Conclusions: Patients with psoriatic arthritis present less stiffness in those load-bearing tendons than healthy controls. There is an inverse correlation between the enthesis involvement demonstrated by ultrasound and the elastography of these tendons. Tendon elastography can be considered a useful quantitative tool in assessing patients with psoriatic disease.
Enthesopathy is the cornerstone of the pathophysiology of psoriatic arthritis (PsoA) [1, 2]. Even in patients without enthesic symptoms, enthesitis has been demonstrated by imaging tests both at the enthesis of load and the so-called “mini-enthesis” and pseudo-enthesis of the fingers [2–4]. Moreover, inflammatory enthesopathy has been demonstrated in patients with psoriasis (Pso), and it is presumed that this finding could be, to some extent, a predictor of the development of PsoA [5].
Currently, there are validated forms of study of entheses both at a clinical and imaging level [6–10]. Ultrasound-based imaging counts are the most widespread among rheumatologists and have demonstrated their reliability, especially at the level of large entheses, including or not the hyperaemia component, currently necessary to use the term enthesitis [8, 9, 11, 12]. However, despite their undeniable validity, the ultrasound indices of enthesis assessment are the result of the arithmetic sum of scores whose values have been obtained by regression analysis. Therefore, they are not especially useful for detecting structural changes unless they are evident on the ultrasound image. This limitation prevents these scores from being helpful in detecting short-term changes.
Elastography is an ultrasound technique that allows to determine, numerically, the resistance that a body offers to deformation. Specifically, shear-wave elastography allows for determining a tissue’s stiffness (in kPa) when exposed to low-frequency deforming waves [13–15]. Although it is an operator-dependent technique, like ultrasound, its application to large tendons such as the patellar or Achilles is not difficult and has shown very acceptable intra- and inter-observer agreement [16, 17].
Observations of the use of elastography in tendons have been made, particularly in sports medicine [18–20]. Although the enthesis territories are those where the tendons establish their anchorage in the cortical bone, there is no specific studies on its application in these regions.
To demonstrate that enthesic elastography of loading tendons correlates satisfactorily with traditional enthesopathy scores would lead to considering the possibility of using this technique as a potential follow-up tool with the added advantage of providing numerical values rather than categorical or semiquantitative data. In addition, its use could be considered for monitoring therapeutic responses in shorter periods than those allowed by clinical detection or conventional ultrasound.
The purpose of the present study is to determine the existence of a correlation between the elastography of two loading entheses and the clinical and ultrasound enthesopathy scores of patients with PsoA and Pso.
A cross-sectional observational study was planned. Patients with consecutive Pso and PsoA were selected from three tertiary hospital centres in the Community of Madrid. Adults patients with a dermatological diagnosis of cutaneous Pso with or without nail manifestation and patients with PsoA according to ClASsification criteria for Psoratic ARthritis (CASPAR) criteria [21] of no more than 24 months since diagnosis were included. Exclusion criteria were as follows: patients recently treated (up to three months) with local steroid injection on an enthesis territory included in the Spondyloarthritis Research Consortium of Canada (SPARCC) or Madrid Sonographic Enthesis Index (MASEI) scores, patients with any impediment to the performance of an elastography of the Achilles or patellar tendons or to the performance of a clinical (SPARCC) or ultrasonographic (MASEI) assessment of the Achilles or patellar tendons, and patients treated with Janus kinase inhibitor, biologic, or apremilast therapies. Patients treated with corticosteroids at any dose four weeks before enrolment were also excluded. Recruitment was done over 12 months, from June, 2022.
The control group consisted of healthy volunteers matched for age (± 3 years), body mass index (BMI, ± 1.5 points) and body fat percentage (BF%, ± 2 points) with the patient group.
For the clinical evaluation of the entheses, two trained rheumatologists applied the SPARCC score [10] in all patients. For the ultrasound evaluation, a single rheumatologist with 12 years of experience in rheumatological musculoskeletal ultrasound performed a MASEI [12] study on the group of patients blinded to diagnostic status.
A second rheumatologist, also blind to diagnostic status, performed elastography of the patellar and Achilles tendons of the dominant leg in both patients and controls. Patellar tendon elastography was performed on the proximal section of the tendon, while Achilles’ tendon was assessed in its middle portion. To standardise the pressure exerted by the probe during elastography, care was taken to exert a force that deformed the contour of the skin until it was parallel to the probe without distorting the longitudinal axis of the corresponding tendon.
