Affiliation:
1Carolinas Rehabilitation-Mountain Island Lake, Atrium Health, Charlotte, NC 28203, USA
Email: Andrew.Ball@atriumhealth.org
ORCID: https://orcid.org/0000-0002-0888-5363
Affiliation:
2Continuing Professional Development, South Piedmont Area Health Education Center, Charlotte, NC 28208, USA
ORCID: https://orcid.org/0009-0004-3537-3189
Affiliation:
1Carolinas Rehabilitation-Mountain Island Lake, Atrium Health, Charlotte, NC 28203, USA
ORCID: https://orcid.org/0009-0000-8469-8124
Affiliation:
1Carolinas Rehabilitation-Mountain Island Lake, Atrium Health, Charlotte, NC 28203, USA
ORCID: https://orcid.org/0009-0009-4409-6781
Affiliation:
3Rehabilitation Services, Novant Health, Charlotte, NC 28204, USA
ORCID: https://orcid.org/0000-0001-9979-6130
Affiliation:
1Carolinas Rehabilitation-Mountain Island Lake, Atrium Health, Charlotte, NC 28203, USA
ORCID: https://orcid.org/0000-0002-5631-4450
Explor Musculoskeletal Dis. 2024;2:49–55 DOI: https://doi.org/10.37349/emd.2024.00033
Received: November 17, 2023 Accepted: December 16, 2023 Published: February 05, 2024
Academic Editor: Nicusor V. Iftimia, Physical Sciences Inc., USA
Upon self-reflection, some clinicians privately confess a lack of confidence in being able to safely perform trigger point dry needling (TrPDN) or trigger point injection (TrPI) on craniofacial muscles. Procedural performance anxiety seems to be more pronounced relative to those muscles that cannot be palpated and/or have an increased risk of iatrogenic injury to neurovascular structures. Participatory action ultrasound imaging (PAUI) can be a useful tool in enhancing clinician confidence. A clinician-subject with a left lateral pterygoid trigger point was dry-needled under ultrasound guidance by a clinician-needler with extensive training and experience relative to evaluation and treatment of patients with craniofacial pain. Prior to PAUI, both the clinician-needler and clinician-observer describe low-to-moderate anxiety in the performance of TrPDN of the lateral pterygoid, using a lateral-to-medial approach. By contrast, both the clinician-needler and clinician-observer expressed high anxiety, objectively confirmed by the state-trait anxiety inventory (STAI) form Y-1 (STAI Y-1), in the performance of a newly learned cephalo-caudal approach. Following an initial round of clinical training without PAUI, subjective anxiety remained high despite a lower theoretical risk to the maxillary artery using the cepalo-caudal approach. A second round of training was performed with the addition of PAUI; the clinician-needler was able to reach the target tissue within 2 min in each of 3 attempts. Upon visual inspection and interpretation of the images and cine, the clinician-needler and clinician-observer both expressed a “significant” decrease in self-reported anxiety in performing the cephalo-caudal approach, objectively verified by improvements in the STAI Y-1 score of both clinicians. This case report presents PAUI as a means for future research and clinician education regarding risk assessment of TrPDN or TrPI of muscles with risk of iatrogenic injury.
Direct palpation and manual treatment of the lateral pterygoid muscle (particularly the inferior head) is clinically controversial in that several authors claim that it is not possible due to the deep anatomical orientation of the muscle largely covered by bone [1, 2]. Several authors have described trigger point dry needling (TrPDN) techniques of the lateral pterygoid with favorable results [3, 4], as well as cadaverous validation of dry needling into the superior and inferior heads respectively [5]. Although TrPDN and trigger point injection (TrPI) have relatively sound safety profiles, serious iatrogenic complications have been known to occur [6–10]. As such, some dry-needling clinicians privately admit to more experienced dry-needling colleagues, a lack of confidence in attempting TrPDN (more typically used by doctors of physical therapy and chiropractic) or TrPI (more typically used by dentists and medical physicians) in using newly learned needling approaches in the treatment of craniofacial pain where the target tissue cannot be directly palpated or the needle placement into target tissue cannot be easily verified. Procedural performance anxiety may lead to clinical self-censorship and resultant procedural underutilization of the technique on patients appropriate for receiving it—theoretically resulting in procedural underutilization and less effective and/or less efficient outcomes.
