Affiliation:
1Academic Rheumatology, School of Medicine, University of Nottingham, NG5 1PB Nottingham, UK
Email: arnair278@gmail.com
ORCID: https://orcid.org/0000-0002-8775-6892
Affiliation:
2Division of Population Health, Health Services Research and Primary Care, Faculty of Biology, Medicine and Health, School of Health Sciences, University of Manchester, M13 9PL Manchester, UK
ORCID: https://orcid.org/0000-0001-6429-988X
Affiliation:
1Academic Rheumatology, School of Medicine, University of Nottingham, NG5 1PB Nottingham, UK
ORCID: https://orcid.org/0000-0003-1142-1460
Affiliation:
1Academic Rheumatology, School of Medicine, University of Nottingham, NG5 1PB Nottingham, UK
ORCID: https://orcid.org/0000-0002-5763-8326
Affiliation:
1Academic Rheumatology, School of Medicine, University of Nottingham, NG5 1PB Nottingham, UK
ORCID: https://orcid.org/0000-0003-0121-4919
Explor Musculoskeletal Dis. 2023;1:68–76 DOI: https://doi.org/10.37349/emd.2023.00011
Received: December 16, 2022 Accepted: May 08, 2023 Published: June 30, 2023
Academic Editor: Reinhard Graf, Academic hospital Stolzalpe, Austria
Aim: To identify constitutional morphological features at the knee that associate with knee osteoarthritis (OA, KOA).
Methods: This was a case-control study using data from the Genetics of Osteoarthritis and Lifestyle (GOAL) study. Radiographic measurements at the knee were undertaken by a single trained observer. Measurement of 12 characteristics was undertaken in 815 controls with asymptomatic structurally normal knees to examine right-left symmetry and variation with gender and age. Measurements were then compared to “cases” (315 asymptomatic and structurally unaffected knees of people with radiographic and symptomatic OA in the contralateral knee) on the assumption that the morphology of the unaffected knee represented the morphology of the contralateral knee prior to the development of OA. Right-left symmetry of morphological measures in controls was examined using paired t test and minimal detectable change (MDC). Linear regression was used to examine the association between measurements and demographic characteristics. Association of morphological features and unilateral KOA [defined as OA in either patellofemoral (PF) or tibiofemoral (TF) joints], PFOA and TFOA were determined using binary logistic regression and odds ratio (OR) and 95% confidence interval (CI) calculated. Cumulative risk of measurements in determining OA was examined using receiver operating characteristic (ROC) curves.
Results: Narrow sulcus and condylar angles, increasing distal femoral, proximal tibial tilt, and increasing varus alignment associated with KOA. ROC curves including all significant morphological features and age, gender, height, and weight predicted knee, PF joint (PFJ), and TF joint (TFJ) OA with area under the curve (AUC) of 0.91, 0.89, and 0.90 respectively. On the contrary, a model only containing age, gender, height, and weight predicted knee, PFJ, and TFJ OA with AUC of 0.59, 0.67, and 0.59 respectively.
Conclusions: Five morphological features associated independently with KOA were identified. Together they explain a large proportion of risk for OA.
Osteoarthritis (OA) is a common complex disorder with multiple genetic, constitutional, and environmental risk factors [1]. The knee is a commonly affected joint and results in a significant healthcare burden [2, 3]. Knee OA (KOA) shows familial clustering and has relatively high heritability (40–60%), though the mechanisms for inherited predisposition remain unclear [4, 5]. Rare monogenic disorders that cause severe developmental abnormality of joint shape can result in early-onset OA, and there is growing interest in the possibility that more subtle variations in joint shape may explain some of the heritability in KOA [6]. Variations in joint shape as a risk factor for OA have been studied mainly at the hip, where non-spherical head [6], extremes of neck-shaft angle [6], and acetabular dysplasia [7] are reported to be associated with hip OA. To date, only a few morphological features at the knee have been associated with OA. These include varus-valgus knee malalignment [8], sulcus angle [9], high Insall-Salvati ratio [10], and laterally displaced patella [9]. However, most studies have limitations such as small sample size, focus on just one or two measurements, an emphasis on progression rather than development of OA, or the use of active shape modelling that is difficult to utilise in routine clinical settings.
