Affiliation:
Department of Gastroenterology, Christian Medical College Vellore, Ranipet Campus, Ranipet 632517, Tamil Nadu, India.
ORCID: https://orcid.org/0009-0002-1574-4590
Affiliation:
Department of Gastroenterology, Christian Medical College Vellore, Ranipet Campus, Ranipet 632517, Tamil Nadu, India.
ORCID: https://orcid.org/0000-0002-6059-6139
Affiliation:
Department of Gastroenterology, Christian Medical College Vellore, Ranipet Campus, Ranipet 632517, Tamil Nadu, India.
ORCID: https://orcid.org/0009-0005-6627-5167
Affiliation:
Department of Gastroenterology, Christian Medical College Vellore, Ranipet Campus, Ranipet 632517, Tamil Nadu, India.
ORCID: https://orcid.org/0000-0002-5111-7861
Affiliation:
Department of Gastroenterology, Christian Medical College Vellore, Ranipet Campus, Ranipet 632517, Tamil Nadu, India.
Email: noblehew@yahoo.com
ORCID: https://orcid.org/0009-0007-1438-5297
Explor Dig Dis. 2025;4:100596 DOI: https://doi.org/10.37349/edd.2025.100596
Received: July 04, 2025 Accepted: September 24, 2025 Published: October 11, 2025
Academic Editor: Nahum Méndez-Sánchez, National Autonomous University of Mexico, Mexico
Aim: Functional defecatory disorder (FDD) is associated with impaired defecation not only due to abnormalities in recto-anal coordination, but also due to abnormalities in anal tone and rectal sensation. This study aimed to characterize the spectrum of anorectal motor and sensory abnormalities in patients with FDD using the London classification.
Methods: In this single-center prospective study, 100 consecutive patients fulfilling Rome IV criteria for FDD were included. Secondary causes of constipation were excluded. High-resolution anorectal manometry, rectal sensory testing, and a balloon expulsion test were performed as per the International Anorectal Physiology Working Group (IAPWG) protocol. Patients were classified using the London classification, which identifies multiple subtypes of anorectal dysfunction.
Results: The median age was 34 years (range: 18–78), with 64% males and 36% females. Among the cohort, 85% had abnormal expulsion with dyssynergia, while 15% had abnormal expulsion with poor propulsion and dyssynergia. Anal hypotension with normal contractility was seen in 9%, while 4% had anal normotension with hypocontractility. Rectal hyposensitivity and borderline rectal hyposensitivity were noted in 4% and 5% of patients, respectively.
Conclusions: This study highlights that dyssynergic defecation is frequently accompanied by additional anorectal dysfunctions. Applying the London classification enhances the recognition of coexisting abnormalities, which may have therapeutic implications. Future research should investigate whether addressing these additional dysfunctions improves treatment outcomes in FDD.
Chronic constipation is one of the most common symptoms of present-day gastroenterology practice. Mertz et al. [1] showed that dyssynergic defecation constitutes up to 59% of patients with refractory chronic constipation in the United States. According to Rome IV criteria [2], functional defecatory disorder (FDD) is diagnosed in patients with functional constipation or irritable bowel syndrome when impaired defecation is demonstrated by at least two of the following: (1) abnormal balloon expulsion test, (2) abnormal anorectal evacuation pattern on manometry or anal surface electromyography (EMG), and (3) impaired rectal evacuation on imaging.
For a long time, clinicians were focusing on anorectal incoordination for the diagnosis of FDD, although patients can have co-existing anorectal sensory and motor abnormalities. During the balloon expulsion test, abnormal expulsion was attributed predominantly to anorectal muscle incoordination, although abnormalities in rectal sensitivity, anal tone, and anal contractility can contribute to abnormal balloon expulsion test [3].
With the introduction of the London classification in 2020 by the International Anorectal Physiology Working Group (IAPWG) [4], there was a significant improvement in the understanding of various anorectal dysfunctions. Multiple studies have been published based on the same classification for evaluation of anorectal disorders like chronic constipation in Parkinson’s disease [5], functional constipation and fecal incontinence [6], although data on dyssynergic defecation are scarce. This study aimed to characterize the spectrum of anorectal motor and sensory abnormalities in patients with FDD using the London classification.
We performed a single-center prospective study from November 2022 to January 2025. Consecutive patients aged > 18 years who fulfilled the Rome IV criteria for FDD, provided consent, and who did not have co-existing secondary causes for constipation (neurological disorders, uncontrolled diabetes mellitus and/or hypothyroidism, hypercalcemia, colorectal structural lesions, current pregnancy) were included in the study. Patients with prior biofeedback therapy for FDD, previous gastrointestinal, pelvic, or spinal surgeries were excluded from the study.