Participatory action research (PAR) [11], a novel research tool that includes the subject as an active participant in the research process for the purposes of enhancing skill and confidence [12], was used to educate the clinician-subjects on the procedural risks of dry needling the lateral pterygoid with an over-the-zygomaticus cephalo-caudal technique. Combined with pre-existing skill validation and certification, as well as pre-existing knowledge of the literature regarding the incidence of iatrogenic injury from TrPDN or TrPI [12, 13], PAR in the form of visual observation of technique parameters [defined in this case report as “participatory action ultrasound imaging (PAUI)”] proved a useful tool in enhancing clinician confidence.
A 5 feet 5 inch, 140 pound, 51 year-old male dry-needling certified clinician-instructor with 10 years of experience as an ultrasound sonologist, nearly 30 years of experience as a physical therapist, and with a left lateral pterygoid trigger point (clinician-instructor), was dry-needled under ultrasound guidance by a trigger-point certified doctor of physical therapy with 17 years of clinical experience and extensive training and instructional experience relative to the evaluation and treatment of patients with craniofacial pain (clinician-needler). An additional trigger-point certified doctor of physical therapy with 10 years of experience and extensive training relative to the evaluation and treatment of patients with craniofacial pain observed the procedure (clinician-observer).
The clinician-needler and clinician-observer in this case study were both trained, tested, and comfortable with dry needling of the lateral pterygoid using a lateral-to-medial approach theoretically biasing the inferior head of the muscle (described as inserting the needle “below the zygomatic process just between the mandibular condyle and the coronoid process. The needle is advanced from anterior to posterior in an upward direction with an angle of 15 degrees to the anterior border of the mandibular process” [5]) (Figure 1). The authors of this paper find this description somewhat awkward, describing the needle advancement as anterior-to-posterior rather than lateral-to-medial, the latter of which will be used to describe the approach throughout the remainder of this article. Dry needling using a lateral-to-medial needle advancement seems to be a commonly utilized approach among dry needling clinicians that treat craniofacial pain in the United States.
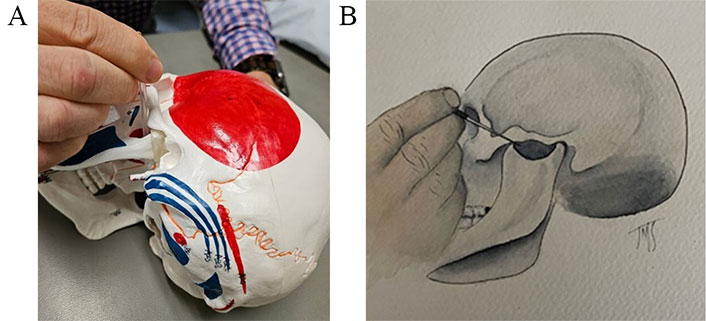
Lateral-to-medial approach in TrPDN/TrPI of the lateral pterygoid. (A) Model demonstration; (B) artist rendering
The cephalo-caudal approach is (in the opinion of the authors) less frequently utilized as it is not as commonly taught in continuing education courses despite its theoretically more favorable safety profile with respect to possible iatrogenic injury to the maxillary artery. When dry needling using this approach (theoretically biasing the superior head of the muscle), “the needle should be inserted over the zygomatic process just posterior at the obituary arch. The needle is advanced from an anterior to posterior direction with an angle of 45 with the horizontal and from a lateral to medial direction with an angle of 15 to the anterior border of the temporomandibular joint” [5] (Figure 2).
