Affiliation:
1Department of Mathematics and Computer Science, University of Catania, 95125 Catania, Italy
2Department of Educational Sciences, Section of Psychology, University of Catania, 95123 Catania, Italy
Email: mirko.casu@live.it
ORCID: https://orcid.org/0000-0001-6975-2241
Affiliation:
2Department of Educational Sciences, Section of Psychology, University of Catania, 95123 Catania, Italy
3Center of Excellence for the Acceleration of Harm Reduction (CoEHAR), University of Catania, 95121 Catania, Italy
ORCID: https://orcid.org/0000-0001-7414-155X
Explor Digit Health Technol. 2024;2:46–58 DOI: https://doi.org/10.37349/edht.2024.00010
Received: October 23, 2023 Accepted: February 03, 2024 Published: March 28, 2024
Academic Editor: Subho Chakrabarti, Postgraduate Institute of Medical Education and Research (PGIMER), India
The article belongs to the special issue Telepsychiatry in Low-and Middle-income Countries: an Update
The paper aimed to provide a comprehensive overview of the use of digital health technologies in the assessment, treatment, and self-management of psychological and psychopathological factors associated with asthma. A collection of research articles and systematic reviews related to asthma, including topics such as outdoor air pollution, early life wheezing illnesses, atopic dermatitis, digital interventions for asthma self-management, psychiatric disorders and asthma, family influences on pediatric asthma, and the use of mobile health (mHealth) applications for asthma management, were analyzed. Eight selected studies were reviewed to assess the potential of digital health technologies in improving asthma psychological-related factors management and treatment outcomes. The reviewed studies suggest that electronic health (eHealth) interventions, mixed reality tools, mHealth technology-enhanced nurse-guided interventions, and smartphone applications integrating Bluetooth-enabled sensors for asthma inhalers can significantly improve symptom self-management, quality of life, and mental health outcomes, especially in children and adolescents with asthma (JMIR Pediatr Parent. 2019;2:e12427. doi: 10.2196/12427; Cochrane Database Syst Rev. 2018;8:CD012489. doi: 10.1002/14651858.CD012489.pub2; Int J Environ Res Public Health. 2020;17:7750. doi: 10.3390/ijerph17217750; J Med Internet Res. 2017;19:e113. doi: 10.2196/jmir.6994; J Med Internet Res. 2021;23:e25472. doi: 10.2196/25472; Ann Allergy Asthma Immunol. 2015;114:341–2.E2. doi: 10.1016/j.anai.2014.12.017; J Med Internet Res. 2022;24:e38030. doi: 10.2196/38030; Int J Qual Methods. 2021;20:16094069211008333. doi: 10.1177/16094069211008333). However, further research is needed to determine their effectiveness and feasibility in different populations and settings. Tailored interventions that address the specific needs and preferences of patients with asthma and associated psychological factors are crucial for ensuring sustained and equitable use of these technologies. The manuscript emphasizes the importance of addressing psychological factors in the management and treatment of asthma and call for continued research and development in this area.
Asthma is a chronic respiratory disease that affects both children and adults, caused by inflammation and muscle tightening around the airways, making breathing harder. The World Health Organization (WHO) has indicated that asthma is frequently not properly diagnosed or treated, especially in countries with low to medium income levels [1]. There are between 100 million and 150 million people suffering from this condition worldwide and deaths associated with the disease, again according to WHO, around 180 thousand each year [2]. In Italy, asthma has a prevalence of about 10% in the pediatric population and 2% of asthmatic children and adolescents suffer from severe asthma [3, 4]. Among the Italian adult population, asthma was found to have a prevalence of about 8.4% [5]. The main causes and risk factors for asthma include genetic factors [6], environmental factors [7], respiratory infections [8], and atopy [9]. The advent of new technologies has led to the introduction of new effective treatment methods in clinical settings, including short message service-based interventions [10], smartphone applications (apps) [11], virtual reality (VR) and augmented reality (AR) [12, 13], and the use of commercial video games [14]. All these are included in electronic health (eHealth) and mobile health (mHealth) categories, which can be defined as follows: eHealth includes the use of information and communication technologies for health, such as eHealth records, personal health records, and clinical decision support tools, while mHealth includes the medical and public health practice supported by mobile devices, such as mobile phones, patient monitoring devices, personal digital assistants, and other wireless devices, such as mHealth apps and wearables [15]. Regarding asthma, the new digital interventions aim to improve asthma management, self-monitoring, and adherence to treatment plans. They have been well received by patients, who generally appreciate the usability of such tools and show the desire to continue treatments [16–18], thus improving adherence. Specifically, multifunctional mHealth apps showed promise in controlling asthma and enhancing patients’ quality of life compared to traditional interventions [19]; also, digital inhaler health platforms, which use digital inhalers to track the timing and date of dosage, served as an effective tool for managing both asthma and medication [20]. These platforms fostered a cooperative care environment between healthcare providers and patients and offered a more detailed understanding of actual inhaler usage, demonstrating potential, with evidence indicating positive effects on various outcomes, including knowledge, limitations in activity, self-care, quality of life, and medication usage [21]. Behind the creation of digital interventions are often psychological models and theories designed to improve their impact and utilization, guiding their optimal design and delivery [22]. Theory-based digital interventions can, in fact, improve asthma self-management outcomes, such as medication adherence, asthma control, and quality of life [23].