All ultrasound studies were performed with a General Electric™ S8 ultrasound unit (USA) equipped with an 8–14 MHz linear probe and a 6 MHz elastography probe. For the MASEI study, the power Doppler pulse repetition frequency was adjusted to 850 Hz. Shear-wave elastography was performed using five regions of interest (ROI) of 2 mm diameter located at the same depth of the tendon, coinciding with the middle of its thickness in the longitudinal plane. Patients were instructed not to perform any exercise or physical effort prior to the ultrasound or elastography scans. Both assessments were done at the same visit, with no particular order. Patellar tendon assessment was performed with the knee in a neutral position, after ten minutes of relaxation and with the probe placed directly on the skin with minimal pressure [22]. Achilles’ tendon assessment was performed according to the Group for Research and Assessment of Pso and PsoA (GRAPPA) recommendations [8].
Demographic and epidemiological data were collected from the electronic medical records while anthropometric data were obtained before the ultrasound assessment. Registries of patients and controls were anonymized and coded before included into an electronic data base.
Continuous variables were reported as mean [standard deviation (SD)] if normally distributed or as median (25–75 percentiles) if non-normally distributed, while dichotomous variables were reported as the observed frequency (percentage of subgroup). Mann–Whitney U tests were used to assess differences in continuous variables among subgroups of patients and controls, while the associations between categorical variables were studied using chi-square (χ2) or Fisher’s exact tests. The linear correlation between shear-wave elastography and MASEI results was tested using Spearman’s Rho test. For purposes of statistical analysis, the Statistical Package for the Social Sciences (SPSS) version 21 (IBM Corp., Armonk, NY) was used.
Forty-eight consecutive patients (24 with PsoA and 24 with Pso) and 48 healthy volunteers were recruited. Normal distribution was achieved only by the variables age and patellar elastography in all groups and BF% in the group of patients. Fifty subjects were male (52%). The mean (SD) of age was 38 (8) years old, BMI median (25–75%) was 23.6 (21.0–26.7) and BF% was 21.0 (15.2–26.0). The complete demographic composition of the groups is shown in Table 1.
Demographic features of the subjects recruited, according to their condition
| Feature | Controls (n = 48) | PsoA group (n = 24) | Pso group (n = 24) |
|---|---|---|---|
| Age (years), mean (SD) | 38 (8) | 39 (7) | 36 (8) |
| Male subjects, n (%) | 25 (52) | 13 (54) | 12 (50) |
| BMI, median, (25–75%) | 23.9 (20.6–26.7) | 22.0 (20.3–26.5) | 24.0 (22.4–26.4) |
| BF%, median, (25–75%) | 21.0 (15.0–26.5) | 19.5 (16.0–26.0) | 21.0 (17.0–23.5) |
n: number of people included in the group
The median of the SPARCC and MASEI score in the patient group was 2 (1–8) and 5 (4–11), respectively. As expected, both scores were significantly higher in the group of patients diagnosed with PsoA (Table 2). Patellar stiffness median was 129.0 kPa (18.8 kPa) in the group of patients and 127.8 kPa (18.5 kPa) in the group of controls (P = 0.755). The median of Achille’s tendon stiffness was 196.8 kPa (184.8–210.1 kPa) in the group of patients and 198.0 kPa (183.2–212.0 kPa) in the group of controls (P = 0.815). However, as shown in Table 2, excluding the control group, patients with PsoA showed a significantly lower stiffness than patients with Pso in the patellar tendon, 119.2 (19.7) vs. 138.8 (11.5, P < 0.001) and the Achilles’ tendon, 184.8 (175.7–193.9) vs. 206 (199.3–213.4, P < 0.001).
Results of the clinical and ultrasound enthesis assessment and the elastography study of patellar and Achilles’ tendons
| Assessment | Controls | PsoA group | Pso group | P-value |
|---|---|---|---|---|
| SPARCC score, median (25–75%) | - | 8.0 (3.5–11.5) | 1.0 (0–2.0) | < 0.001 |
| MASEI score, median (25–75%) | - | 11.0 (6.0–15.0) | 5.0 (4.0–11.0) | < 0.001 |
| Patellar tendon stiffness, mean (SD) | 127.8 (18.5) | 119.2 (19.7) | 138.8 (11.5) | < 0.001a |
| Achilles’ tendon stiffness, median (25–75%) | 198.0 (183.2–212.0) | 184.8 (175.5–193.9) | 206.2 (199.3–213.4) | < 0.001a < 0.018b |
a Among both subgroups of patients; b between controls and PsoA group
The SPARCC and MASEI scores showed an acceptable correlation between them, with a correlation coefficient (CC) of 0.788 (P < 0.001). MASEI score showed a strong inverse correlation with the stiffness of the patellar (CC = –0.851, P < 0.001) and Achilles tendon (CC = –0.950, P < 0.001) (Figure 1). Considering patients according to the corresponding diagnosis, MASEI scores showed stronger inverse correlations with tendon stiffness than SPARCC scores (Table 3), except for the patellar tendon in the PsoA group, where SPARCC correlation was slightly higher.