Therefore, the authors in the study sought to examine a range of individual morphological variations that can be assessed readily on knee radiographs as risk factors for knee OA. The objectives of this study were to: (1) examine whether the morphologic measurements are symmetric between the right and left knees in the absence of knee OA; (2) examine whether these features vary with age, sex, weight, and height; (3) determine whether these features independently are associated with knee OA; and (4) explore the cumulative risk explained by them.
In this study, symmetry of knee morphology was examined in participants that had knees unaffected by radiographic OA and without any self-reported knee pain. We assumed that if participants without knee OA exhibit symmetry of morphological measures between right and left knees, it can reasonably be inferred that the unaffected knee of people with unilateral knee OA represents the morphology of the affected knee before the onset of OA. Hence in this study, the unaffected knee of participants with unilateral knee OA was defined as the “case knee” and compared to the “control knee” of the same side in people without knee OA. A similar strategy has been used previously to examine the associations between hip morphology and OA [5–7].
This was a case-control study using data from the Genetics of Osteoarthritis and Lifestyle (GOAL) study. GOAL was established as a case-control study of 45- to 80-year-old Caucasians that recruited 1,042 participants with clinically severe KOA, 1,007 with clinically severe hip OA, and 1,121 participants without hip or knee OA, living in or around Nottingham. Ethical approval was granted by the Nottingham City Hospital Local Research Ethics Committee (reference EC02/06) in February 2002. The project was funded by AstraZeneca, UK as a collaborative project with the University of Nottingham, UK.
KOA cases were recruited from hospital orthopedic surgery lists and from a rheumatology OA clinic. All cases had been referred to hospital with symptomatic, clinically severe KOA, and the majority had undergone unilateral or bilateral total joint replacement within the previous 5 years. Controls were defined as individuals without symptoms, signs, or radiographic evidence of OA at both knees and hips. Control participants were recruited from lists of people who were referred to hospital for intravenous urography (IVU). Individuals who did not have radiographic hip OA on their screening IVU radiograph had no knee or hip symptoms, and did not have any exclusion criteria were invited to participate. Full details of the GOAL study have been published elsewhere [6]. All participants underwent bilateral knee radiographs—skyline views of the patellofemoral (PF) compartment in 30 degrees flexion, and standing, flexed posterior-anterior knee radiographs using a Rosen Template to standardise knee flexion and foot rotation [11].
Cases were selected from participants with unilateral knee OA, where the unaffected knees with no knee pain and no radiographic OA were used as “case knees”. Control knees were selected from the control group where both knees had no knee pain or radiographic OA. Absence of radiographic knee OA was defined as summated tri-compartment scores for joint space narrowing (JSN) and osteophyte of 0 and 0 or 1, respectively, using the Nottingham Line Drawing Atlas [12].
All radiographic measurements were undertaken using the HIPAX computerised software (Hipax Dicom 4.2, Vorsetetten, Germany). This allows measurement of degrees and lengths in millimetres correct to two decimal points. Nine morphological features at the PF and three at the tibiofemoral (TF) compartments were measured by Nair A. These were:
Angular measurements: sulcus angle, patellar angle, condylar angle, distal femoral tilt, condylar plateau angle, and proximal tibial tilt.
Linear measurements: patellar width, patellar thickness, medial condylar height, lateral condylar height, intercondylar width, and condylar width.
Varus and valgus alignment were measured by another assessor (Abhishek A) previously [13] using the method described by Krause et al. Please see Supplementary materials (Figures S1–S11) for details of the methods used for the measurements.
Mean [standard deviation (SD)] and n (%) were used for descriptive purposes. Intra-rater reliability was determined by undertaking repeated measurements on a random sample of 20 knee radiographs (10 right and 10 left) with the observer blind to the initial scores. This was repeated on different sets at the beginning, middle and end of the period of measurement. Two-way intra-class correlation coefficient (ICC) for absolute agreement was used to determine reliability [14].