Patients underwent anorectal physiology testing, which includes high-resolution anorectal manometry, rectal sensory testing, and balloon expulsion test based on IAPWG protocol [4]. Anorectal manometry was done using a water-perfused high-resolution manometry system (Ready Stock). Manoeuvres in manometry included a period of stabilization, followed by rest, short squeeze, long squeeze, cough, push, and recto-anal inhibitory reflex (RAIR). The normal values were defined based on the previously published data [7, 8].
For rectal sensory testing, a rectal balloon was placed at least 3–5 cm above the upper border of the anal canal, and balloon volume was recorded for first constant sensation volume (FCSV), desire to defecate volume (DFV), and maximum tolerated volume (MTV). Rectal hyposensitivity was diagnosed when 2 or more sensory thresholds were above the upper limit of normal [4, 9]. Rectal hypersensitivity was diagnosed when at least one sensory threshold (including maximum tolerable volume) was below the lower limit of normal [4]. The normal value for rectal sensory testing was defined based on the study done by Oblizajek et al. [8].
The balloon expulsion test was done using a flexible catheter. The balloon was distended with 50 mL tepid water with the patient lying down in the left lateral position. The patient was later transferred to a private room with a commode and was asked to expel the balloon in a seated position. Abnormal balloon expulsion was defined as the inability to expel the balloon in 60 s [8].
All the patients were classified according to IAPWG classification, which included RAIR, anal hypertension, combined anal hypotension with hypocontractility, anal hypotension with normal contractility, anal normotension with hypocontractility, abnormal expulsion with normal manometric pattern of recto-anal coordination, abnormal expulsion with dyssynergia, abnormal expulsion with poor propulsion, abnormal expulsion with poor propulsion and dyssynergia, normal expulsion with abnormal manometric pattern of recto-anal coordination, rectal hyposensitivity, borderline rectal hyposensitivity, and rectal hypersensitivity. Patients were again classified as having major, minor, or inconclusive findings based on anorectal dysfunction, and a single patient could fall into multiple categories simultaneously.
This study was approved by the Institutional Review Board (Ref: Silver Ethics and Research Committee IRB Min No. 14236 dated 08.09.2021) and adhered to the 2013 version of the Helsinki Declaration. All participants provided written informed consent to participate in this study. Participants provided written informed consent to the publication of research data and results.
A sample size of 100 patients was chosen, given the exploratory nature of the study. Categorical variables were reported using frequencies and percentages. Continuous variables were expressed as median values with interquartile range.
A total of 550 patients with functional constipation were screened. 424 patients were excluded as they did not meet the Rome IV criteria for FDD. Of the remaining 126 patients, 26 were excluded owing to a prior history of biofeedback therapy, previous pelvic surgery, or refusal to provide consent. The final study cohort comprised 100 patients (Figure 1). The demographic details of the patients are described in Table 1. The median age of patients was 34 (18–78) years. Sixty-four patients were males (64%), and the median duration of constipation was 5 (1–20) years.
Baseline demographic and manometric parameters of study participants.
| Parameters (n = 100) | Value/Frequency |
|---|---|
| Age (year, median [IQR]) | 34 (18–78) |
| Sex (n, %) | |
| Male | 64 (64%) |
| Female | 36 (36%) |
| Comorbidities (n, %) | |
| Systemic hypertension | 21 (21%) |
| COPD | 8 (8%) |
| Dyslipidemia | 16 (16%) |
| Coronary artery disease | 4 (4%) |
| Rao’s type of dyssynergia (n, %) | |
| Type 1 | 79 (79%) |
| Type 2 | 1 (1%) |
| Type 3 | 19 (19%) |
| Type 4 | 1 (1%) |
| Duration of illness (years) | 5 (1–20) |
| Anal resting pressure (mmHg) | 61.5 (51–71.3) |
| Anal squeeze pressure (mmHg) | 146 (116–175) |
| Anal pressure during strain (mmHg) | 77.1 (63.5–95.5) |
| Rectal basal pressure (mmHg) | 8.8 (6.0–12.1) |
| Rectal pressure during strain (mmHg) | 50 (39.4–60.6) |
| Rectal pressure increment during strain (mmHg) | 43.4 (33.9–57.5) |
| Anal pressure decrement during strain (mmHg) | –13.2 (–30.9 to –2) |
| First sensation (mL) | 30 (20–40) |
| Urge for defecation (mL) | 120 (100–170) |
| Discomfort (mL) | 180 (160–220) |
IQR: interquartile range; COPD: chronic obstructive pulmonary disease.