Remaining within the realm of psychology, it is known that various psychological and psychopathological factors can influence asthma: Individuals with asthma often experience comorbidities, showing a higher prevalence of anxiety and depressive disorders compared to the general population [24]. These psychological factors can negatively impact asthma control, adherence to treatment, and overall quality of life [25]. Stress can exacerbate asthma symptoms, and stress management interventions may help improve asthma outcomes [26]. Additionally, the relationship between asthma and psychological factors can be bidirectional: Not only do psychological factors influence asthma symptoms, but asthma symptoms can also lead to increased psychological distress [27]. Parental psychological factors can also impact children’s asthma outcomes. Specifically, parental anxiety and depression were associated with poorer asthma control in children [28]. Overall, these studies demonstrate the complex interplay between psychological and psychopathological factors and asthma, emphasizing the importance of addressing these factors in the management and treatment of asthma [24–28]. The paper’s contribution to the existing literature on digital health interventions (DHIs) for managing asthma-related psychological factors is also summarized, as presented in Table 1.
Problem or issue addressed, what is already known, and the unique contribution of the paper to the existing literature
| Problem or issue | What is already known | What this paper adds |
|---|---|---|
| Management of psychological factors associated with asthma using digital health technologies. | Previous research has demonstrated the possible advantages of eHealth strategies, mixed reality instruments, and mobile apps in enhancing the management of symptoms, life quality, and mental health results. | Digital health technologies have been found to significantly enhance symptom self-management, improve quality of life, and positively impact mental health outcomes, especially in children and adolescents with asthma. The review of selected studies suggests the potential effectiveness of these digital interventions in addressing psychological factors in asthma management and treatment outcomes. |
The aim of our literature review is to investigate the state of the art of the use of DHIs specifically in relation to the assessment and treatment of psychological dimensions related to asthma, such as stress, anxiety, depression, and coping strategies put in place to counteract the emotional distress that asthma can cause. Furthermore, we evaluate the practicality of employing these innovative technological tools for carrying out observational clinical studies. We also scrutinize the efficacy and implementation of digital self-management aids for both adults and children suffering from asthma.
This review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) for systematic reviews [29], a set of guidelines for reporting systematic reviews and meta-analyses. It enhances transparency, quality, and replicability of reviews, allows easy assessment of the review’s strengths and weaknesses, and promotes compliance with guidelines.
We chose to use a PRISMA diagram over a bibliometrics analysis due to the specific needs and goals of the review. The PRISMA diagram is an excellent tool for mapping out the process of a systematic review or a systematic search, providing a clear and concise visual representation of the number of records identified, included, and excluded, along with the reasons for exclusions. This allows for a transparent and replicable methodology, which is crucial. On the other hand, bibliometrics analysis, while valuable in understanding publication patterns and impacts, does not offer the same level of detail or clarity in the process of a literature review. It is more suited to analyzing the impact of a body of work rather than the process of reviewing it. Therefore, for the purpose of conducting a thorough and transparent literature review, a PRISMA diagram was the more appropriate choice. Additional literature, which is not depicted in the flow diagram, has been derived from full-text articles and is included in the references.