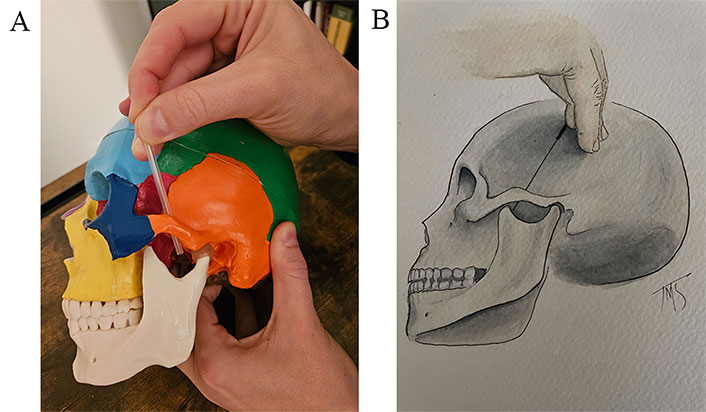
Cephalo-caudal approach in TrPDN/TrPI of the lateral pterygoid. (A) Model demonstration; (B) artist rendering
Both the dry needling and observing clinicians reported low to moderate anxiety in the performance of a previously learned lateral-to-medial approach (anterior to the mandibular condyle and superior to the mandibular notch needling superficial-to-deep into the lateral pterygoid muscle) versus high anxiety, objectively confirmed by the state-trait anxiety inventory (STAI) form Y-1 (STAI Y-1) [13, 14], in the performance of a newly learned cephalo-caudal approach (initially taught without the benefit of PAUI). The STAI is a psychological inventory based on a 4-point Likert scale and consists of 40 questions on a self-report basis. The STAI measures two types of anxiety. Form Y-1 measures state anxiety (anxiety about an event), and form Y-2 measures trait anxiety measures, or anxiety level as a personal characteristic [14]. Incidentally, although the clinician-needler self-described as high-anxiety as a personality trait, the STAI Y-2 scores of the clinician-needler and clinician observer (scores of 34 and 37 respectively) are both interpreted as “no to low overall anxiety” and did not objectively support the subjective claim.
Following an initial round of technique training, subjective anxiety regarding the performance of the nearly learned cephalo-caudal approach remained high despite a much lower theoretical risk to the maxillary artery versus the lateral-to-medial approach. A second round of training was performed with the addition of PAUI to determine how clinician-needler and clinician-observer confidence might change through real-time ultrasound imaging visual inspection and education regarding needle placement during the cephalo-caudal approach. The patient-subject was placed in side-lying and the lateral pterygoid was imaged with a genderal electric (GE) Voluson ultrasound system with a 12Linear-Remote Sensor (12L-RS) linear probe at 13 megahertz (MHz) frequency.
Upon visual inspection and interpretation of the image and cine/video by the clinician-instructor with the clinician-needler and clinician-observer (e.g., PAUI), clinical confidence subjectively improved on the part of both clinician-learners. Of note, the 60 mm (or 2.36 inch) long dry needle used during PAUI not only traversed the targeted superior head of the lateral pterygoid but safely reached the inferior head of the lateral pterygoid as well. Following PAUI, both the clinician-needler and clinician-observer not only reported a “significant” decrease in self-reported anxiety in performing the cephalo-caudal approach, but STAI Y-1 scores improved as well [from 63 and 62 respectively to improvement to minimal anxiety (score of 38) in the case of the more experienced clinician-needler, and even greater improvement to slight anxiety (score of 28) in the case of the less experienced clinician-observer].
This case report presents a previously undescribed means of using PAUI for clinician education regarding TrPDN, TrPI, or acupuncture of muscles with a risk of iatrogenic injury to neurovascular structures where the muscle cannot be directly palpated (Figure 3). Studies have shown that ultrasound imaging for procedural guidance enhances clinician skill and confidence [15–17]. Studies describing clinician safety and skill with the procedural aspects of TrPDN or TrPI have examined patient positioning [18], the accuracy of rib palpation and needling of muscles requiring intercostal blocking [17, 19], adverse event incidence [6–10], but not the needling of muscles with risk of iatrogenic injury to neurovascular structures where the muscle cannot be directly palpated. More study is needed to investigate how variation in patient anatomy influences the achievement of advancing the dry needle to target tissue, as well as how the learner’s confidence with the anatomical specifics of the target tissue influences the procedural learning process. It is proposed hope that future research on clinician education and training consider the use of PAUI to further explore its value in the clinical education and training process, particularly with respect to invasive procedures such as TrPDN and TrPI.