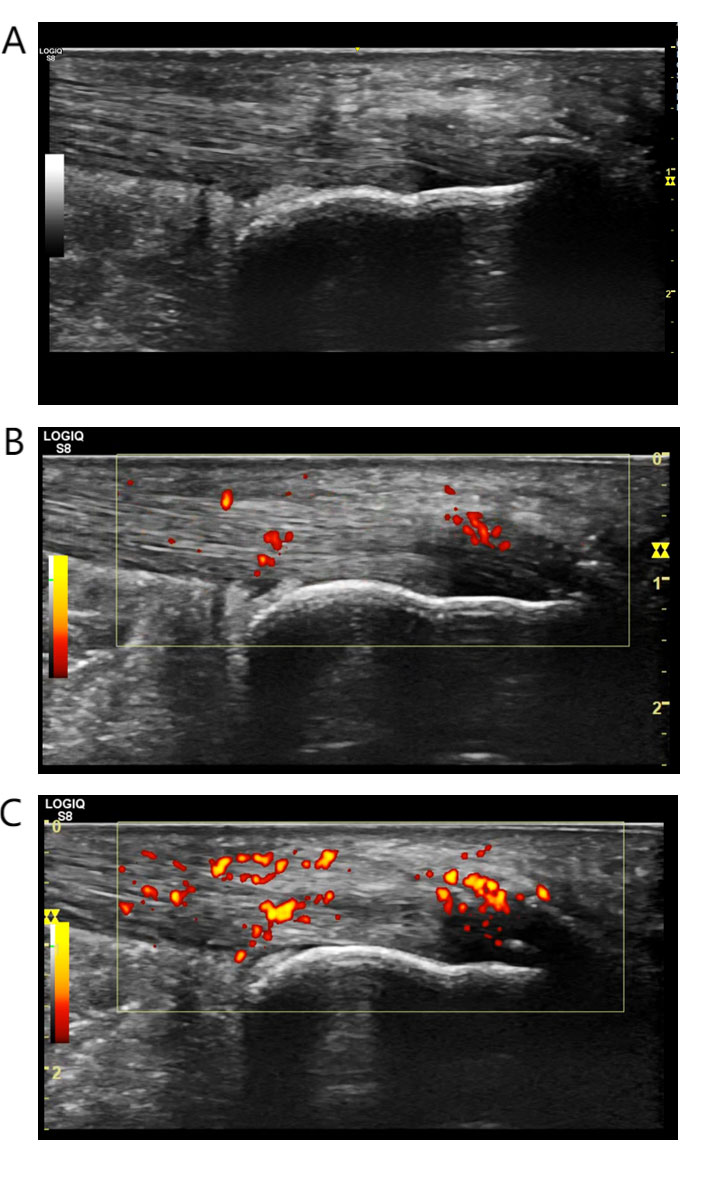
Representative images of the ultrasound studies (MASEI) carried out in the Aquilean territories. A. Patient from the control group of subjects. 46-year-old male, postman. Distal enthesophytosis, tendon thickening without other findings. Elastographic outcome: 188.5 kPa; B. patient with Pso. Male, 38 years old, overweight and sedentary. Tendon thickening, mild-moderate alteration of the distal fibrillar pattern, small enthesophytosis and mild pre-Achilles bursitis. The power Doppler signal placed at more than 2 mm from the cortical surface. Elastographic outcome: 180.3 kPa; C. patient with PsoA. Male, 35 years old, taxi driver. Tendon thickening, alteration of the echostructure of the enthesal territory, enthesophytosis, bursal distension and intense power Doppler signal. Elastographic outcome: 165.7 kPa
Results of the Spearman’s Rho tests of clinical and ultrasonographic scores and the shear-wave elastography assessment of the patellar and Achilles’ tendon
| Region assessed | Patients | PsoA group | Pso group | |||
|---|---|---|---|---|---|---|
| MASEI | SPARCC | MASEI | SPARCC | MASEI | SPARCC | |
| Patellar tendon stiffness | –0.851a | –0.860a | –0.813a | –0.843a | –0.741a | –0.245b |
| Achilles’ tendon stiffness | –0.950a | –0.780a | –0.941a | –0.777a | –0.746a | –0.177b |
a P < 0.001; b no statistically significant
The results of our study demonstrate that load-bearing tendon elastography is a test that correlates satisfactorily with inflammatory activity in psoriatic disease, particularly PsoA, as measured by the MASEI score.