The research question guiding this review was: “In adults and youth with asthma, how does the use of digital technologies for self-management and treatment (such as mobile apps, VR, and wearable technology) compare to traditional asthma management methods in terms of psychological factors (stress, anxiety, and depression) and their impact on asthma?”. This question is framed using the patient, intervention, comparison, outcome (PICO) framework [30] to guide the investigation of the efficacy of digital technologies in addressing psychological and psychopathological factors associated with asthma in both adult and youth populations. Every article included the following criteria: Study population was to be adults and youth with asthma of any sex and socioeconomic status; intervention: Digital technologies for self-management or treatment of asthma-related psychological and psychopathological factors (mobile apps, VR, and wearable technology); some research compared traditional asthma management methods with the ones which included digital technologies; outcome: effectiveness of digital technologies to self-management and/or treatment of psychological and psychopathological factors related to asthma.
From May to June 2023, we conducted several searches on our internal search engine Summon [31] using different search terms combinations. We analyzed articles from the PubMed, PubMed Central, Health & Medical Collection, and Web of Science databases, focusing on results that discussed the relationship between asthma and digital technologies, such as mobile apps, VR, and wearable devices, and their correlation with psychological factors like stress, anxiety, and depression.
The first search was conducted using the terms “asthma” AND (“smartphone applications” OR “mobile apps”) AND (“psychological factors” OR “psychopathological factors”). Out of the 12 papers found, 9 were duplicates and 2 were irrelevant, leaving 1 paper for further analysis.
The second search used the terms “asthma” AND (“smartphone applications” OR “mobile apps”) AND (“stress” OR “anxiety” OR “depression”). Out of the 99 papers found, 68 were duplicates, leaving 3 papers for further analysis.
The third search used the terms “asthma” AND (“virtual reality” OR “video games”) AND (“psychological factors” OR “psychopathological factors”). Out of the 23 papers found, 16 were duplicates, leaving 1 paper for further analysis.
The fourth search used the terms “asthma” AND (“virtual reality” OR “video game”) AND (“stress” OR “anxiety” OR “depression”). Out of the 27 papers found, 15 were duplicates, leaving 1 paper for further analysis.
The fifth search used the terms “asthma” AND (“wearable technology” OR “telemedicine”) AND (“psychological factors” OR “psychopathological factors”). Out of the 24 papers found, 15 were duplicates and none were selected for further analysis.
The sixth and final search used the terms “asthma” AND (“wearable technology” OR “telemedicine”) AND (“stress” OR “anxiety” OR “depression”). Out of the 164 papers found, 104 were duplicates, leaving 2 papers for further analysis.
All the studies published since 2015 were included. There were no limitations based on language. The reference lists of the included studies underwent additional scrutiny to identify additional potential studies. Two authors of the review independently examined and chose studies from the conducted searches.
We included every article that met the following criteria:
All studies and reviews that were published in indexed journals and listed in PubMed, PubMed Central, Health & Medical Collection, and Web of Science databases.
Studies related to digital technologies associated with asthma’s psychological and psychopathological factors, such as stress, anxiety, and depression.
Studies published from 2015 to the present.
We excluded every article meeting the following criteria:
Studies not related to digital technologies associated with asthma’s psychological and psychopathological factors, such as stress, anxiety, and depression.
Studies that focus on the clinical management of asthma, such as pharmacological interventions.
Studies that do not examine the psychological factors associated with the use of digital technologies for asthma.
Studies published in non-scientific or non-peer-reviewed sources.
Studies published prior to 2015.
The two reviewers independently performed data extraction. Any inconsistencies were resolved through discussion or with the assistance of a third reviewer.
The search yielded a total of ten full-text articles, after that eight full-text articles were assessed for eligibility. The term “full-text articles” in the PRISMA diagram represents the number of articles that were deemed potentially relevant after the abstract-level screening and were assessed in detail by reviewing the full text. This is a critical step in the PRISMA process as it ensures that only the most relevant and appropriate studies are included in the final review. The article selection process reported in the PRISMA, compiled in accordance with the guidelines for updates of systematic reviews, can be found in Figure 1. The main characteristics of the included studies are explained below.