Anal hypotension with normal contractility was noted in 9 patients (9%), and anal normotension with hypocontractility in 4 (4%). Abnormal expulsion with dyssynergia was noted in 85 patients (85%), and abnormal expulsion with poor propulsion and dyssynergia was noted in 15 (15%). Four patients had rectal hyposensitivity (4%) and five showed borderline rectal hyposensitivity (5%). None of the patients had absent recto-anal areflexia, abnormal expulsion with normal manometric pattern of recto-anal coordination, abnormal expulsion with poor propulsion, normal expulsion with abnormal manometric pattern of recto-anal coordination, or rectal hypersensitivity (Table 2). 75% (n = 75) of patients had only one type of anorectal dysfunction. However, 23% (n = 23) of patients had two types of anorectal dysfunction, and 2% (n = 2) of patients had three types of anorectal dysfunction (Figure 2).
Frequency of anorectal disorders among participants based on the London classification.
| Parameter | Frequency (%) |
|---|---|
| Disorder of the recto-anal inhibitory reflex | |
| Recto-anal areflexia (n, %) | 0 (0%) |
| Disorders of anal tone and contractility | |
| Anal hypertension (n, %) | 2 (2%) |
| Combined anal hypotension and hypocontractility (n, %) | 1 (1%) |
| Anal hypotension with normal contractility (n, %) | 9 (9%) |
| Anal normotension with hypocontractility (n, %) | 4 (4%) |
| Disorders of recto-anal coordination | |
| Abnormal expulsion with normal manometric pattern of recto-anal coordination (n, %) | 0 (0%) |
| Abnormal expulsion with dyssynergia (n, %) | 85 (85%) |
| Abnormal expulsion with poor propulsion and dyssynergia (n, %) | 15 (15%) |
| Abnormal expulsion with poor propulsion (n, %) | 0 (0%) |
| Normal expulsion with abnormal manometric pattern of recto-anal coordination (n, %) | 0 (0%) |
| Disorders of rectal sensation | |
| Rectal hyposensitivity (n, %) | 4 (4%) |
| Borderline rectal hyposensitivity (n, %) | 5 (5%) |
| Rectal hypersensitivity (n, %) | 0 (0%) |
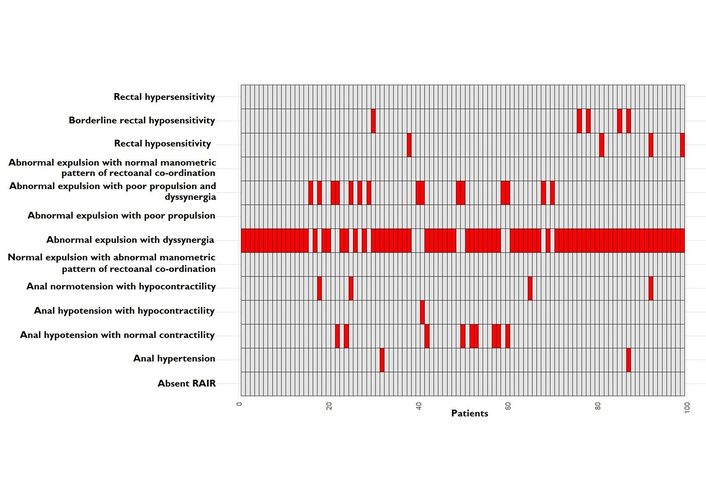
Distribution of multiple anorectal abnormalities among patients with functional defecatory disorder. RAIR: recto-anal inhibitory reflex.
Also, twelve patients (12%) had a major finding, all patients had a minor finding (100%), and five patients (5%) had an inconclusive finding (Table 3). Since patients could have more than one finding, 20% (n = 20) patients had major and minor findings, 5% (n = 5) patients had minor and inconclusive findings, and 75% (n = 75) patients had only minor findings (Figure 3).
Frequency of anorectal dysfunction among participants based on major, minor, and inconclusive findings.
| Findings | Frequency (%) |
|---|---|
| Major | 12 (12%) |
| Minor | 100 (100%) |
| Inconclusive | 5 (5%) |
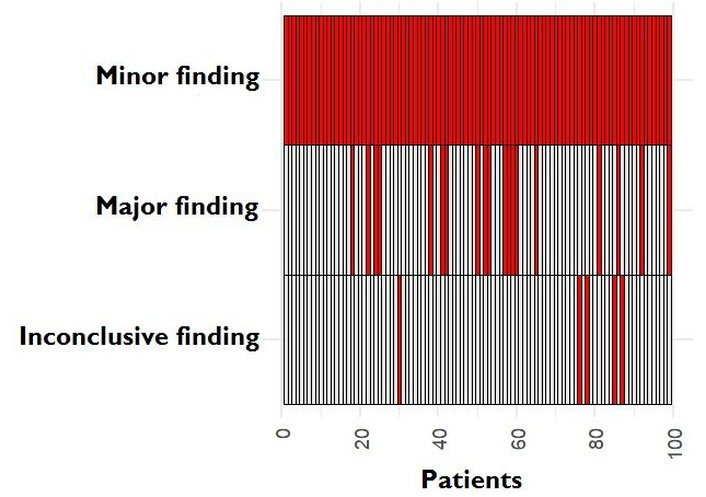
Distribution of major, minor, and inconclusive findings among the patients with functional defecatory disorder.