All measurements in the control knees were examined for right-left symmetry using descriptive statistics, paired t test, mean difference and 95% confidence interval (CI), and the minimal detectable change (MDC). The MDC is defined as the minimum change required to distinguish true change from a change due to variability in performance of the test or due to error in measurement [15]. This was calculated by multiplying the standard error of the measurement (SEM) by the z score of 90% confidence level and the square root of 2 (MDC = z-score90 × SEM × √2). SEM measures the amount of error in the measurement and was calculated using the formula: SEM = s√(1 – r), where, s is the SD of the first and second measurements and r is the ICC [16]. Measurements were defined as being symmetric if the mean difference between the left and right sides was less than the MDC90.
Association of morphological measures and age, gender, height, and weight was examined using multivariate linear regression using data from the control knees. Logistic regression was used to examine the association between morphological features and KOA. Measurements in the unaffected knees of the cases were compared to the same side of the control, hence 315 cases and 315 controls were included in the analysis. The proportion of right versus left knees was matched with the case group. For this analysis, knee OA was defined as present if there was either TFOA or PFOA. Subgroup analyses were conducted restricted to PFOA (defined as only PFOA) or TFOA (defined as only TFOA). Morphological features were adjusted for each other and for age, gender, height, and weight [17]. Adjusted odds ratio (OR) and 95% CI were calculated.
Three receiver operating characteristic (ROC) curve analyses were undertaken for KOA, PFOA, and TFOA, each including the following variables: As distal femoral and proximal tibial tilt were correlated (r = 0.54), only distal femoral tilt was included in the prediction model.
(1) morphological features that were significantly associated with KOA;
(2) morphological features that were significantly associated with KOA and age, gender, height, and weight; and
(3) age, gender, height, and weight alone.
Area under the curve (AUC) and 95% CI for each model were presented. Data management and statistical analysis were conducted using STATA version 15 (StataCorp LLC, Texas, USA). Bonferroni correction was undertaken for multiple testing, with P < 0.003 defined as statistically significant.
Data for 408 controls without KOA and 315 cases with unilateral KOA were included in this study (Table 1). Cases were significantly more likely to be female, be older in age, and have a higher body mass index. The measurements in the right and left knees of the normal controls were comparable in magnitude (Table 2). After correcting for multiple testing, condylar plateau angle, condylar width, patellar width, and sulcus angle were significantly different between the right and left sides (P < 0.001). However, the absolute magnitude of these differences was small and they were less than the MDC (Table 2).
Characteristics of the study participants
| Demographic characteristics | Controls (n = 408) | Cases (n = 315) | P value |
|---|---|---|---|
| Age (years)1 | 62.10 (8.57) | 64.00 (8.60) | < 0.001 |
| Weight (kg)1 | 76.95 (15.72) | 78.30 (14.41) | 0.41 |
| Height (cm)1 | 167.57 (11.10) | 166.70 (14.20) | 0.31 |
| BMI (kg/m2)1 | 27.8 (10.65) | 30.1 (20.08) | 0.01 |
| Women (%)1 | 54% | 59% | 0.03 |
1Continuous variables summarised as mean (SD). BMI: body mass index
Tests for symmetry in controls knees
| Measurements | Right knee Mean (SD) | Left knee Mean (SD) | Mean difference | P value | MDC 90% level Left knee | MDC 90% level Right knee |
|---|---|---|---|---|---|---|
| Sulcus angle1 | 141.40 (5.32) | 142.5 (5.39) | 1.07 | < 0.001 | 3.25 | 3.14 |