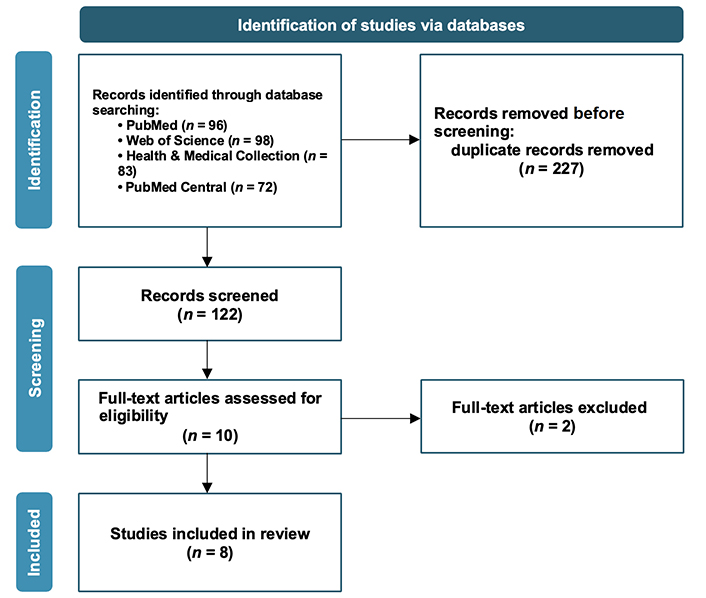
PRISMA flow diagram representing the article selection process in accordance with the guidelines for systematic reviews
Note. Adapted from “The PRISMA 2020 statement: an updated guideline for reporting systematic reviews,” by Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. BMJ. 2021;372:n71 (https://www.bmj.com/content/372/bmj.n71.long). CC BY.
The articles presented in this review investigate the application of eHealth interventions and digital health technologies for the evaluation, treatment, and self-management of psychological and psychopathological aspects associated with asthma in children, adolescents, and young adults. Systematic reviews, reviews, qualitative protocols, participatory studies, and articles are included. The studies were analyzed qualitatively, and the findings were synthesized to provide an overview of the current state of research in this area. A summary of these studies can be found in Table 2 [32–42]. The limitations of the studies and the implications for future research are also discussed.
Summary of studies included in the “Review outcomes” section
| Authors | Year | Type of intervention/tool | Type of paper | Outcome |
|---|---|---|---|---|
| McGar et al. [32] | 2019 | eHealth interventions | Systematic review | Effectiveness of eHealth interventions in improving psychological sequelae in children with medical conditions |
| Thabrew et al. [33] | 2018 | eHealth interventions | Systematic review | Effectiveness of eHealth interventions for managing anxiety and depression in children and adolescents with long-term physical conditions |
| Nichols et al. [34] | 2020 | mHealth intervention | Study protocol | Effectiveness of the mHealth intervention (Managing Asthma and Obesity Related Symptoms; MATADORS) in facilitating symptom self-management among youth with asthma |
| Peters et al. [35] | 2017 | Preferences for an asthma self-management app | Participatory study | Identification of psychological needs and preferences of young individuals for an asthma self-management app |
| Neves et al. [37] | 2021 | Health and fitness mobile apps | Secondary analysis of observational studies | Determinants of the use of health and fitness mobile apps by patients with asthma |
| Dzubur et al. [38] | 2015 | The smartphone app that integrates sensors for asthma inhalers | Letter to the editor | The app can help understand adolescent asthma patients’ real-time experiences, improve treatment adherence, tailor treatments, and enhance patient-provider communication |
| Shah et al. [41] | 2022 | DHIs | Scoping review | DHIs are mostly used for treatment, primarily focus on depression, and are often delivered via web-based platforms. However, their implementation in standard care is limited |
| Sharrad et al. [42] | 2021 | Mixed reality technology | Qualitative protocol | The paper outlines a project to develop and test mixed reality tools for delivering CBT to young people with asthma. The project’s results are not yet available |
In this section, we will review articles that discuss the use of eHealth and mHealth tools for the treatment, management, or self-monitoring of psychological factors related to asthma or similar chronic physical conditions in young people, from children to adolescents.
The first study we examine is the one conducted by McGar et al. [32], which conducted a systematic review of 22 studies that evaluated the efficacy of eHealth interventions designed to prevent or treat psychological sequelae (such as anxiety, depression, posttraumatic stress symptoms (PTSS), and quality of life) in youth with medical conditions and their caregivers. They found mixed but promising results, suggesting that eHealth interventions may help improve psychological and functional outcomes in some pediatric populations, especially those with traumatic brain injury and other potentially traumatic injuries. Among the 22 studies reviewed, three focused on children with persistent asthma. These studies used eHealth interventions that provided self-management education, interactive asthma monitoring, and tailored feedback to improve asthma control and quality of life. The authors reported that these interventions achieved at least one targeted outcome, indicating that eHealth interventions may be useful for enhancing disease management and reducing psychological distress in children with asthma. eHealth interventions have the potential to broaden the reach and accessibility of psychological interventions for children with medical conditions and their caregivers, suggesting that future eHealth interventions should be based on evidence-based theoretical frameworks, such as cognitive behavioral therapy (CBT) or problem-solving therapy, and should be tailored to the specific needs and challenges of each medical population.