A potential limitation of this case study is that the clinician-needler performed the technique on a clinician-instructor who was both calm and encouraging during the process. The improvements in procedural confidence may not be reproducible when guided by a colleague of less clinical/procedural skill, teaching experience, education, and/or confidence. Furthermore, upon post-learning participatory action review of the STAI Y-1 results, it was noted that the more experienced clinician (clinician-needler), did not experience the same level of decreased anxiety as the less experienced clinician (clinician-observer). The impact of overall anxiety as a personality trait versus or combined with anxiety regarding the performance of a specific clinical procedure is not known. In addition, as a case report, the reader should take caution not to over-generalize the findings. Future research should consider comparing larger cohorts in the assessment of the relative value of PAUI in novice clinicians versus experienced clinicians, in tech-comfortable clinicians versus tech-resistant clinicians, and in clinicians with overall high-anxiety versus low.
Although more study is required to determine the impact of variation of anatomical variation, and patient-to-clinician encouragement upon both safety and clinician confidence, PAUI proved a valuable tool in clinician confidence when learning a new approach to TrPDN or TrPI of the lateral pterygoid. Additionally, although the theoretical risk of iatrogenic injury to the maxillary artery is exceedingly small during TrPDN or TrPI of the lateral pterygoid, it is still theoretically possible when using a lateral-to-medial technique. Given the theoretically more favorable safety profile of TrPDN or TrPI of the cephalo-caudal approach, as well as the demonstrated ability to reach not only the superior head of the lateral pterygoid, but the inferior head as well, clinicians using TrPDN or TrPI in their clinical practice may wish to consider first approaching the lateral pterygoid cephalo-caudally, and employing the lateral-to-medial approach ad-hoc only when success is not realized with the cephalo-caudal approach. As demonstrated in this case report, participatory action imaging as an educational tool may have a significant impact on clinician confidence in performing TrPDN and TrPI in instances where target tissue cannot be palpated and a risk of iatrogenic injury to a neurovascular structure exists. Ideally, improved clinician confidence should result in a decrease in under-utilization of TrPDN/TrPI of the lateral pterygoid and facilitate safe and judicious application of the cephalo-caudal approach to all appropriate patient candidates.
In conclusion, PAUI is a valuable tool in demonstrating to clinician-subjects the low procedural risk of TrPDN/TrPI, particularly in muscles where target tissue cannot be palpated and risk of iatrogenic injury to a neurovascular structure is theoretically higher. Future study is required to determine meaningful shifts in, and minimal standards of, clinician-subject confidence for the safe patient application of TrPDN/TrPI on muscles that cannot be easily, if at all, palpated.
PAUI: participatory action ultrasound imaging
STAI: state-trait anxiety inventory
TrPDN: trigger point dry needling
TrPI: trigger point injection
AB: Conceptualization, Investigation, Writing—original draft, Writing—review & editing. SL and SB: Investigation, Writing—review & editing. DM and EB: Writing—review & editing. JS: Visualization, Writing—review & editing. All authors read and approved the submitted version.
The author declares that there are no conflicts of interest.
Although case reports do not require Atrium Health Wake Forest Baptist Review Board (IRB) oversight, Atrium Health IRB associate director and research privacy officer reviewed manuscript for compliance with HIPAA and ethical compliance. All investigating authors/participants are good clinical practice (GCP) certified by the collaborative institutional training initiative (CITI Program) for human subject research, ethics compliance and safety training.
The informed consent to participate in the study was obtained from all participants.
Not applicable.
Not applicable.
Not applicable.
© The Author(s) 2024.
Copyright: © The Author(s) 2024. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 4965
Download: 27
Times Cited: 0