| Patella angle1 | 135.27 (6.34) | 135.3 (6.80) | 0.03 | 0.89 | 3.84 | 3.16 |
| Condylar angle1 | 14.01 (9.15) | 14.88 (2.80) | 0.87 | 0.05 | 3.36 | 3.84 |
| Patella thickness1 | 23.19 (3.11) | 23.36 (2.60) | 0.16 | 0.18 | 3.70 | 3.15 |
| Patella width1 | 49.04 (6.45) | 48.2 (6.07) | –0.76 | < 0.001 | 3.80 | 3.72 |
| Condylar height lateral1 | 7.11 (1.70) | 6.8 (1.410) | –0.24 | 0.26 | 1.64 | 2.70 |
| Condylar height medial1 | 8.82 (1.95) | 9.05 (2.20) | 0.22 | 0.31 | 2.86 | 3.05 |
| Condylar width1 | 65.77 (6.72) | 65.05 (7.00) | –0.71 | < 0.001 | 3.35 | 2.82 |
| Intercondylar width1 | 46.63 (5.70) | 46.40 (5.25) | –0.20 | 0.18 | 3.01 | 1.81 |
| Condylar plateau angle1 | 5.42 (0.93) | 5.63 (1.00) | 0.21 | < 0.001 | 0.88 | 1.23 |
| Distal femoral tilt1 | 2.73 (1.51) | 2.60 (1.57) | –0.12 | 0.08 | 3.39 | 3.37 |
| Proximal tibial tilt1 | 2.35 (1.03) | 2.51 (1.13) | 0.16 | 0.12 | 2.04 | 1.81 |
| Anatomical axis1 | 179.83 (1.25) | 179.89 (1.26) | –0.06 | 0.20 | 1.16 | 1.16 |
1All angles measured in degrees, and all dimensions in millimetres
The majority of measurements were not associated with age, sex, height, or weight (Tables S1 to S5). However, patellar width was associated with height [β coefficient (βcoef) = 0.4; 95% CI 0.3, 0.42] and weight [βcoef = 0.05; 95% CI 0.01, 0.1]. Patellar thickness was associated with age [βcoef = 0.01; 95% CI 0.04, 0.3] and, patellar width [βcoef = –2.5; 95% CI –4, –0.93] and condylar width [βcoef = –3.33; 95% CI –4.5, –2.15] were associated negatively with female gender. Valgus knee alignment was associated with age and varus alignment with weight (Table S5).
Narrow sulcus angle, narrow condylar angle, increasing proximal tibial tilt, and varus alignment were associated with KOA (Table 3). All these measurements and distal femoral tilt were associated with TFOA. Only sulcus angle and condylar angle were associated with PFOA. ROC curves including all significant morphological features and age, gender, height, and weight carried a high cumulative risk of KOA, PFOA, and TFOA with an AUC of 0.91 (95% CI 0.89, 0.93), 0.91 (95% CI 0.86, 0.95), and 0.91 (95% CI 0.89, 0.93), respectively (Figure 1). In contrast, a model containing only age, gender, height, and weight predicted KOA, PFOA, and TFOA with AUC of 0.59 (95% CI 0.54, 0.63), 0.67 (95% CI 0.60, 0.74), and 0.59 (95% CI 0.54, 0.63), respectively.
Association between morphological features and OA
| Measurements | Knee OA* | PFOA* | TFOA* |
|---|---|---|---|
| Sulcus angle1 | 0.83 (0.80, 0.87)2 | 0.86 (0.81, 0.91)2 | 0.86 (0.82, 0.91)2 |
| Condylar angle1 | 0.52 (0.48, 0.58)2 | 0.48 (0.41, 0.56)2 | 0.52 (0.42, 0.57)2 |
| Intercondylar width1 | 0.97 (0.93, 1.01) | 0.95 (0.87, 1.05) | 1.37 (1.20, 1.57)2 |
| Distal femoral tilt1 | 1.08 (0.96, 1.22) | 0.99 (0.92, 1.07) | 1.38 (1.15, 1.64)2 |
| Proximal tibial tilt1 | 1.21 (1.02, 1.44) | 0.98 (0.55, 0.90) | 0.96 (0.87, 1.05) |
| Patellar thickness1 | 0.93 (0.86, 1.0) | 0.95 (0.81, 1.1) | 0.98 (0.95, 1.02) |
| Patellar width1 | 0.97 (0.94, 1.0) | 1.14 (1.00, 1.31) | 0.86 (0.75, 1.98) |
| Condylar height medial1 | 1.15 (0.02, 1.3) | 0.95 (0.92, 1.0) | 1.23 (0.01, 1.35) |
| Condylar height lateral1 | 0.79 (0.71, 1.8) | 0.93 (0.88, 0.99) | 0.97 (0.93, 1.01) |
| Condylar width1 | 1.02 (0.99, 1.05) | 0.88 (0.64, 1.21) | 0.93 (0.89, 0.98) |
| Intercondylar width1 | 0.97 (0.93, 1.00) | 1.08 (0.89, 1.30) | 1.02 (0.83, 1.25) |
| Condylar plateau angle1 | 0.96 (0.80, 1.2) | 1.18 (0.92, 1.52) | 3.92 (2.44, 6.29)2 |
| Varus alignment1 | 3.06 (1.95, 4.82)2 | 2.67 (1.24, 5.72) | 2.09 (1.24, 3.52)2 |
| Valgus alignment1 | 1.90 (1.17, 3.08) | 1.25 (0.47, 3.33) | 0.86 (0.82, 0.91)2 |
* Adjusted OR (95% CI) for age, sex, height, weight, and any other morphological features in the table. 1 All angles measured in degrees, and all distances in millimetres; 2 significant after Bonferroni correction at P < 0.003
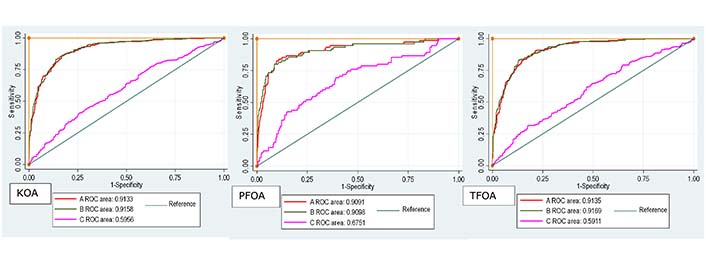