Thabrew et al. [33] conducted a systematic review of eHealth interventions for anxiety and depression in children and adolescents with long-term physical conditions, such as asthma. They included five trials of three interventions (Breathe Easier Online, Web-MAP, and multimodal CBT), which involved 463 participants aged 10 to 18 years. They found very low-quality evidence that eHealth interventions were not clearly better than any comparator (such as attention placebo, treatment as usual, or waiting list) in reducing symptoms of anxiety and depression, improving quality of life, functioning, or status of long-term physical condition. They also found very low-quality evidence that eHealth interventions were less acceptable than any comparator. They concluded that the effects of eHealth interventions for this population are uncertain and that more research is needed to develop and evaluate effective and acceptable eHealth interventions. Despite this uncertainty, considering the increasing number of these interventions and the worldwide enhancement in technology accessibility, there seems to be potential for the development and assessment of suitable and effective technology-based treatments tailored for children and adolescents with long-term physical conditions.
Nichols et al. [34] described the development and feasibility testing of a mHealth intervention that aims to improve symptom self-management among youth (ages 10–17) with asthma and obesity. The intervention, called MATADORS, integrates motivational enhancement and behavioral activation (BA) strategies within a family-centric model and a novel mobile app that includes educational content, symptom monitoring, activity tracking, and photo/video/voice diaries. The authors reported the results of a pilot study that randomized 30 youth with asthma and obesity to either MATADORS or a control condition. The intervention group received a six-week nurse-guided mHealth program, while the control group received usual care. The feasibility outcomes included recruitment, reach, adherence, satisfaction, and participant burden. The preliminary outcomes included fatigue, pain, self-efficacy, anxiety, sleep, depression, and quality of life, measured at baseline, 6, and 12 weeks. The authors conclude that MATADORS is a feasible and acceptable intervention that has the potential to improve symptom self-management and quality of life for youth with asthma and obesity. However, they did not report the statistical significance of the preliminary outcomes. Therefore, it is not clear whether MATADORS worked or not in terms of reducing these symptoms and improving these outcomes.
Finally, Peters and colleagues [35] carried out a participatory study to understand the experiences, needs, and ideas of young individuals with asthma. The goal was to identify the requirements for an asthma app that would be engaging and effective in enhancing their well-being. The study included 20 participants aged between 15 and 24 years who filled out a workbook and took part in a workshop, leading to the creation of 102 participant-generated artifacts. The data highlighted that psychological aspects such as anxiety and obstacles to autonomy, competence, and relatedness were viewed by young individuals with asthma as significant influences on their quality of life. The study proposes that an app designed for young individuals with asthma should offer support for mental health factors linked to lived experience, along with practical features for managing asthma. These findings could potentially influence the design of technologies intended to assist people with chronic illnesses more broadly.
Fitness apps can have a profound impact on psychological health by providing several key benefits [36]. They offer motivation and support, helping users set goals, track progress, and receive feedback and encouragement for their physical activity. This can lead to an increase in self-esteem and a sense of accomplishment. Fitness apps also promote engagement and enjoyment by helping users choose the most effective and enjoyable forms of physical activity for their needs, fostering increased engagement and a more positive relationship with exercise. Furthermore, the convenience and accessibility of fitness apps make it easier for users to incorporate regular physical activity into their lives, which can improve mood and reduce symptoms of stress, anxiety, and depression. However, it’s important to note that while fitness apps can contribute to psychological well-being, they are not a substitute for professional mental health care [36].