Our study shows that multiple types of anorectal dysfunction can co-exist with dyssynergic defecation. None of our patients had absent RAIR, as we only included patients with dyssynergic defecation and excluded the pediatric population from the study [10]. The multicenter study done by Vollebregt et al. [6] in 309 patients with chronic constipation also showed absent RAIR in only 1.8% patients.
Among patients with disorders of anal tone and contractility, a significant number of patients with dyssynergia had abnormal anal tone and/or contractility. In the study done by Vollebregt et al. [6], 45% patients had abnormality in anal tone and contractility, as opposed to 16% in our study. In our cohort, 14% of patients had anal hypotension, hypocontractility, or both, whereas only 2% had anal hypertension. This suggests that baseline anal pressures may not reliably predict the degree of anal relaxation during defecation. However, further studies with larger sample sizes are required to validate this finding.
All our patients had abnormality in recto-anal coordination, which was expected as the presence of dyssynergia and abnormal balloon expulsion was a mandatory inclusion criterion. For the same reason, none of the patients had abnormal expulsion with normal manometric pattern of recto-anal coordination, abnormal expulsion with poor propulsion, or normal expulsion with abnormal manometric pattern of recto-anal coordination. Whether all these patients respond similarly to biofeedback therapy is a question that warrants further studies.
It is well known that rectal hyposensitivity is associated with the severity of chronic constipation [11]. Rectal hyposensitivity was noted in 4% (n = 4), and borderline rectal hyposensitivity was noted in 5% (n = 5) of patients with dyssynergia in our study. The study by Vollebregt et al. [6] showed that the presence of rectal hyposensitivity and borderline rectal hyposensitivity are 10% and 10.7% respectively, in patients with chronic constipation. It is already known that sensory training with biofeedback therapy and sacral neuromodulation improves outcomes in chronic constipation [12, 13]. Hence, incorporating sensory training alongside biofeedback therapy in patients with rectal hypotension and dyssynergia may enhance treatment outcomes in chronic constipation.
Our study has several strengths. It is among the first studies to classify anorectal dysfunctions in dyssynergic defecation using the London classification. Thorough focus on patients meeting the Rome IV criteria for FDD and prospective design of the study are other strengths. However, there are limitations to consider. The exploratory nature and limited sample size in this study may have led to an underestimation of the true prevalence of rarer anorectal abnormalities. The lack of a control group is another limitation of the study. Also, the study was conducted at a single center, which may restrict the generalizability and external validity of our results.
In conclusion, various other disorders of anorectal function coexist with dyssynergia in patients with FDD. Applying the London classification to reporting helps to uncover aspects of anorectal dysfunction that require attention and were otherwise ignored. In addition, further multi-center studies are warranted to obtain external validation and identify how addressing these aspects of anorectal dysfunction in patients with FDD can influence patient outcomes.
FDD: functional defecatory disorder
IAPWG: International Anorectal Physiology Working Group
RAIR: recto-anal inhibitory reflex
The authors gratefully acknowledge the contributions of Mrs. Yugalakshmi, motility nurse, for her assistance in patient preparation and data collection, and Mrs. Jansi Rani, statistician, for her support in statistical analysis and data interpretation.
SB: Conceptualization, Data curation, Methodology, Project administration, Supervision, Validation, Writing—original draft. RJ: Conceptualization, Supervision, Writing—original draft. AKC: Data curation, Project administration, Formal analysis, Writing—review & editing. AKD: Conceptualization, Supervision, Formal analysis, Writing—review & editing. NVM: Conceptualization, Methodology, Formal analysis, Project administration, Supervision, Writing—review & editing, Investigation, Visualization. All authors read and approved the submitted version.
The authors declare that they have no conflicts of interest.
The study was approved by the Institutional Review Board (Ref: Silver Ethics and Research Committee IRB Min No. 14236 dated 08.09.2021) and adhered to the 2013 version of the Helsinki Declaration.
Written informed consent to participate in the study was obtained from all participants.
Written informed consent to publication of research data and results was obtained from participants.
Data will be available from the corresponding author upon reasonable request.
Not applicable.
© The Author(s) 2025.
Open Exploration maintains a neutral stance on jurisdictional claims in published institutional affiliations and maps. All opinions expressed in this article are the personal views of the author(s) and do not represent the stance of the editorial team or the publisher.
Copyright: © The Author(s) 2025. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 2324
Download: 22
Times Cited: 0