ROC curve for KOA, PFOA, and TFOA. Curve A plotted with only morphological features; Curve B plotted with morphological features + demographic features; Curve C plotted with demographic features only
This is the largest study to date to investigate knee morphological features that predispose to KOA, and the first to separately investigate the PF and TF compartments. This study identified five morphological features that were associated with increased risk of KOA, specifically smaller sulcus angle, smaller condylar angle, larger distal femoral tilt, larger proximal tibial tilt, and varus malalignment. These associations were independent of age, gender, height, and weight. Larger distal femoral tilt, proximal tibial tilt and varus malalignment were associated with TFOA but not with PFOA. However, smaller sulcus angle and condylar angle were associated with both PFOA and TFOA. Addition of these morphological features to a risk prediction model containing age, gender, height, and weight greatly enhanced the predictability for KOA, suggesting a substantial role of these features in prediction of KOA. Such constitutional features might also explain much of the heritability of KOA. Morphological features of unaffected knees of unilateral knee OA participants were compared with non-OA controls on the assumption that the unaffected knee of people with unilateral KOA represents the constitutional shape of the affected knee prior to development of OA. This strategy was supported by the right-left symmetry demonstrated for all morphological features in the controls without OA. Some of the linear measurements but none of the angular measurements varied with age, height, weight, and gender. This suggests that such demographic factors mainly influence a proportional change in the size of different bones whilst still maintaining the relative proportions and alignment.
The findings of this study, that a wide sulcus angle is associated with a lower risk of KOA accords with three previous studies [18–20]. However, two other studies, one using magnetic resonance imaging (MRI) [21] and one using radiographs [22] have reported that a wider sulcus angle is associated with KOA. This disparity might result from the use of a different anatomical location on the femoral condyle for measuring sulcus angle in the first study [21], and from the use of weight-bearing skyline PF views and a focus on progression rather than the development of KOA in the second study [22]. The association between knee malalignment and KOA has been reported previously [8, 22, 23], with varus alignment particularly being a strong risk factor for KOA.
There are some plausible biomechanical explanations as to why these morphological variants may predispose to KOA. For example, a wider sulcus angle provides a better area for articulation with the patella, thereby reducing PF contact stress and providing an optimal retro-patellar joint load [18–20]. Also, a narrower condylar angle suggests a more laterally placed patella, and during knee movement a laterally placed patella would be compressed against the lateral femoral condyle instead of distributing load evenly between the lateral and medial PF compartments, leading to excessive contact forces mainly on the lateral PF compartment [24]. A wider distal femoral tilt can cause the patellar tendon to be abnormally twisted and exert more PF force on the patella [25]. As the proximal tibial slope increases, the increased anterior tibial translation increases stress on the anterior cruciate ligament. For instance, the loading increases by 136 Newtons for a 5° increase in proximal tibial tilt, and by 460 Newtons for 10° increase [26]. Varus alignment increases adduction thereby increasing the quadriceps angle (Q-angle), which exerts more stress to the medial PF and TF compartments with possible subsequent detrimental effects [8].