In this regard, Neves and associates [37] carried out research to evaluate the use of general health and fitness apps among individuals with asthma and to pinpoint the factors that influence their usage. Most of the participants reported having good overall health. However, the occurrence of anxiety and depression was found to be 34.3% and 11.9%, respectively. Roughly 41.1% of the participants reported using health and fitness mobile apps. The research showed that individuals who were single and those with more than 10 years of education were more inclined to use these apps. Moreover, participants with higher digital literacy scores were more likely to use the apps. Interestingly, participants showing symptoms of depression were less likely to use health and fitness apps. The study emphasizes the importance of understanding the obstacles and motivators for app usage among patients with lower education levels, lower digital literacy, or depressive symptoms. This understanding is vital for creating tailored interventions that ensure continued and equitable use of these technologies.
Dzubur et al. [38] discussed the development of a smartphone app that integrates ecological momentary assessment (EMA) and Bluetooth-enabled sensors for asthma inhalers to measure real-time asthma symptoms, social and physical context, behavior, stress, and inhaler use. The effectiveness of long-term asthma management is influenced by behavioral factors such as medication adherence and psychosocial stress. The app was developed by a multidisciplinary team and tested on a small sample of Hispanic middle and high school students. The app used signal-contingent and event-contingent EMA sampling triggered by asthma inhaler use. It prompts users with electronic surveys at random times and after inhaler usage, collecting data on various factors such as positive and negative affect, stress, energy, fatigue, activity type, social and physical contexts, and asthma symptoms.
The app holds promise in aiding researchers and clinicians to gain a deeper understanding of the real-time experiences of teenage asthma patients. It could enhance adherence to treatment plans, customize treatments to meet specific needs, and improve communication between patients and providers. Future research should concentrate on enhancing adherence rates, extending the findings to populations beyond non-Hispanics, and evaluating the health literacy of adolescents.
DHIs are health interventions delivered through digital technologies, such as web-based platforms, mobile apps, or telehealth systems [39]. DHIs may have the potential to improve the mental health of people with asthma, who often experience depression and anxiety as comorbid conditions [40]. In this regard, Shah et al. [41] conducted a scoping review of the literature on DHIs for the prevention, detection, or treatment of depression and anxiety among people with chronic conditions, including asthma. The 53 studies in this review described 36 unique DHIs for prevention (8%), detection (9%), and treatment (83%) of mental health issues in people with chronic conditions. The most common technologies used were web-based platforms (38%) and mobile devices (32%). Most studies focused on depression (68%), with some addressing both depression and anxiety (26%). DHIs typically included education (57%), psychological therapy (53%), and mental health status monitoring (26%). Other components were peer support (17%), communication with healthcare providers (17%), mindfulness (6%), and chat rooms or forums (13%). Most interventions were guided (60%), with guidance provided by various professionals, such as nurses, psychologists, and allied health professionals. Guidance served various functions, including answering questions, providing information, promoting engagement, and monitoring symptoms. The delivery methods for guidance varied, with some using a combination of in-person, phone calls, and text messages. The study revealed that these tailored DHIs have the potential to significantly improve the mental health outcomes of people with asthma, who often suffer from depression and anxiety as comorbid conditions. In particular, stepped-care models showed promise for implementing DHIs into standard care, however, their implementation is still scarce.
A qualitative protocol put forth by Sharrad and colleagues [42] was designed to investigate the potential of utilizing mixed reality tools, including AR, VR, and holographic technology, for delivering CBT to manage symptoms of heightened psychological distress in young individuals with asthma. The success of this protocol is grounded in the application of mixed reality tools such as AR, VR, and holographic technology for delivering evidence-based CBT to young individuals experiencing elevated psychological distress. Mixed reality technologies have the capacity to address low health literacy [43, 44], can be customized based on population characteristics, enhance engagement with content [45], expand the geographic reach and accessibility of information [46], and facilitate real-time content updates. The project plans to employ a qualitative action research framework, moderator guides, and qualitative research to examine the feasibility and acceptability of using mixed reality tools for delivering CBT to manage symptoms of heightened psychological distress in young individuals with asthma. The project would also develop mixed reality-enabled CBT resources and evaluate their acceptability and usability through one-on-one interviews with young people, parents, and health professionals. The data would be scrutinized through three pre-determined perspectives, and the mixed reality resources would be enhanced based on qualitative feedback. Once the project is completed, the data will be compiled for use in publications and conferences, and reports will be shared with participants and relevant stakeholders. The study plans to involve 30 participants, comprising 10 young individuals with asthma, 10 parents of these young individuals, and 10 healthcare professionals. The information gathered from this study would be utilized to refine the mixed reality resources for future feasibility studies, and the objective of the study is to alleviate the impact of asthma by improving access to evidence-based treatments for heightened psychological distress in young individuals with asthma.