One of the current limitations in assessing the inflammatory activity of PsoA is the lack of quantitative biomarkers, including laboratory data combined with clinical assessments and image studies. In this last field, multiple efforts have been carried out for the elaboration, development and validation of scoring systems for clinical and ultrasound assessment of entheses [5, 6, 23–25]. On one hand, these tools, which have demonstrated great utility, have the limitation that they operate semi-quantitatively. For example, the widely used MASEI score scores six enthesis territories based on a combination of measurements and operator judgments [12]. The SPARCC clinical score, on the other hand, is based on the painful response of patients to pressure exerted by the examiner at eight different points, making it a broadly dichotomous assessment [10]. These limitations do not affect the discriminative capability of these tools to separate patients from healthy subjects or patients with PsoA from patients with Pso, but it is not equally useful in the assessment of the evolution of patients over time, especially in short periods of time.
Shear-wave elastography is a quantitative test that has good inter- and intra-observer agreement [16, 26, 27] and has also demonstrated good sensitivity to change. Its inverse correlation with the indicators of inflammatory enthesis activity is explained by the well-known involvement of PsoA-, which is also demonstrated in Pso- in entheses. Previously, elastography has proven useful in sports medicine in the study of tendon and muscle injuries [18, 19, 28]. In the field of rheumatology, its use in spondyloarthritis is much more austere, although it has proven useful in the detection of therapeutic response at the level of the Achilles tendon in patients treated with biological therapies [29]. A recently published study on validation of Achilles elastography in patients with PsoA showed a satisfactory correlation with joint and skin disease severity. However, the results are not comparable to ours due to significant differences in the measuring instrument [30]. Both forms of elastography most commonly used in clinical practice are operator-dependent assessments, although to a lesser extent than musculoskeletal ultrasound. Homogenisation of the pressure exerted on the skin, as we used in this study, is a standard recommendation used to minimise variability of results.
Our study has two limitations that should be considered when interpreting the results. Firstly, the patients chosen were being treated with non-homogeneous therapies; therefore, we cannot ensure that the results of the elastographic study, or the rest of the response variables, are not heterogeneously influenced by the type of treatment. For example, exposure to corticosteroids or anti-tumor necrosis factor (TNF) therapies could limit the detection of the power Doppler signal on ultrasound, and the use of analgesics could reduce the SPARCC score. In order to reduce this limitation, patients not exposed to corticosteroids and without exposure to advanced therapies were chosen. This choice leads to the second limitation, which is that our group of patients could be considered to be composed of people with mild psoriatic disease, as can be seen from the SPARCC and MASEI score results. However, a large part of the manifestations that score in the MASEI score correspond to structural lesions associated with longer evolution times. Knowing this, patients with PsoA with less than two years of diagnosis were precisely chosen so that the results of the reference indicators can be attributed more to inflammatory activity than to cumulative structural lesions.
Elastography is a technique that is easily accessible for rheumatology units accustomed to performing ultrasound, non-invasive and less operator dependent than musculoskeletal ultrasound. Although it is reasonable to consider future studies with cohorts, elastography can be considered, in light of our results, as a test of interest in the follow-up of patients with psoriatic disease.
BF%: body fat percentage
BMI: body mass index
CC: correlation coefficient
MASEI: Madrid Sonographic Enthesis Index
Pso: psoriasis
PsoA: psoriatic arthritis
SD: standard deviation
SPARCC: Spondyloarthritis Research Consortium of Canada
CAGA: Conceptualization, Investigation, Writing—original draft, Validation, Supervision, Writing—review & editing. MTC, ÁAS, NGM, PZP, JGM and MVD: Conceptualization, Investigation, Writing—original draft, Writing—review & editing. All authors read and approved the submitted version.
The authors declare that they have no conflicts of interest.
Present study was approved by our centre’s scientific research ethics committee (17/05/2022, file 433) and all study procedures were conducted in accordance with the guidelines of the Declaration of Helsinki.
Informed consent to participate in the study was obtained from all participants.
Not applicable.
The research team will share the content of the database used to conduct this study on request (carlosantonio.guillen@salud.madrid.org).
Not applicable.
© The Author(s) 2023.
Copyright: © The Author(s) 2023. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