There are several limitations to this study. Firstly, being cross-sectional in nature it can only demonstrate association and not causation. A prospective study is required to confirm causality. Secondly, two-dimensional images were used in the study, although a standardized protocol was used, variability in positioning may have influenced the assessments. Also plain radiographs are insensitive at identifying early changes of KOA [17], so some knees that were classified as normal control knees may have had undetected mild structural OA. This is unlikely to play a significant part as the control participants of the study did not report any knee pain. KOA is predominantly bilateral and it is possible that the apparently unaffected knee had undergone early bone remodeling and morphological alterations, e.g., increase in size of the bones, as part of OA prior to occurrence of other OA features, such as osteophyte and narrowing, which are evident on radiographs. This may have been encouraged by alteration in biomechanics caused by clinically severe OA in the contralateral knee [27]. Similarly, any trauma attained on the knees can alter the normal joint biomechanics which could in turn affect the predictability of these phenotypes. Thirdly, GOAL is a hospital-based study of Caucasian people in one region of the UK, so the generalisability of the findings to other populations remains in question, and further studies in other populations are required. Also, being hospital-based and not a random population sample, there may have been selection bias, especially with respect to the non-OA control group. The study hypothesize that these abnormal measurements are constitutional risk factors for the development of knee OA, hence for future prospective studies it is important to include and adjust for the variation in these morphological features. Future prospective studies should include more sensitive imaging techniques, such as MRI or computed tomography (CT), to detect and measure bone changes and provide three dimensional details. Also, the application of statistical shape models in future studies can help in describing the variation in whole knee joint geometry with respect to OA and so may be better at predicting knee OA development with better sensitivity and specificity. Future studies should also investigate further role of genetics in variation of bone shape that predates OA, using research methods such as Mendelian randomization that can aid in establishing causal effects of exposure on the disease without being affected by confounders.
This study has identified five morphological features such as sulcus angle, condylar angle, varus malalignment, and proximal and distal femoral tilt that can be measured readily on standard radiographs, which independently associate with KOA and may explain much of its occurrence. These angular and linear measures of knee could be used in the clinical setting to identify those who are vulnerable to developing knee OA. Early intervention and disease prevention techniques such as weight loss, strengthening exercise, and minimization of specific activities that may cause adverse biomechanical stress could be advised to such people at high risk. Prospective studies are required to provide further support for causality.
AUC: area under the curve
CI: confidence interval
GOAL: Genetics of Osteoarthritis and Lifestyle
KOA: knee osteoarthritis
MDC: minimal detectable change
OA: osteoarthritis
PF: patellofemoral
PFJ: patellofemoral joint
PFOA: patellofemoral osteoarthritis
ROC: receiver operating characteristic
SD: standard deviation
SEM: standard error of the measurement
TF: tibiofemoral
TFJ: tibiofemoral joint
TFOA: tibiofemoral osteoarthritis
βcoef: β coefficient
The supplementary material for this article is available at: https://www.explorationpub.com/uploads/Article/file/100711_sup_1.pdf.
We are grateful to all the participants for taking part in the GOAL study and to all staff involved in the organisation and logistics of the study.
ARN, KM, WZ, MD, AA: Data curation, Writing–original draft, Writing–review & editing. All authors approved the final submitted manuscript.
The authors declare that they have no conflicts of interest.
The GOAL study was granted by the Nottingham City Hospital Local Research Ethics Committee (reference EC02/06).
Informed consent to participate in the study was obtained from all participants.
Informed consent to publication was obtained from relevant participants.
All datasets are available on request.
Not applicable.
© The Author(s) 2023.
Copyright: © The Author(s) 2023. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