The findings of this review highlight the potential of DHIs in addressing psychological factors associated with asthma, in particular in children and adolescents. The included studies demonstrated that eHealth interventions, mixed reality tools, mHealth technology-enhanced nurse-guided interventions, and smartphone apps integrating EMA and Bluetooth-enabled sensors for asthma inhalers can significantly improve symptom self-management, quality of life, and mental health outcomes in this population [32–35, 37, 38, 41, 42]. However, it is important to note that the field of DHIs for the treatment of anxiety or depression with long-term physical conditions, including asthma, is still limited. Further research is needed to determine the effectiveness and feasibility of these interventions in diverse populations and settings [38]. Tailored interventions that address the specific needs and preferences of patients with asthma and associated psychological factors are crucial for ensuring sustained and equitable use of these technologies [38]. Future studies should focus on improving methodological rigor, generalizability, and long-term outcomes, as well as addressing concerns about accessibility, privacy, and data security. The development of personalized interventions and the integration of digital health technologies into routine clinical care have the potential to make a substantial difference in public health for individuals living with chronic conditions, including asthma.
We, the authors, have been working in the psychological and psychotherapeutic field for years, and we know well how psychological and psychopathological factors such as anxiety and depression, for example, can reduce people’s quality of life. The increasingly comprehensive use of new technologies opens so many doors, and the creation of treatment programs for such factors when they are in comorbidity with asthma is certainly an unfortunately under-explored field, but one of great social and health impact. The presence of a few studies in this review is indicative of just that: We know that asthma, like other chronic conditions, causes discomfort in people, discomfort that can turn into real psychopathological disorders. Our goal with this review is therefore at least to pose the question to the scientific community, highlighting what is available for consultation at the time of writing. We hope that this will increase the interest and development, as well as the application, of the new technologies available in digital health to reduce the impact that negative psychological factors can have on people with asthma.
The reviewed articles provide insights into DHIs for managing asthma and related psychological factors, but limitations exist. The scope of the review is limited to a specific set of studies, due to the scarcity of studies available in the literature on the specific topic of DHIs for managing asthma and associated psychological factors. The effectiveness of these interventions may vary across populations and settings, and their personalization needs further investigation. The review doesn’t address technological challenges in adopting these interventions, nor does it consider ethical, privacy, and data security issues. Further research is needed to address these limitations and advance the understanding of DHIs in asthma management.
In conclusion, DHIs hold the promise to enhance the management of asthma and related psychological aspects in children and adolescents. The studies reviewed in this article suggest that eHealth interventions, mixed reality tools, mHealth technology-enhanced nurse-guided interventions, and smartphone apps integrating EMA and Bluetooth-enabled sensors for asthma inhalers can significantly improve symptom self-management, quality of life, and mental health outcomes [32–35, 37, 38, 41, 42]. However, the field of DHIs for the treatment of anxiety or depression in children and adolescents with long-term physical conditions is limited, and further research is needed to determine their effectiveness and feasibility in different populations and settings. The development of tailored interventions that address the specific needs and preferences of patients with asthma and associated psychological factors is crucial for ensuring sustained and equitable use of these technologies. Future studies should focus on improving methodological rigor, generalizability, and long-term outcomes, as well as addressing concerns about accessibility, privacy, and data security. In essence, DHIs have the potential to make a substantial difference in public health for individuals living with chronic conditions, including asthma. These interventions warrant further exploration and development to enhance patient outcomes and quality of life.
apps: applications
AR: augmented reality
CBT: cognitive behavioral therapy
DHIs: digital health interventions
eHealth: electronic health
EMA: ecological momentary assessment
MATADORS: Managing Asthma and Obesity Related Symptoms
mHealth: mobile health
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses
VR: virtual reality
MC: Conceptualization, Investigation, Writing—original draft, Writing—review & editing. PC: Conceptualization, Validation, Investigation, Supervision, Writing—original draft, Writing—review & editing. Both authors read and approved the submitted version.
The authors declare that they have no conflicts of interest.
Not applicable.
Not applicable.
Not applicable.
Not applicable.
Not applicable.
© The Author(s) 2024.
Copyright: © The Author(s) 2024. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Deborah A. Fisher ... Ted R. Miller
Mehr Muhammad Adeel Riaz ... Faisal A. Nawaz
